Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 26(3); 2013 > Article
-
Original Article
- Minimally Invasive Plate Osteosynthesis with Locking Compression Plate for Distal Femur Fracture
- Sung Won Cho, M.D., Sang Ho Ha, M.D., Gwang Chul Lee, M.D., Woong Hee Kim, M.D.
-
Journal of the Korean Fracture Society 2013;26(3):205-211.
DOI: https://doi.org/10.12671/jkfs.2013.26.3.205
Published online: July 15, 2013
Department of Orthopaedic Surgery, School of Medicine, Chosun University, Gwangju, Korea.
- Address reprint requests to: Sang Ho Ha, M.D. Department of Orthopaedic Surgery, Chosun University Hospital, 365 Pilmun-daero, Dong-gu, Gwangju 501-717, Korea. Tel: 82-62-220-3147, Fax: 82-62-226-3379, shha@chosun.ac.kr
Copyright © 2013 The Korean Fracture Society. All rights reserved.
This is anOpen Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 742 Views
- 1 Download
- 2 Crossref
Abstract
-
Purpose
- To analyze the clinical and radiologic results of minimally invasive plate osteosynthesis (MIPO) for distal femur fractures using a locking compression plate (LCP) and to evaluate its usefulness.
-
Materials and Methods
- From May 2006 to April 2011, 23 patients (24 cases) with distal femur fracture were treated by MIPO with a LCP and followed-up for at least 12 months. Mean age was 61.6 years (35-80 years). Union time and post-operative alignment were measured on radiograph, and clinical function was evaluated by range of motion (ROM), Knee Society Score and complications.
-
Results
- In 22 patients (23 cases) except for 1 case, bony union was obtained after an average of 18 weeks (12-26 weeks). The mean ROM was 124 degrees (80-135 degrees). According to the Knee Society Score, there were 12 excellent, 8 good, 1 fair and 2 poor results and the mean score was 87.5 (60-98). Postoperative complications were nonunion in 1 case, ankylosis in 1 case, malunion in 2 cases and superficial wound infection in 2 cases.
-
Conclusion
- The treatment of distal femoral fracture with MIPO using a LCP was considered a useful method which can result in satisfactory clinical and radiologic outcomes if there is accurate understanding about the surgical techniques and appropriate procedures involved.
- 1. Button G, Wolinsky P, Hak D. Failure of less invasive stabilization system plates in the distal femur: a report of four cases. J Orthop Trauma, 2004;18:565-570.
- 2. Davison BL. Varus collapse of comminuted distal femur fractures after open reduction and internal fixation with a lateral condylar buttress plate. Am J Orthop (Belle Mead NJ), 2003;32:27-30.
- 3. Ehlinger M, Adam P, Abane L, Arlettaz Y, Bonnomet F. Minimally-invasive internal fixation of extra-articular distal femur fractures using a locking plate: tricks of the trade. Orthop Traumatol Surg Res, 2011;97:201-205.
- 4. Ehlinger M, Adam P, Arlettaz Y, et al. Minimally-invasive fixation of distal extra-articular femur fractures with locking plates: limitations and failures. Orthop Traumatol Surg Res, 2011;97:668-674.
- 5. Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur Less Invasive Stabilization System (LISS). Injury, 2001;32:Suppl 3. SC24-SC31.
- 6. Giles JB, DeLee JC, Heckman JD, Keever JE. Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw. J Bone Joint Surg Am, 1982;64:864-870.
- 7. Han SB, Choi IC, Lee SH, Suh DH, Cho HJ. Minimal invasive plate osteosynthesis for distal femoral fracture. J Korean Fract Soc, 2006;19:11-16.
- 8. Janzing HM, Stockman B, Van Damme G, Rommens P, Broos PL. The retrograde intramedullary nail: prospective experience in patients older than sixty-five years. J Orthop Trauma, 1998;12:330-333.
- 9. Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma, 2004;18:509-520.
- 10. Kregor PJ, Stannard J, Zlowodzki M, Cole PA, Alonso J. Distal femoral fracture fixation utilizing the Less Invasive Stabilization System (L.I.S.S.): the technique and early results. Injury, 2001;32:Suppl 3. SC32-SC47.
- 11. Krettek C, Müller M, Miclau T. Evolution of minimally invasive plate osteosynthesis (MIPO) in the femur. Injury, 2001;32:Suppl 3. SC14-SC23.
- 12. Krettek C, Schandelmaier P, Miclau T, Bertram R, Holmes W, Tscherne H. Transarticular joint reconstruction and indirect plate osteosynthesis for complex distal supracondylar femoral fractures. Injury, 1997;28:Suppl 1. A31-A41.
- 13. Mize RD. Surgical management of complex fractures of the distal femur. Clin Orthop Relat Res, 1989;(240):77-86.
- 14. Park KC, Chung KS, Moon JK. Treatment of distal femur fracture with minimally invasive locking compression plate osteosynthesis. J Korean Fract Soc, 2012;25:13-19.
- 15. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br, 2002;84:1093-1110.
- 16. Schatzker J. Fractures of the distal femur revisited. Clin Orthop Relat Res, 1998;(347):43-56.
- 17. Schatzker J, Home G, Waddell J. The Toronto experience with the supracondylar fracture of the femur, 1966-72. Injury, 1974;6:113-128.
- 18. Schütz M, Müller M, Krettek C, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury, 2001;32:Suppl 3. SC48-SC54.
- 19. Siliski JM, Mahring M, Hofer HP. Supracondylar-intercondylar fractures of the femur. Treatment by internal fixation. J Bone Joint Surg Am, 1989;71:95-104.
- 20. Wagner M. General principles for the clinical use of the LCP. Injury, 2003;34:Suppl 2. B31-B42.
- 21. Zlowodzki M, Bhandari M, Marek DJ, Cole PA, Kregor PJ. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005). J Orthop Trauma, 2006;20:366-371.
REFERENCES
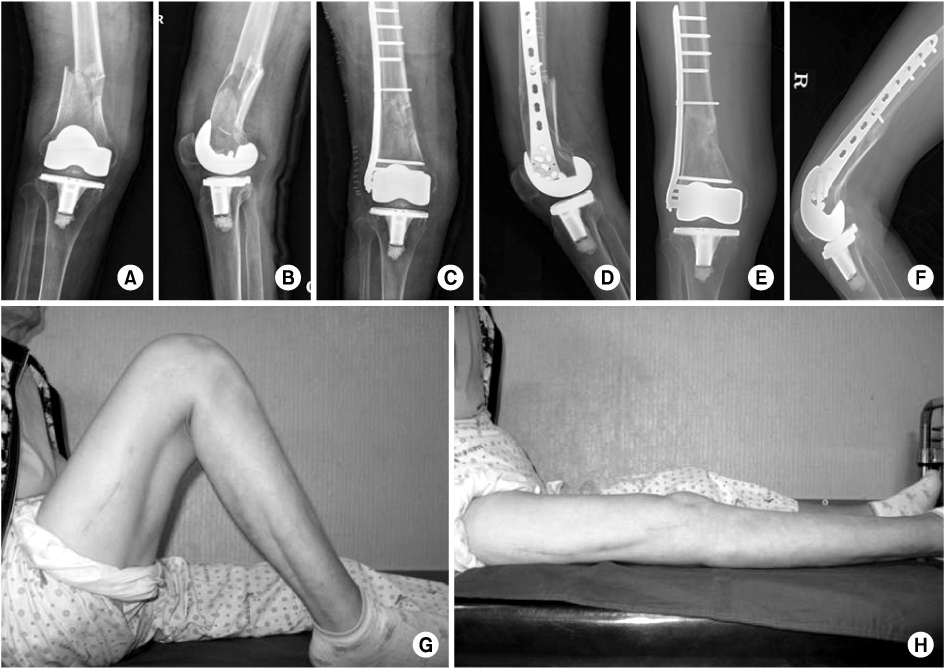
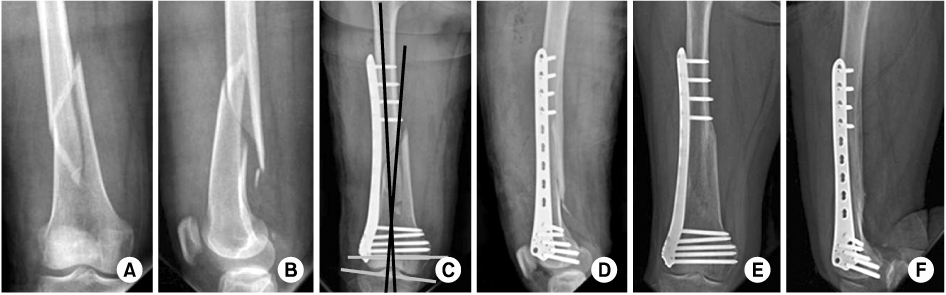
Figure & Data
REFERENCES
Citations

- Surgical Treatment of AO/OTA 33-C Intra-Articular Distal Femoral Fractures through Parapatellar Approach
Suk Kyu Choo, Sung Tan Cho, Hyoung Keun Oh
Journal of the Korean Fracture Society.2022; 35(1): 1. CrossRef - Incidence of nonunion after surgery of distal femoral fractures using contemporary fixation device: a meta‐analysis
Byung-Ho Yoon, In Keun Park, Youngwoo Kim, Hyoung-Keun Oh, Suk Kyu Choo, Yerl-Bo Sung
Archives of Orthopaedic and Trauma Surgery.2021; 141(2): 225. CrossRef

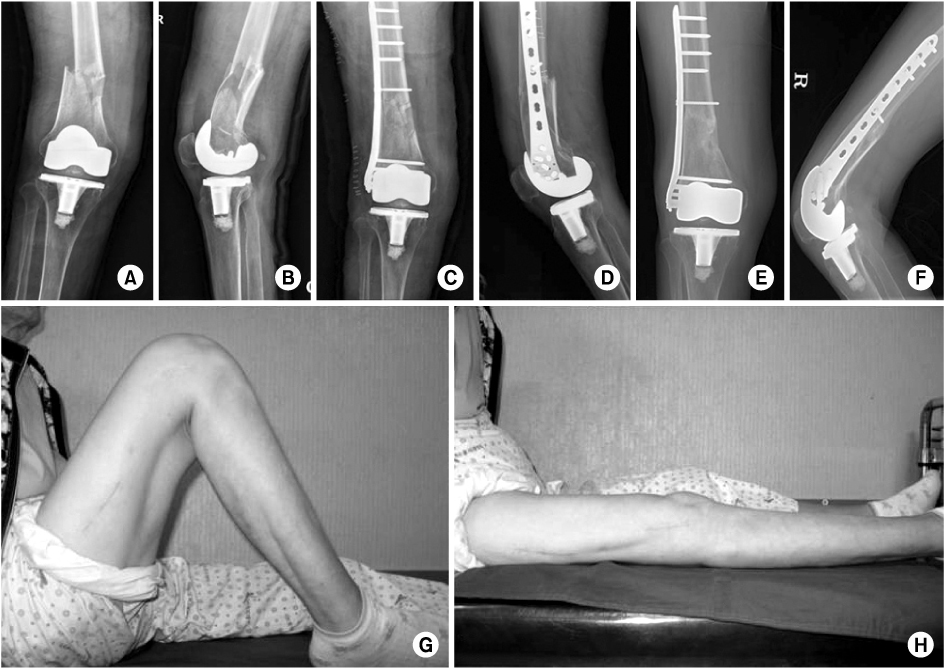
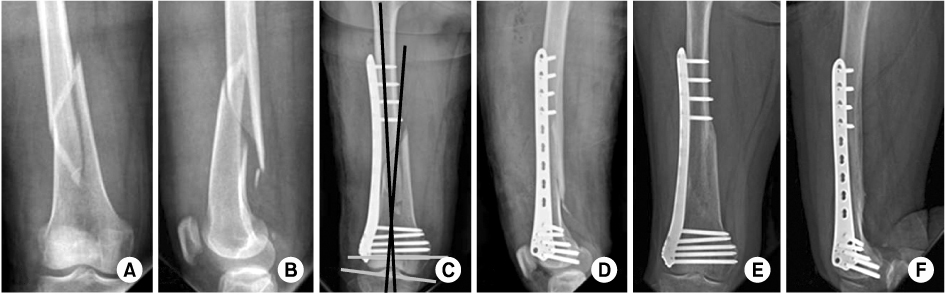
Fig. 1
Fig. 2
Fig. 3
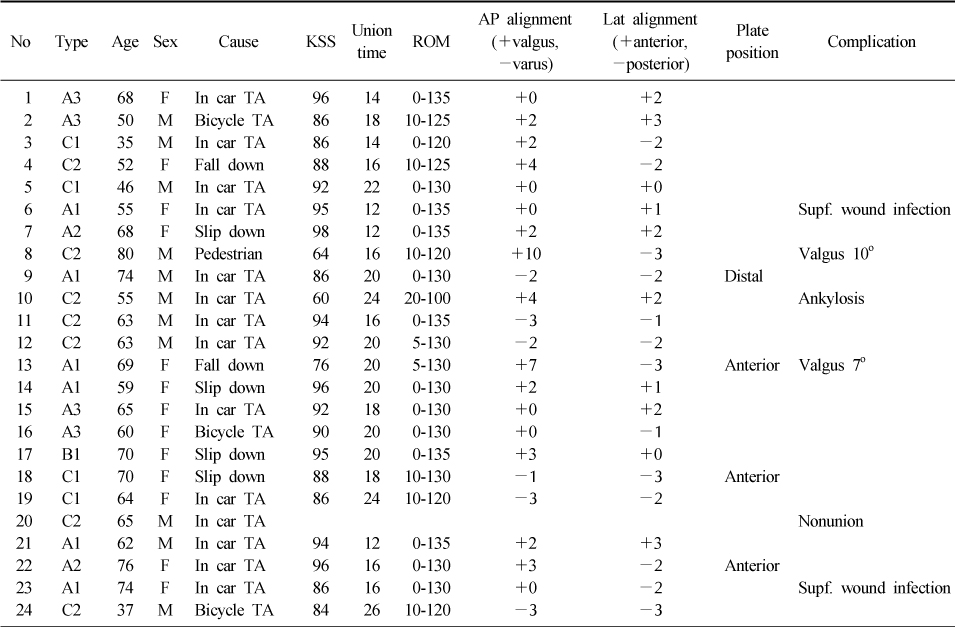
Patient Demographics, Clinical and Radiographic Outcomes
KSS: Knee society score, ROM: Range of motion, AP: Anteriorposterior, Lat: Lateral, F: Female, M: Male, TA: Traffic accident, Supf.: Superficial.
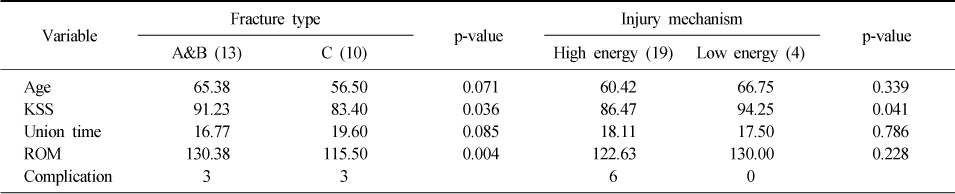
Comparison of Clinical Outcomes
KSS: Knee society score, ROM: Range of motion.
KSS: Knee society score, ROM: Range of motion, AP: Anteriorposterior, Lat: Lateral, F: Female, M: Male, TA: Traffic accident, Supf.: Superficial.
KSS: Knee society score, ROM: Range of motion.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

