Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 22(1); 2009 > Article
-
Review Article
- Correction of Malalignment during Subtrochanteric Nailing
- Kyu Hyun Yang, M.D.
-
Journal of the Korean Fracture Society 2009;22(1):66-70.
DOI: https://doi.org/10.12671/jkfs.2009.22.1.66
Published online: January 31, 2009
Department of Orthopaedic Surgery, Gangnam Severance Hospital, College of Medicine, Yonsei University, Seoul, Korea.
- Address reprint requests to: Kyu Hyun Yang, M.D. Department of Orthopaedic Surgery, Gangnam Severance Hospital, College of Medicine, Yonsei University, 146-92, Dokok-dong, Gannam-gu, Seoul 135-720, Korea. Tel: 82-2-2019-3414, Fax: 82-2-573-5393, kyang@yuhs.ac
Copyright © 2014 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 578 Views
- 6 Download
- 3 Crossref
- 1. Brownner BD, Brown CM. Locked nailing of femoral fractures. In: Browner BD, editor. The science and practice of intramedullary nailing. Baltimore: Lippincott Williams & Willins; 1996. p. 161-181.
- 2. Carr JB. The anterior and medial reduction of intertrochanteric fractures: a simple method to obtain a stable reduction. J Orthop Trauma, 2007;21:485-489.
- 3. French BG, Tornetta P 3rd. Use of an interlocked cephalomedullary nail for subtrochanteric fracture stabilization. Clin Orthop Relat Res, 1998;348:95-100.
- 4. Gugenheim JJ, Probe RA, Brinker MR. The effects of femoral shaft malrotation on lower extremity anatomy. J Orthop Trauma, 2004;18:658-664.
- 5. Kempf I, Grosse A, Beck G. Closed locked intramedullary nailing. Its application to comminuted fractures of the femur. J Bone Joint Surg Am, 1985;67:709-720.
- 6. Liu HT, Wang IC, Yu CM, et al. Closed femoral nailing in lateral decubitus position without a fracture table: a preliminary report of fifteen patients. Chang Gung Med J, 2005;28:629-635.
- 7. Russell TA, Mir HR, Stoneback J, Cohen J, Downs B. Avoidance of malreduction of proximal femoral shaft fractures with the use of a minimally invasive nail insertion technique (MINIT). J Orthop Trauma, 2008;22:391-398.
- 8. Tornetta P 3rd, Ritz G, Kantor A. Femoral torsion after interlocked nailing of unstable femoral fractures. J Trauma, 1995;38:213-219.
- 9. Tornetta P 3rd, Tiburzi D. Antegrade or retrograde reamed femoral nailing. A prospective, randomised trial. J Bone Joint Surg Br, 2000;82:652-654.
- 10. Winquist RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am, 1984;66:529-539.
- 11. Wolinsky P, Tejwani N, Richmond JH, Koval KJ, Egol K, Stephen DJ. Controversies in intramedullary nailing of femoral shaft fractures. Instr Course Lect, 2002;51:291-303.
REFERENCES
Fig. 1Nail insertion with uncorrected external rotation and flexion displacement of the proximal fragment results in varus and flexion deformity.


Fig. 2Malalignment correction is performed by insertion and elevation of a long tonsil hemostat from lateral aspect of the proximal thigh.


Fig. 3External rotation and abduction deformity of the proximal fragment is corrected by elevating the handle of the forceps toward the anterior aspect of the thigh using a curved tip placed at the lesser trochanter as a fulcrum, which is followed by advancing a straight guide wire through the proper entry point.


Fig. 4Flexion deformity (C) of the proximal fragment that remained even after correction of external rotation deformity with one hemostatic forceps (A, B), is further corrected by placing additional forceps more distal to the previously inserted forceps in a similar manner, finally followed by advancing a straight guide wire in a well reduced position (D).
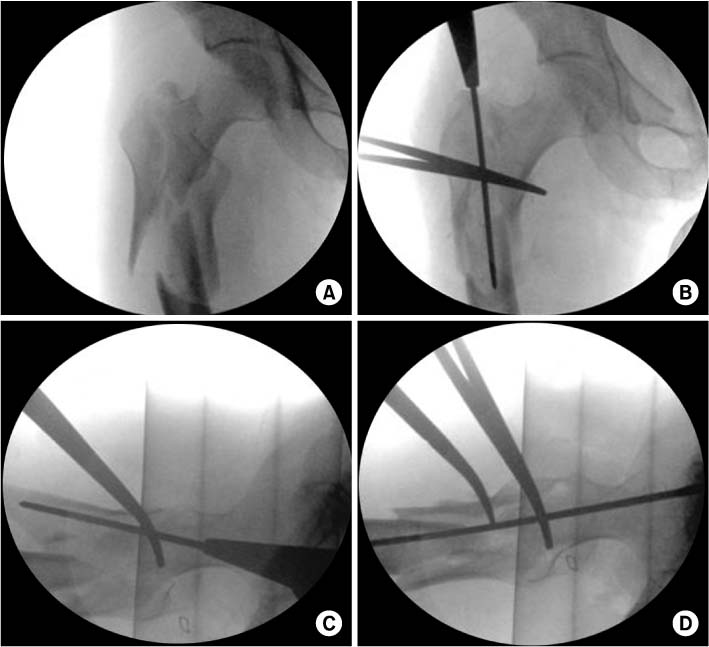
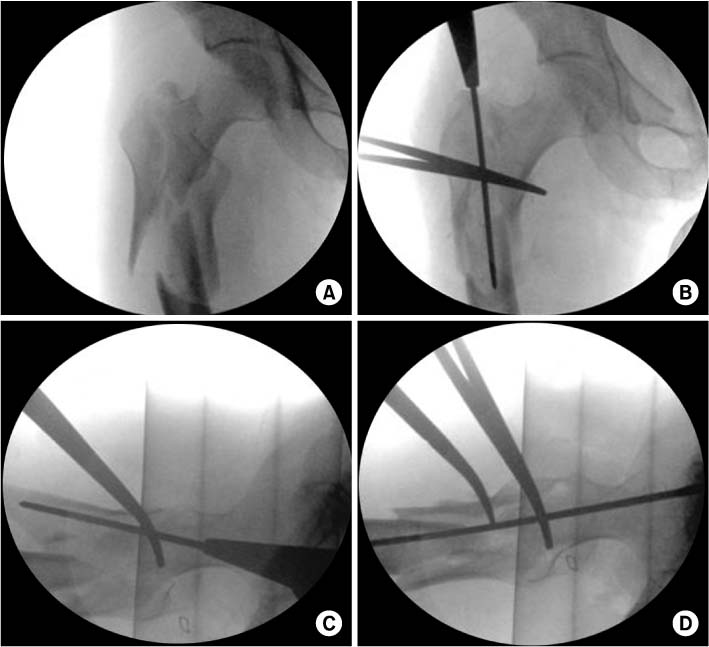
Fig. 5Both hemostatic forceps are maintained in place (A) until the lag screw guide pin is placed in the proper position of the femoral head (C, D) to prevent recurrence of flexion deformity. With the distal interlocking holes circular (arrow) and posterior margins of both femoral condyles exactly overlapped in the lateral view (B), nail geometry can be used to get a correct rotational alignment (femoral anteversion of 15° in this case).


Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Subtrochanteric Fracture Reduction during Intramedullary Nailing: Technical Note
Gyu Min Kong
Journal of the Korean Fracture Society.2019; 32(2): 107. CrossRef - Treatment of Femur Subtrochanteric Fracture Using the Intramedullary Long Nail; Comparison of Closed Reduction and Minimal Open Reduction
Sang Joon Lee, Sang Hong Lee, Sang Soo Park, Hyung Seok Park
Journal of the Korean Orthopaedic Association.2015; 50(1): 18. CrossRef - Surgical Treatment of Femur Intertrochanteric and Subtrochanteric Fracture
Jong-Oh Kim, Tae-Ho Kim
Hip & Pelvis.2010; 22(1): 1. CrossRef
Correction of Malalignment during Subtrochanteric Nailing



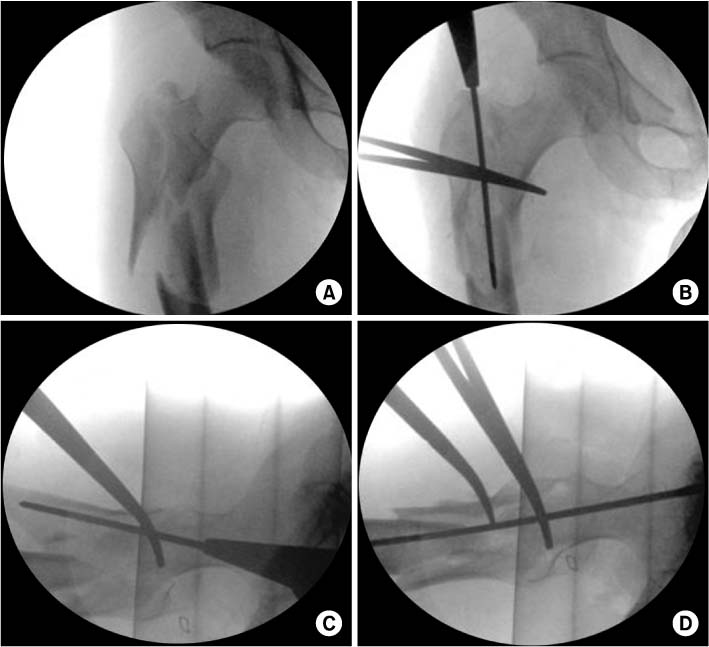
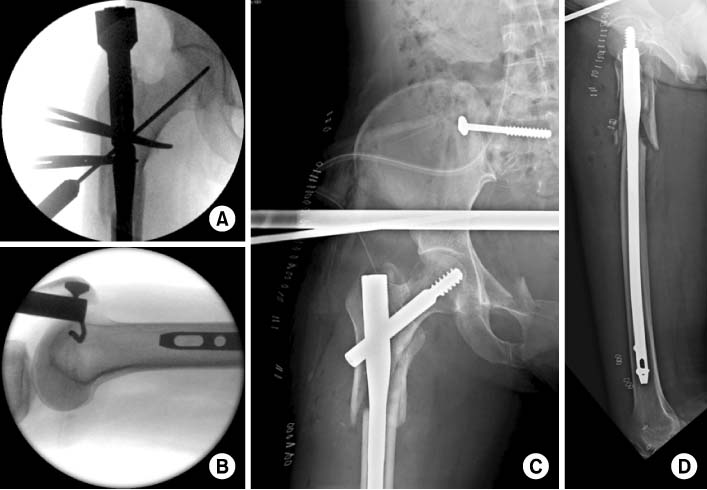
Fig. 1
Nail insertion with uncorrected external rotation and flexion displacement of the proximal fragment results in varus and flexion deformity.
Fig. 2
Malalignment correction is performed by insertion and elevation of a long tonsil hemostat from lateral aspect of the proximal thigh.
Fig. 3
External rotation and abduction deformity of the proximal fragment is corrected by elevating the handle of the forceps toward the anterior aspect of the thigh using a curved tip placed at the lesser trochanter as a fulcrum, which is followed by advancing a straight guide wire through the proper entry point.
Fig. 4
Flexion deformity (C) of the proximal fragment that remained even after correction of external rotation deformity with one hemostatic forceps (A, B), is further corrected by placing additional forceps more distal to the previously inserted forceps in a similar manner, finally followed by advancing a straight guide wire in a well reduced position (D).
Fig. 5
Both hemostatic forceps are maintained in place (A) until the lag screw guide pin is placed in the proper position of the femoral head (C, D) to prevent recurrence of flexion deformity. With the distal interlocking holes circular (arrow) and posterior margins of both femoral condyles exactly overlapped in the lateral view (B), nail geometry can be used to get a correct rotational alignment (femoral anteversion of 15° in this case).
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Correction of Malalignment during Subtrochanteric Nailing

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

