Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 35(3); 2022 > Article
- Original Article Assessment of Noncontiguous Posterior Malleolar Fractures in Distal One-Third Tibia Shaft Fractures with Proximal Fibula Fractures
- Dae-Geun Kim, Byung Hoon Kwack
-
Journal of Musculoskeletal Trauma 2022;35(3):103-108.
DOI: https://doi.org/10.12671/jkfs.2022.35.3.103
Published online: July 31, 2022

- 491 Views
- 8 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
Posterior malleolar fractures after intramedullary nail surgery rarely occur in distal tibia shaft fractures. The importance of preoperative ankle evaluation in preventing these fractures is also common knowledge. There are no studies in the literature on posterior malleolar fractures in distal onethird tibia shaft fractures except for distal metaphyseal tibia fractures to the best of our knowledge. The purpose of this study was to evaluate the incidence and radiological features of posterior malleolar fractures in distal one-third tibia shaft fractures with proximal fibula fractures.
Materials and Methods
Thirty-one patients diagnosed with distal one-third tibia shaft fractures with proximal fibula fractures from January 2016 to May 2021 were retrospectively reviewed. With the aid of plain radiographs and computed tomography (CT) scans, the fracture patterns of the tibia and fibula were classified according to the AO Foundation/Orthopedic Trauma Association (AO/OTA) classification, and posterior malleolar fractures were identified. The fracture pattern was classified according to the Haraguchi classification, and the angle between the bimalleolar axis and the posterior malleolar fracture line was measured when there was a posterior malleolar fracture.
Results
Out of the 31 distal one-third tibia shaft fractures with proximal fibula fractures, 16 cases (51.6%) had noncontiguous posterior malleolar fractures that were confirmed on a CT scan, while 3 cases (18.8%) were visible on initial plain radiographs. There was no statistically significant variation seen in the presence of a posterior malleolar fracture in the tibia (p=0.15) and fibula (p=0.87) fractures.
According to the Haraguchi classification, there were 15 posterolateral-oblique fractures (Type I) and 1 medial-extension fracture (Type II), and the mean angle was 24.5°.
Conclusion
Noncontiguous posterior malleolar fractures occurred in approximately half of the distal one-third tibia shaft fractures with proximal fibula fractures, and a CT scan was considered necessary to diagnose posterior malleolar fractures before surgery
Published online Jul 25, 2022.
https://doi.org/10.12671/jkfs.2022.35.3.103
 , M.D., Ph.D.
and Byung Hoon Kwack
, M.D., Ph.D.
and Byung Hoon Kwack , M.D.
, M.D.
Abstract
Purpose
Posterior malleolar fractures after intramedullary nail surgery rarely occur in distal tibia shaft fractures. The importance of preoperative ankle evaluation in preventing these fractures is also common knowledge. There are no studies in the literature on posterior malleolar fractures in distal one-third tibia shaft fractures except for distal metaphyseal tibia fractures to the best of our knowledge. The purpose of this study was to evaluate the incidence and radiological features of posterior malleolar fractures in distal one-third tibia shaft fractures with proximal fibula fractures.
Materials and Methods
Thirty-one patients diagnosed with distal one-third tibia shaft fractures with proximal fibula fractures from January 2016 to May 2021 were retrospectively reviewed. With the aid of plain radiographs and computed tomography (CT) scans, the fracture patterns of the tibia and fibula were classified according to the AO Foundation/Orthopedic Trauma Association (AO/OTA) classification, and posterior malleolar fractures were identified. The fracture pattern was classified according to the Haraguchi classification, and the angle between the bimalleolar axis and the posterior malleolar fracture line was measured when there was a posterior malleolar fracture.
Results
Out of the 31 distal one-third tibia shaft fractures with proximal fibula fractures, 16 cases (51.6%) had noncontiguous posterior malleolar fractures that were confirmed on a CT scan, while 3 cases (18.8%) were visible on initial plain radiographs. There was no statistically significant variation seen in the presence of a posterior malleolar fracture in the tibia (p=0.15) and fibula (p=0.87) fractures. According to the Haraguchi classification, there were 15 posterolateral-oblique fractures (Type I) and 1 medial-extension fracture (Type II), and the mean angle was 24.5°.
Conclusion
Noncontiguous posterior malleolar fractures occurred in approximately half of the distal one-third tibia shaft fractures with proximal fibula fractures, and a CT scan was considered necessary to diagnose posterior malleolar fractures before surgery.
초록
목적
원위 경골 간부 골절에서 골수강내 금속정을 이용한 수술 후, 후과 골절이 드물게 발생한다. 하지만 이러한 연구들에는 원위 경골 골간단의 골절이 포함되어 있어서 원위 1/3 경골 간부 골절과 관련된 후과 골절에 대한 연구는 아직 없는 실정이다. 본 연구의 목적은 근위 비골 골절을 동반한 원위 1/3 경골 간부 골절에서 후과 골절에 대한 발생 빈도와 방사선학적인 결과를 평가하고자 하였다.
대상 및 방법
근위 비골 골절을 동반한 원위 1/3 경골 간부 골절로 진단된 31예를 대상으로 하였다. 단순 방사선 및 CT 검사를 시행한 결과로 후과 골절을 확인하였고, Haraguchi 분류를 이용하여 후과 골절을 분류하였으며, 후과 골절과 양과 골절 축 사이의 각도를 측정하였다.
결과
CT 검사상 16예(51.6%), 단순 방사선 검사상 3예(18.8%)에서 비연속적인 후과 골절이 확인되었다. Haraguchi 분류상 Type I이 15예, Type II가 1예였으며 평균 각도는 24.5도였다.
결론
근위 비골 골절을 동반한 원위 1/3 경골 간부 골절의 약 절반에서 비연속적인 후과 골절이 발생하였으며, 술 전 후과 골절에 대한 진단을 위해 CT 검사는 필요할 것으로 판단된다.
Introduction
Posterior malleolar fractures with distal third tibia shaft fractures were associated with spiral pattern fractures, low-energy trauma, and ipsilateral fibula fractures, with an incidence of 9%-43%.1,2,3) Boraiah et al.1) reported 2 cases of occult posterior malleolar fractures on plain radiographs and the importance of computed tomography (CT) scan of the ankle. Of 22 patients reported to have noncontiguous posterior malleolar fractures with spiral distal tibia shaft fractures in their study, 20 had fibula fractures proximal to the level of the tibia fractures. They emphasized the importance of evaluating occult ankle injury, particularly of the posterior malleolus, in spiral distal tibia shaft fractures with proximal fibula fractures.
The importance of evaluation and surgical treatment for posterior malleolar fractures in distal tibia shaft fractures has been widely reported.2,3) However, reports in the literature present the results of a mix of distal one-third tibial shaft fractures and distal metaphyseal tibial fractures. To the best of our knowledge, no studies have reported the features and incidence of posterior malleolar fractures in distal one-third tibia shaft fractures with proximal fibula fractures. The purpose of this study was to evaluate the incidence and radiological features of posterior malleolar fractures in distal one-third tibia shaft fractures with proximal fibula fractures and to determine the usefulness of a CT scan of the ankle.
Materials and Methods
1. Patients selection
This retrospective single-center cohort study was approved by the Institutional Review Board of Soonchunhyang University Gumi Hospital (IRB No. 2021-03), and patient consent was waived due to the retrospective nature of the study. Thirty-one patients diagnosed with distal one-third tibia shaft fractures with proximal fibula fractures from January 2016 to May 2021 at Soonchunhyang University Gumi Hospital were retrospectively reviewed. The distal one-third tibia shaft fractures included fractures of 5 cm proximal to the ankle joint line.4) Each patient had to have initial plain radiographs and CT images, including the full length of the tibia, knee, and ankle joint. Fifteen male and 16 female patients were reviewed, and their mean age was 50.4 years (range, 25-86 years). According to the AO Foundation/Orthopedic Trauma Association (AO/OTA) classification,5) tibia fractures were 17 42A1, 1 42A3, 5 42B2, and 8 42B3, and fibula fractures were 14 4F2A and 17 4F2B. There were 3 cases of open fracture, and they were all Type I according to the Gustilo and Anderson classification.6)
2. Radiologic evaluation
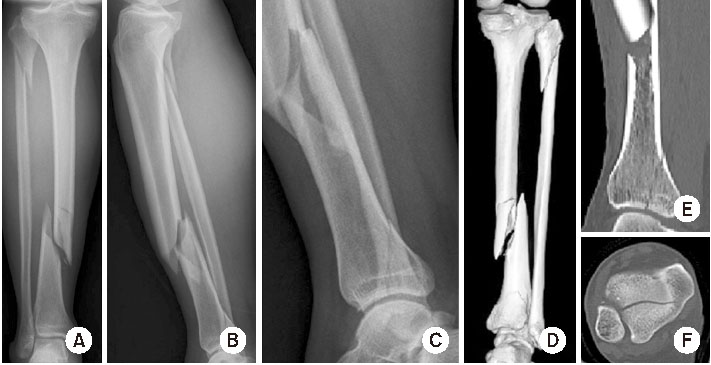
We retrospectively reviewed all the radiographs. Anteroposterior, lateral, and mortise radiographs were used to confirm posterior malleolar fractures on plain radiographs (Fig. 1). The CT images were obtained using a 128-slice CT scanner (Somatom Definition AS+; Siemens Healthcare, Forchheim, Germany). Serial 3.0 mm tomograms were obtained, including the knee and ankle joint without contrast. Axial, coronal, and sagittal reformation images were used. An axial image from the CT 3.0 mm above the tibia plafond was used to confirm posterior malleolar fracture on the CT scan. Posterior malleolar fractures were classified according to the Haraguchi classification,7) and the angle between the bimalleolar axis and the posterior malleolar fracture line was measured.
Fig. 1
(A-C) Anteroposterior/lateral X-rays of distal one-third a tibial shaft fracture with proximal fibular fracture. The spiral tibial shaft fracture was located 6 cm proximal to the articular surface. No posterior malleolus fracture was detected. (D-F) Computed tomography imaging revealed a nondisplaced and noncontiguous posterior malleolus fracture.
3. Statistical methods
IBM SPSS Statistics program (ver. 25.0; IBM, Armonk, NY, USA) was used to analyze radiologic results and calculate the p-value. The p-value was calculated using the Mann–Whitney test, Pearson’s chi-square test, and Fisher’s exact test, and p<0.05 was considered statistically significant.
Results
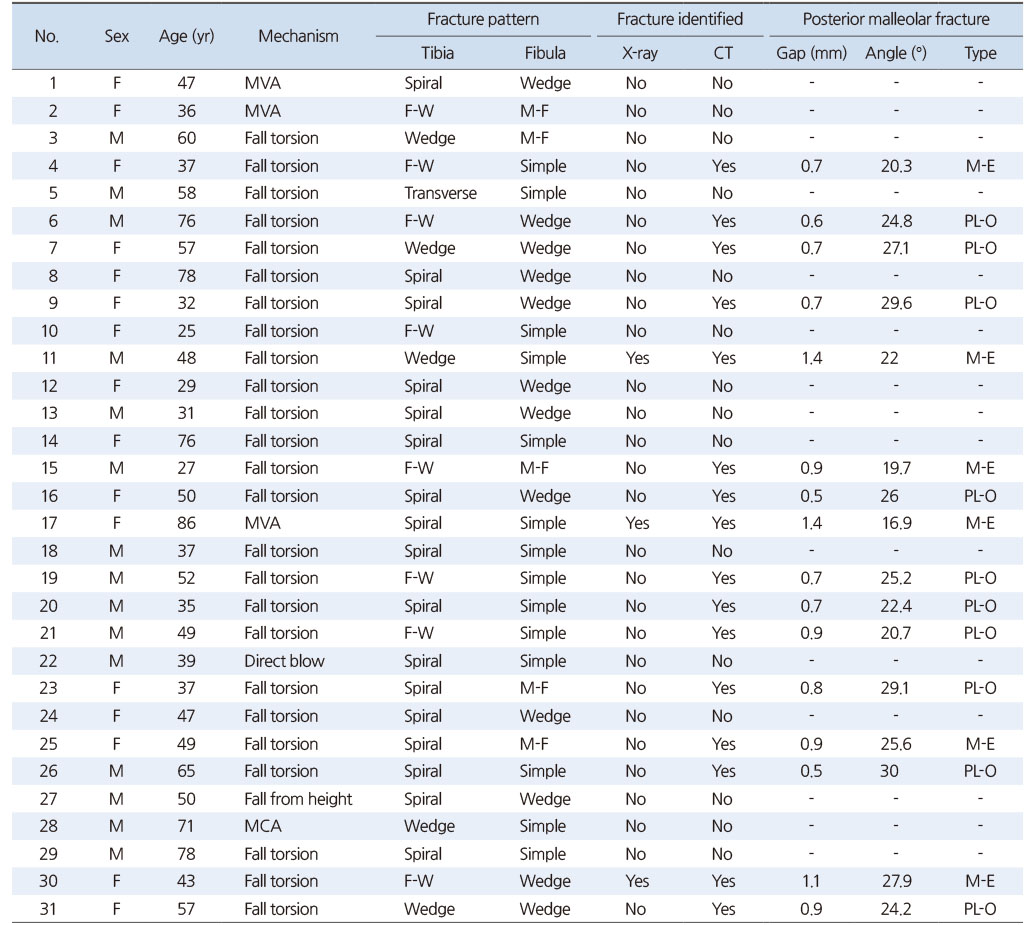
Consecutive cases of the 31 distal one-third tibia shaft fractures with proximal fibula fractures in our study revealed that 16 cases (51.6%) had posterior malleolar fractures that were confirmed on a CT scan (Fig. 1). In all cases, the fracture line of posterior malleolar fractures was not connected with the distal one-third tibia shaft fractures. Of the 16 fractures identified on a CT scan, 3 cases (18.8%) were visible on initial plain radiographs (Fig. 2). The fracture gap was more than 1.0 mm in all 3 cases. In 16 posterior malleolar fractures, the mean fracture gap was 0.8 mm (0.5-1.4 mm), and the mean angle of the fracture off the bimalleolar axis was 24.5° (16.9°-30°). According to the Haraguchi classification,7) there were 15 posterolateral-oblique fractures (Type I) and 1 medial-extension fracture (Type II). In the tibia fracture pattern, wedges and fragmentary wedges showed a spiral pattern in all cases. Thirty cases showed a spiral tibia fracture pattern. Twenty-five cases resulted from low-energy torsion mechanisms (Table 1).
Fig. 2
(A-C) Anteroposterior/lateral X-rays of a distal one-third tibial shaft fracture with proximal fibular fracture. The wedge tibial shaft fracture was 8 cm proximal to the articular surface. Posterior malleolus fracture was detected. (D-F) Computed tomography imaging revealed a nondisplaced and noncontiguous posterior malleolus fracture.
Table 1
Distribution of Noncontiguous Posterior Malleolar Fractures in Distal One-Third Tibial Shaft Fractures with Proximal Fibular Fractures
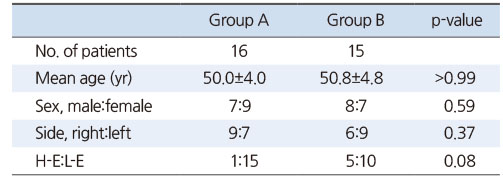
To determine the factors contributing to the tibia or fibula fracture pattern for posterior malleolar fractures, we identified two groups according to the presence or absence of posterior malleolar fractures. The patients’ demographics for each group are given in Table 2. There was no statistical difference in the patients’ demographics for both groups (p>0.05). We simplified the AO/OTA classification5) to 42A, 42B, and 42C to determine factors contributing to the posterior malleolar fracture based on the type of distal one-third tibia shaft fractures. The groups with posterior malleolar fractures were 7 42A and 9 42B, and those without posterior malleolar fractures were 7 42A and 8 42B. There was no statistical difference between the two groups (p=0.15). Based on the type of proximal fibula fractures, the groups with posterior malleolar fractures were 7 4F2A and 9 4F2B, and those without posterior malleolar fractures were 7 4F2A and 8 4F2B. There was no statistical difference between the two groups (p=0.87).
Table 2
Demographic Data
Discussion
This study aimed to evaluate the usefulness of a CT scan for posterior malleolar fractures in distal one-third tibia shaft fractures with proximal fibula fractures. Georgiadis et al.8) reported the displacement of occult posterior malleolar fractures in 4 cases during intramedullary nailing of external rotational tibia shaft fractures. They recommended preoperative evaluation of the ankle joint. Purnell et al.3) showed the importance of CT scans in Noncontiguous malleolar fractures with distal third tibia shaft fractures. They reported that the diagnostic rates of orthopedic surgeons and musculoskeletal radiologists using plain radiographs were 45% and 69%, respectively. However, among distal third tibia fractures, those occurring more than 5 cm from the ankle joint line were in 16 out of 29 cases, and nondisplaced posterior malleolar fractures were in 11 out of the 16 cases. Of these 11 cases, 1 and 3 cases were detected by orthopedic surgeons and musculoskeletal radiologists on plain radiographs, respectively. Thus, the orthopedic surgeons could not detect 90.9% of the occult posterior malleolar fractures with distal one-third tibia shaft fractures on plain radiographs. In our study, 13 (81.3%) out of 16 cases with posterior malleolar fractures confirmed by CT scan were not detected by plain radiographs.
Böstman9,10) reported that displaced malleolar fractures, including the posterior malleolar fractures, accounted for 0.9% of tibia shaft fractures and 3.9% of spiral tibia shaft fractures. Fibula fractures associated with spiral tibia shaft fractures were common with high diaphyseal fibula fractures and did not influence the severity of displacement of the spiral tibia fractures. Purnell et al.3) showed that spiral fracture patterns occurred in 72% of distal third tibia fractures and 93% of associated intra-articular malleolar fractures. In our study, 96.8% of distal one-third tibia shaft fractures with proximal fibula fractures were spiral patterns.
Haraguchi and Armiger11), in a cadaveric study, showed that fractures at the posterolateral corner of the distal tibia (Type I according to the Haraguchi classification7)) were produced by external rotation of the talus. In contrast, fractures involving the entire posterior tibia margin (Type II according to the Haraguchi classification7)) were produced by external rotation of the talus and axial loading from the talus. Kellam et al.12) reported in a comparative study of tibia shaft versus rotational ankle fractures that the posterior malleolar fractures of the tibia shaft fractures were twice as large, medial-extension fractures (Type II) were more than posterolateral-oblique fractures (Type I), and the mean angle of the fracture off the bimalleolar axis was 21° compared with 24° in rotational ankle fractures. Mitchell et al.13) showed that posterolateral-oblique fractures occurred in 93% of posterior malleolar fractures with spiral infraisthmal tibia fractures, and the mean angle of the fracture off the bimalleolar axis was 24°. In our study, 15 (93.8%) out of 16 cases had posterolateral-oblique fractures, and the mean angle of the fracture off the bimalleolar axis was 24.5°. In the posterior malleolar fractures of distal one-third tibia shaft fractures with proximal fibula fractures, the external rotational ankle injury was considered the mechanism of injury.
This study had several limitations. First, this study was a retrospective study. Rather than a study on patients who underwent surgery, we thought that selection bias could be reduced in this study because it included all diagnosed patients. Second, the sample group was small and nonparametric statistics were used to derive the results. We believed that purified data could be obtained for distal one-third tibia shaft fractures with proximal fibula fractures because distal metaphyseal tibia fractures were excluded. However, this might be the strength of our study because it was performed by single-center applying the same radiologic evaluation protocol for the fractures.
In summary, posterior malleolar fractures were less likely to be diagnosed in distal one-third tibia shaft fractures with proximal fibula fractures on plain radiographs, and a CT scan was required for confirmation. The tibia or fibula fracture pattern did not establish the presence of posterior malleolar fractures. The posterior malleolar fractures of distal one-third tibia shaft fractures with proximal fibula fractures were thought to be caused by a rotational ankle injury mechanism, unlike those of tibia shaft fractures.
Conclusion
Noncontiguous posterior malleolar fractures occurred in approximately half of the distal one-third tibia shaft fractures with proximal fibula fractures and commonly appeared as occult fractures. CT scan was required to diagnose posterior malleolar fractures before surgery in distal one-third tibia shaft fractures with proximal fibula fractures.
Financial support:None.
Conflict of interests:None.
References
-
Böstman OM. Displaced malleolar fractures associated with spiral fractures of the tibial shaft. Clin Orthop Relat Res 1988;(228):202–207.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

