Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 34(3); 2021 > Article
- Original Article Comparison of the Results between Plating and Intramedullary Nailing for Ipsilateral Fibular Fractures in Pilon Fractures
- Yong Jin Cho, Jun Young Lee, Jae Hwan Lim, Je Hong Ryu, Jung Ho Lee
-
Journal of Musculoskeletal Trauma 2021;34(3):97-104.
DOI: https://doi.org/10.12671/jkfs.2021.34.3.97
Published online: July 31, 2021
- 451 Views
- 3 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
To compare the results between plating and intramedullary nailing for ipsilateral fibular fractures in pilon fractures.
Materials and Methods
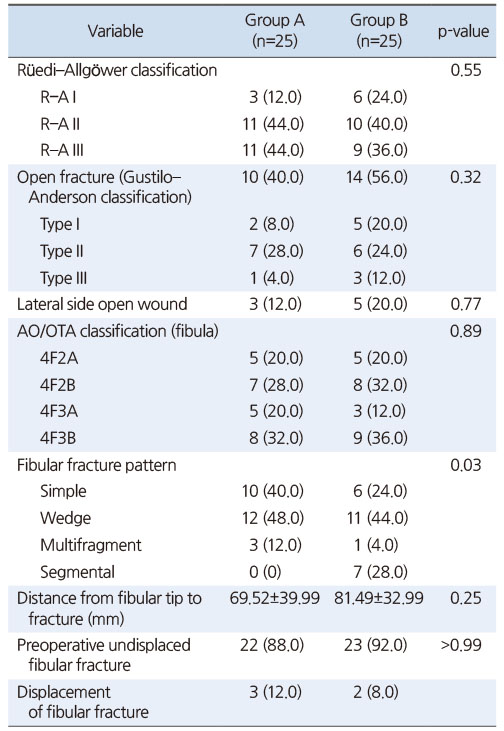
Among 124 patients with pilon fractures from November 2008 to March 2019, 50 patients with a fibular fracture were studied retrospectively and divided into two groups: Group A using a plate and Group B using a Rush pin. The radiological tests confirmed the fracture pat-terns (Rüedi–Allgöwer classification, AO/OTA classification) and evaluated the degree of reduction of fibular and tibial fractures after surgery. The American Orthopaedic Foot & Ankle Society (AOFAS) was examined for a clinical evaluation, and the complications were checked.
Results
The two groups showed similar distributions in gender, age, injury mechanism, diabetes, smoking, mean follow-up period, Rüedi–Allgöwer classification, AO/OTA classification, and open fracture.
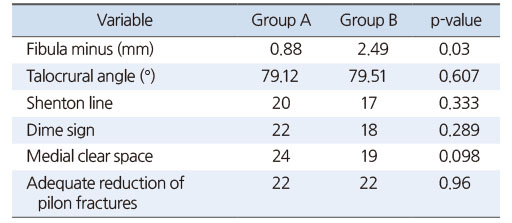
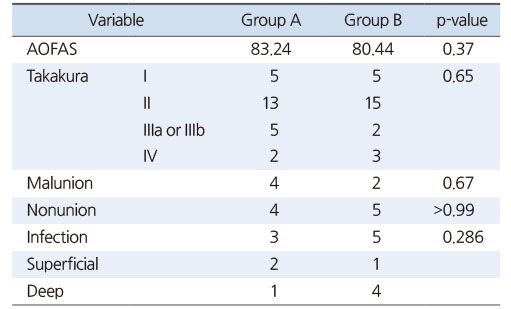
The fibular fractures were classified as simple, wedge, multiple, and segmental, showing significant differences between the two groups (p=0.03). There was no difference in the Talocrural angle, Shenton line, and Dime sign. In the reduction of pilon fractures, the appropriate reduction was obtained in 22 cases (88.0%) for both groups. The AOFAS averaged 83.24 in Group A and 80.44 points in Group B, showing no significant difference in complications (nonunion, malunion, infection, and arthritis).
Conclusion
Regardless of how the fibular fracture was fixed, the reduction of pilon fractures in both groups showed good results. Both intramedullary nail and plate fixation could be a suitable fixation method for ipsilateral fibular fractures with a low risk of shortening in pilon fractures.
Published online Jul 23, 2021.
https://doi.org/10.12671/jkfs.2021.34.3.97
Comparison of the Results between Plating and Intramedullary Nailing for Ipsilateral Fibular Fractures in Pilon Fractures
 , M.D.,
Jun Young Lee
, M.D.,
Jun Young Lee , M.D.,
Jae Hwan Lim
, M.D.,
Jae Hwan Lim , M.D.,
Je Hong Ryu
, M.D.,
Je Hong Ryu , M.D.
and Jung Ho Lee
, M.D.
and Jung Ho Lee , M.D.
, M.D.
Abstract
Purpose
To compare the results between plating and intramedullary nailing for ipsilateral fibular fractures in pilon fractures.
Materials and Methods
Among 124 patients with pilon fractures from November 2008 to March 2019, 50 patients with a fibular fracture were studied retrospectively and divided into two groups: Group A using a plate and Group B using a Rush pin. The radiological tests confirmed the fracture patterns (Rüedi-Allgöwer classification, AO/OTA classification) and evaluated the degree of reduction of fibular and tibial fractures after surgery. The American Orthopaedic Foot & Ankle Society (AOFAS) was examined for a clinical evaluation, and the complications were checked.
Results
The two groups showed similar distributions in gender, age, injury mechanism, diabetes, smoking, mean follow-up period, Rüedi-Allgöwer classification, AO/OTA classification, and open fracture. The fibular fractures were classified as simple, wedge, multiple, and segmental, showing significant differences between the two groups (p=0.03). There was no difference in the Talocrural angle, Shenton line, and Dime sign. In the reduction of pilon fractures, the appropriate reduction was obtained in 22 cases (88.0%) for both groups. The AOFAS averaged 83.24 in Group A and 80.44 points in Group B, showing no significant difference in complications (nonunion, malunion, infection, and arthritis).
Conclusion
Regardless of how the fibular fracture was fixed, the reduction of pilon fractures in both groups showed good results. Both intramedullary nail and plate fixation could be a suitable fixation method for ipsilateral fibular fractures with a low risk of shortening in pilon fractures.
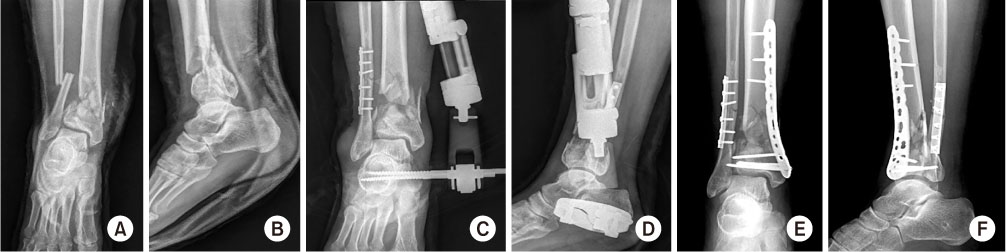
Fig. 1
A 44-year-old man in Group A, preoperative simple radiology (A: anterolateral view, B: lateral view), postoperative radiology after a primary emergency operation with external fixation for the tibia Pilon fracture and plate fixation for a fibular fracture (C: anterolateral view, D: lateral view), postoperative radiology after a secondary operation with internal fixation for a tibia pilon fracture (E: anterolateral view, F: lateral view).
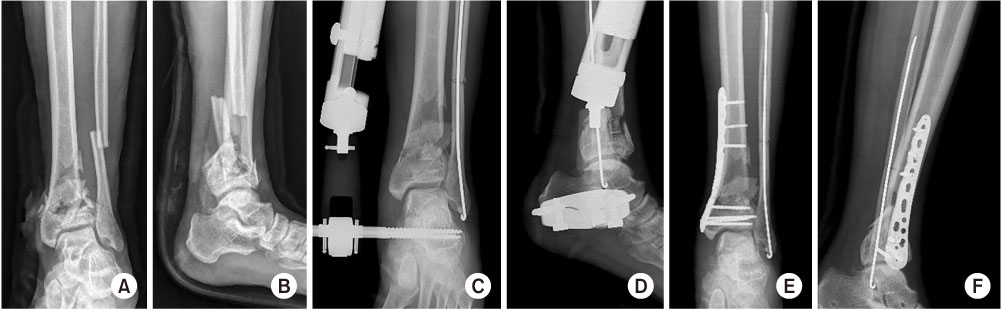
Fig. 2
A 55-year-old man in Group B, preoperative simple radiology (A: anterolateral view, B: lateral view), postoperative radiology after a primary emergency operation with external fixation for a tibia pilon fracture and Rush pin fixation for fibular fracture (C: anterolateral view, D: lateral view), postoperative radiology after a secondary operation with internal fixation for tibia pilon fracture (E: anterolateral view, F: lateral view).
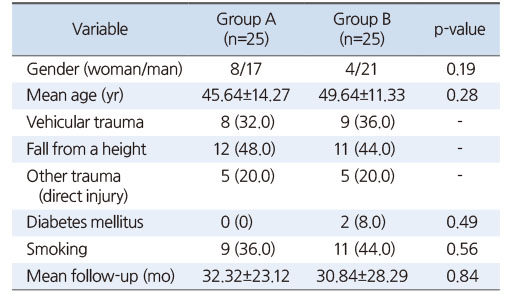
Fig. 3
(A) Fibular displacement (black solid line). The distance from the tip of fibula to the fracture (black dotted line). (B) Talocrural angle (white solid line), Dime sign (white circle), Shenton line (black dotted line), Medial clear space (black solid line). (C) Fibula minus, vertical distance between the horizontal line drawn from the distal tip of the fibula and the horizontal line drawn from the apex of the lateral process of the talus. (D) Reduction of a pilon fracture, varus or valgus deformity (black solid line), joint incongruent (black dotted line).
Table 1
Preoperative Demographics in the Two Groups
Table 2
Preoperative Radiologic Assessment in the Two Groups
Table 3
Radiological Results in the Two Groups
Table 4
Clinical Results and Complications in the Two Groups
References
-
Rüedi TP, Allgöwer M, et al. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res 1979;138:105–110.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

