Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 26(1); 2013 > Article
-
Review Article
- Updated Basic Principles of Internal Fixation of Fracture
- Oog-Jin Shon, M.D., Ji-Wan Kim, M.D., Beom-Jung Kim, M.D.
-
Journal of the Korean Fracture Society 2013;26(1):81-91.
DOI: https://doi.org/10.12671/jkfs.2013.26.1.81
Published online: January 17, 2013
Department of Orthopedic Surgery, Yeungnam University Medical Center, Daegu, Korea.
*Department of Orthopaedic Surgery, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- Address reprint requests to: Oog-Jin Shon, M.D. Department of Orthopedic Surgery, Yeungnam University Medical Center, 170, Hyeonchung-ro, Nam-gu, Daegu 705-717, Korea. Tel: 82-53-620-3640, Fax: 82-53-628-4020, ossoj@med.yu.ac.kr
Copyright © 2013 The Korean Fracture Society
- 1,843 Views
- 50 Download
- 3 Crossref
- 1. Aguila AZ, Manos JM, Orlansky AS, Todhunter RJ, Trotter EJ, Van der Meulen MC. In vitro biomechanical comparison of limited contat dynamic compression plate and locking compression plate. Vet Comp Orthop Traumatol, 2005;18:220-226.Article
- 2. Ahmad M, Nanda R, Bajwa AS, Candal-Couto J, Green S, Hui AC. Biomechanical testing of the locking compression plate: when does the distance between bone and implant significantly reduce construct stability? Injury, 2007;38:358-364.Article
- 3. Bagby GW, Janes JM. The effect of compression on the rate of fracture healing using a special plate. Am J Surg, 1958;95:761-771.Article
- 4. Baumgaertel F, Buhl M, Rahn BA. Fracture healing in biological plate osteosynthesis. Injury, 1998;29:Suppl 3. C3-C6.Article
- 5. Cheal EJ, Mansmann KA, DiGioia AM 3rd, Hayes WC, Perren SM. Role of interfragmentary strain in fracture healing: ovine model of a healing osteotomy. J Orthop Res, 1991;9:131-142.Article
- 6. Danis R. Théorie et pratique de l'ostéosynthése, Paris, Masson. 1949.
- 7. Eggers GW. Internal contact splint. J Bone Joint Surg Am, 1948;30A:40-52.Article
- 8. Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma, 2004;18:488-493.Article
- 9. Frigg R. Development of the locking compression plate. Injury, 2003;34:Suppl 2. B6-B10.Article
- 10. Gautier E, Perren SM. Limited contact dynamic compression plate (LC-DCP)-biomechanical research as basis to new plate design. Orthopade, 1992;21:11-23.
- 11. Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury, 2003;34:Suppl 2. B63-B76.Article
- 12. Gerber C, Mast JW, Ganz R. Biological internal fixation of fractures. Arch Orthop Trauma Surg, 1990;109:295-303.ArticlePDF
- 13. Goodship AE, Kenwright J. The influence of induced micromovement upon the healing of experimental tibial fractures. J Bone Joint Surg Br, 1985;67:650-655.ArticlePDF
- 14. Kowalski MJ, Schemitsch EH, Harrington RM, Chapman JR, Swiontkowski MF. A comparative biomechanical evaluation of a noncontacting plate and currently used devices for tibial fixation. J Trauma, 1996;40:5-9.Article
- 15. Krettek C, Miclau T, Grün O, Schandelmaier P, Tscherne H. Intraoperative control of axes, rotation and length in femoral and tibial fractures. Technical note. Injury, 1998;29:Suppl 3. C29-C39.Article
- 16. Kubiak EN, Fulkerson E, Strauss E, Egol KA. The evolution of locked plates. J Bone Joint Surg Am, 2006;88:Suppl 4. 189-200.Article
- 17. Lambotte A. Technique et indication des prothéses dans le traitement des fractures. Presse Med, 1909;17:321.
- 18. Lane WA. Some remarks on the treatment of fractures. Br Med J, 1895;1:861-863.Article
- 19. Laurence M, Freeman MA, Swanson SA. Engineering considerations in the internal fixation of fractures of the tibial shaft. J Bone Joint Surg Br, 1969;51:754-768.ArticlePDF
- 20. Mast J, Jakob R, Ganz R. Planning and reduction technique in fracture surgery, 1989;Berlin; New York, Springer-Verlag. xiii254.
- 21. Müller M, Allgöwer M, Willenegger H. Compression fixation with plates. Technique of internal fixation of fractures, 1965;Berlin, Springer. 47-51.
- 22. Niemeyer P, Südkamp NP. Principles and clinical application of the locking compression plate (LCP). Acta Chir Orthop Traumatol Cech, 2006;73:221-228.Article
- 23. Perren SM. The concept of biological plating using the limited contact-dynamic compression plate (LC-DCP). Scientific background, design and application. Injury, 1991;22:Suppl 1. 1-41.Article
- 24. Perren SM. Evolution and rationale of locked internal fixator technology. Introductory remarks. Injury, 2001;32:Suppl 2. B3-B9.
- 25. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br, 2002;84:1093-1110.
- 26. Rahn BA, Gallinaro P, Baltensperger A, Perren SM. Primary bone healing. An experimental study in the rabbit. J Bone Joint Surg Am, 1971;53:783-786.
- 27. Rozbruch SR, Müller U, Gautier E, Ganz R. The evolution of femoral shaft plating technique. Clin Orthop Relat Res, 1998;(354):195-208.Article
- 28. Ruedi TP, Murphy MW. AO principles of fracture management, 2000;1st ed. Stuttgart; New York, Thieme. 7-31. 139-155. 169-184. 195-218. 221-230. 249-253. 290-305.
- 29. Schatzker J. Changes in the AO/ASIF principles and methods. Injury, 1995;26:Suppl 2. 51-56.Article
- 30. Stoffel K, Dieter U, Stachowiak G, Gächter A, Kuster MS. Biomechanical testing of the LCP-how can stability in locked internal fixators be controlled? Injury, 2003;34:Suppl 2. B11-B19.Article
- 31. Tepic S, Perren S. The biomechanics of the PC-Fix internal fixator. Injury, 1995;26:Suppl 2. 5-10.Article
- 32. Tong GO, Bavonratanavech S. AO manual of fracture management. Minimally invasive plate osteosynthesis (MIPO), 2007;1st ed. Stuttgart, Thieme. 3-45. 66-118. 305-325.
- 33. Von Recum J, Wendl K, Vock B, Grützner PA, Franke J. Intraoperative 3D C-arm imaging. State of the art. Unfallchirurg, 2012;115:196-201.ArticlePDF
- 34. Wagner M. General principles for the clinical use of the LCP. Injury, 2003;34:Suppl 2. B31-B42.Article
REFERENCES
Fig. 1
Various kinds of minimally invasive osteosynthesis (MIO).
(A) Minimally invasive plate osteosynthesis (MIPO).
(B) Minimally invasive nail osteosynthesis (MINO).
(C) Minimally invasive screw osteosynthesis (MISO).
(D) Minimally invasive external fixator osteosynthesis (MIEFO).
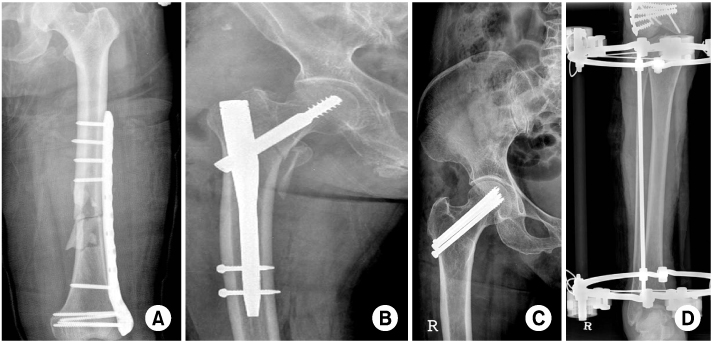
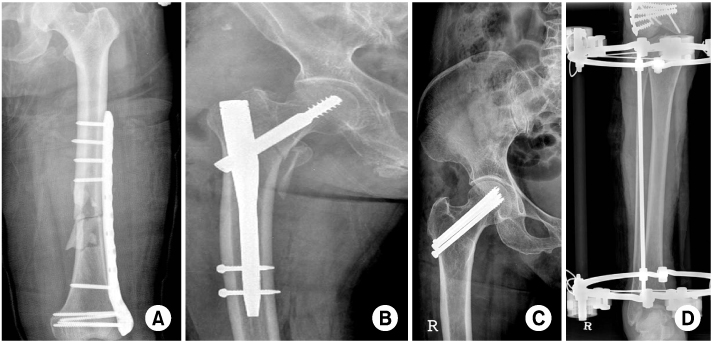
Fig. 2
Fracture of the distal lower leg in a 45-year-old man.
(A) Anteroposterior view of the lower leg demonstrating the distal fracture.
(B) It was treated by conventional plating of the distal fibula and locking compression plate (LCP) osteosynthesis of the distal tibia using a minimally invasive plate osteosynthesis (MIPO) technique.
(C) After implant removal 10 months after injury.


Fig. 3
Fracture of the lower leg in a 31-year-old man.
(A) Multiple injured male with open wound of both lower extremities caused by pedestrian traffic accident. Metaphyseal comminuted fracture of tibia, fibula.
(B) Because the compromised soft tissue did not allow open reduction, consolidation was attempted with the initially applied external fixator.
(C) After 2 weeks, lateral plate fixation of the distal tibia using the minimally invasive plate osteosynthesis (MIPO) technique was performed and free flap was applied.
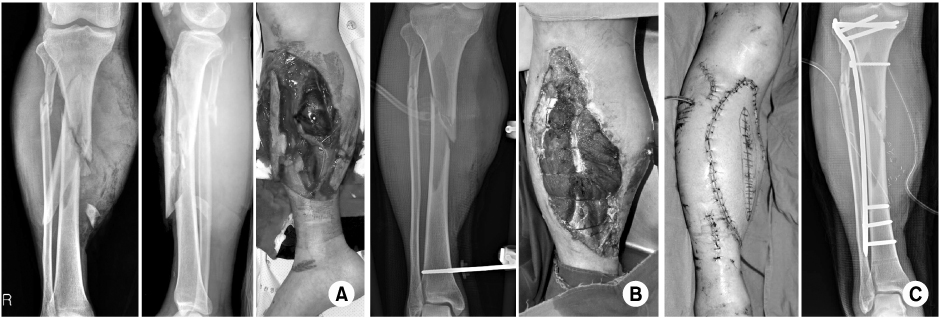
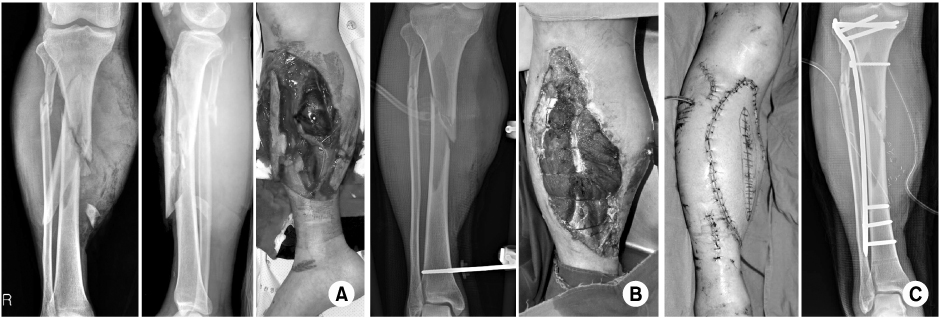
Fig. 4
Open fracture of the lower leg in a 38-year-old man caused by a traffic accident.
(A) Metaphyseal comminuted fracture of tibia, fibula.
(B) A contaminated fracture fragment was removed, consolidation was attempted with the initially applied external fixator. An antibiotic containig cement bead was inserted in dead space.
(C) After 2 weeks, cement bead was removed, osteotomy & external fixation of distal tibial fragment was performed for bone transport and skin graft was applied.
(D) After 6 weeks, bone transport was done. External fixator was removed and fragment was fixed with previous locking compression plate (LCP).
(E) After 12 weeks, internal fixation, and bone graft was performed using autogenous iliac bone.
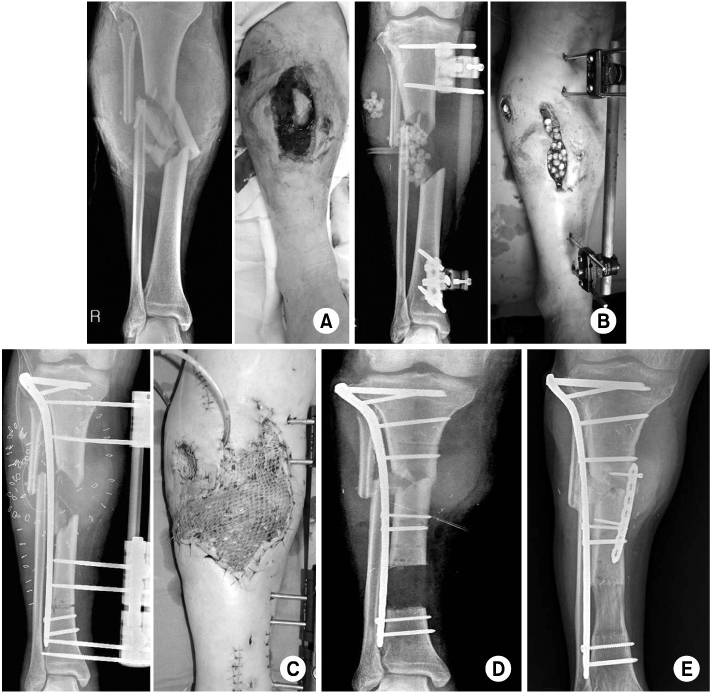
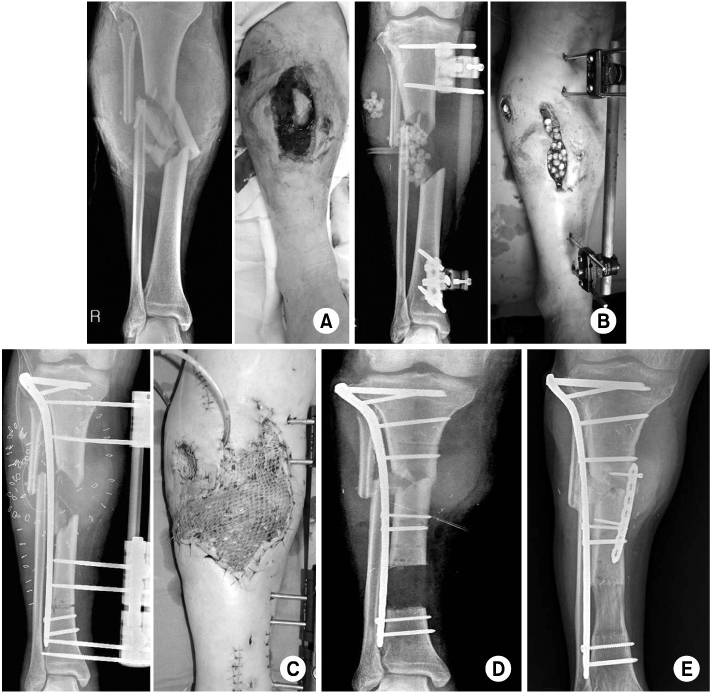
Fig. 7
Lateral entry nail of proximal femur.
(A) Spiral fracture of the femoral shaft in a 25-year-old male.
(B) Nailing was performed with A2FN (Expert Asian Femoral Nail, AO).
(C) Simple fracture of the femoral shaft in a 37-year-old female.
(D) Nailing was performed with Sirus nail (Zimmer).
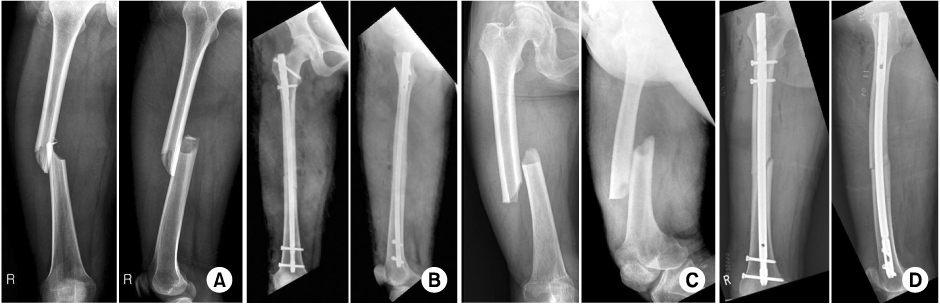
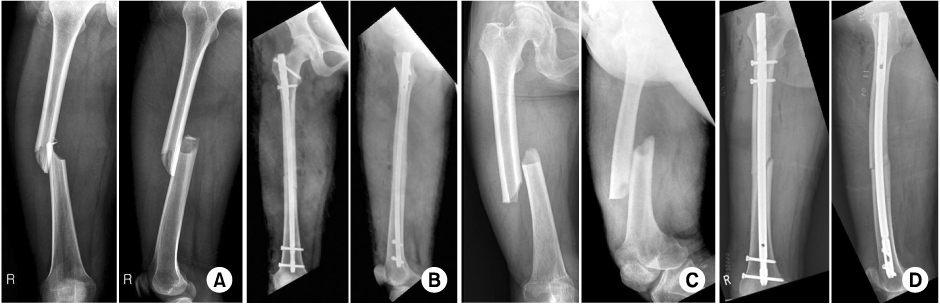
Fig. 8
Collinear reduction clamp can be used for reduction.
(A) Instrument.
(B, C) Intraoperative use.
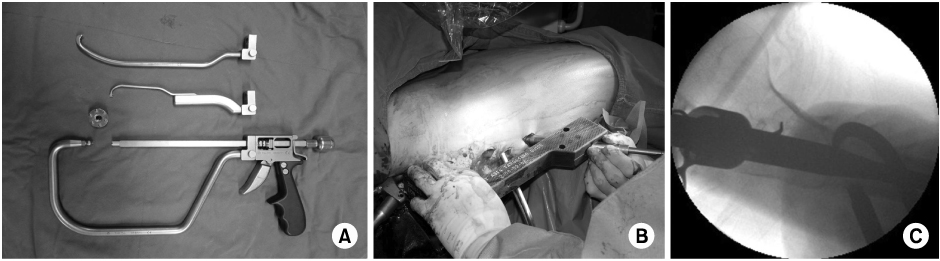
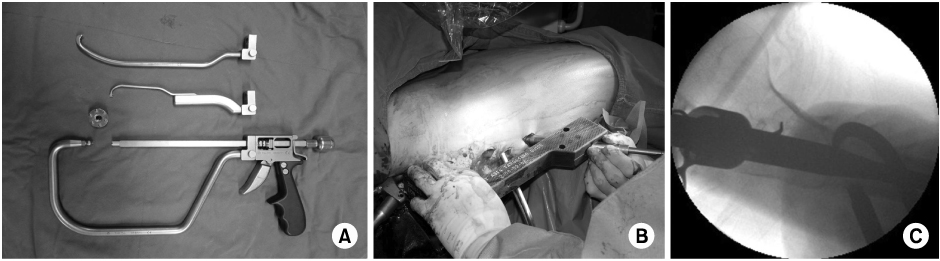
Fig. 9
Periarticular wiring can be used for reduction.
(A) Instrument.
(B) Intraoperative use.
(C) Subtrochanteric fracture of femur in a 58-year-old female.
(D) Reduction was performed using wring and nailing was done.
(E) Follow-up x-rays 6 months after surgery showed good fracture healing with callus formation.


Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Safety and Efficacy of Korean Medicine Treatment Including Chuna Manual Therapy for Patients with Spinal, Pelvic, or Hip Fractures: A Retrospective Chart Review
Omin Kwon, Somi Jung, Seju Chang, Jungmin Lee
Journal of Korean Medicine Rehabilitation.2025; 35(4): 143. CrossRef - A Review of Domestic and International Clinical Research Trends on Pharmacopuncture Treatment for Fractures
Hea Sun Chun
Journal of Physiology & Pathology in Korean Medicine.2023; 37(6): 185. CrossRef - Comparison of Greater Trochanter Versus Piriformis Entry Nail for Treatment of Femur Shaft Fracture
Jong-Hee Lee, Jong-Hoon Park, Si-Yeong Park, Seong-Cheol Park, Seung-Beom Han
Journal of the Korean Fracture Society.2014; 27(4): 287. CrossRef
Updated Basic Principles of Internal Fixation of Fracture
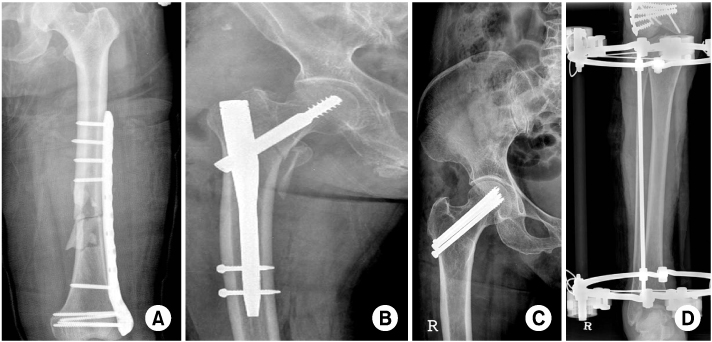

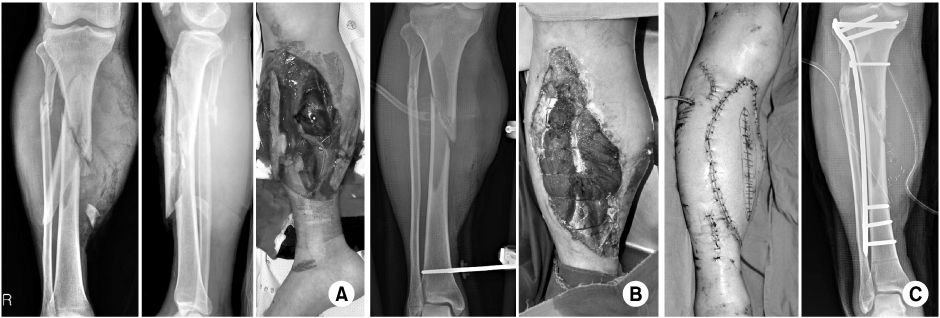


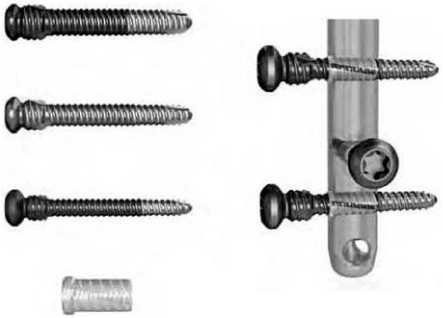
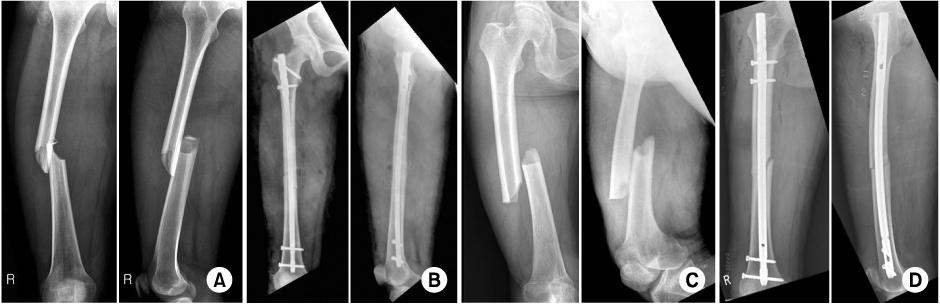
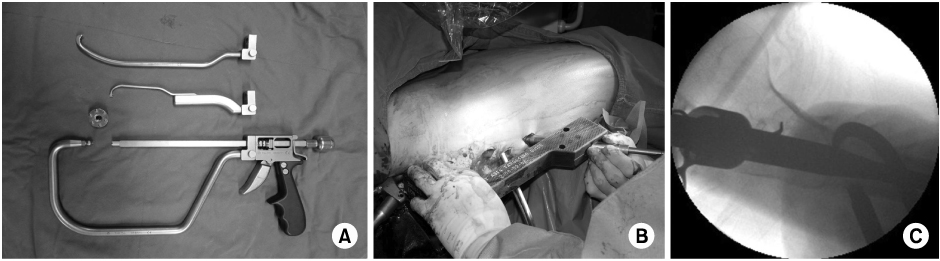

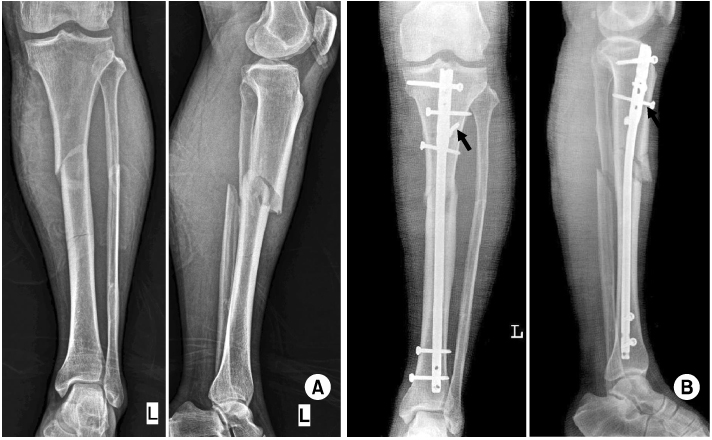
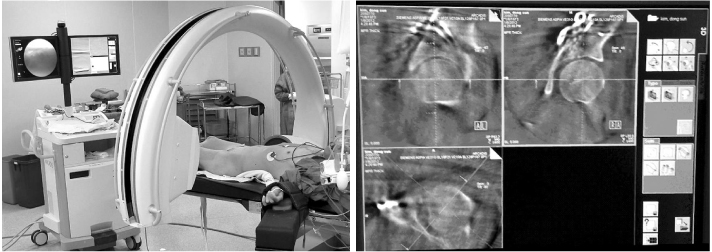
Fig. 1
Various kinds of minimally invasive osteosynthesis (MIO).
(A) Minimally invasive plate osteosynthesis (MIPO).
(B) Minimally invasive nail osteosynthesis (MINO).
(C) Minimally invasive screw osteosynthesis (MISO).
(D) Minimally invasive external fixator osteosynthesis (MIEFO).
Fig. 2
Fracture of the distal lower leg in a 45-year-old man.
(A) Anteroposterior view of the lower leg demonstrating the distal fracture.
(B) It was treated by conventional plating of the distal fibula and locking compression plate (LCP) osteosynthesis of the distal tibia using a minimally invasive plate osteosynthesis (MIPO) technique.
(C) After implant removal 10 months after injury.
Fig. 3
Fracture of the lower leg in a 31-year-old man.
(A) Multiple injured male with open wound of both lower extremities caused by pedestrian traffic accident. Metaphyseal comminuted fracture of tibia, fibula.
(B) Because the compromised soft tissue did not allow open reduction, consolidation was attempted with the initially applied external fixator.
(C) After 2 weeks, lateral plate fixation of the distal tibia using the minimally invasive plate osteosynthesis (MIPO) technique was performed and free flap was applied.
Fig. 4
Open fracture of the lower leg in a 38-year-old man caused by a traffic accident.
(A) Metaphyseal comminuted fracture of tibia, fibula.
(B) A contaminated fracture fragment was removed, consolidation was attempted with the initially applied external fixator. An antibiotic containig cement bead was inserted in dead space.
(C) After 2 weeks, cement bead was removed, osteotomy & external fixation of distal tibial fragment was performed for bone transport and skin graft was applied.
(D) After 6 weeks, bone transport was done. External fixator was removed and fragment was fixed with previous locking compression plate (LCP).
(E) After 12 weeks, internal fixation, and bone graft was performed using autogenous iliac bone.
Fig. 5
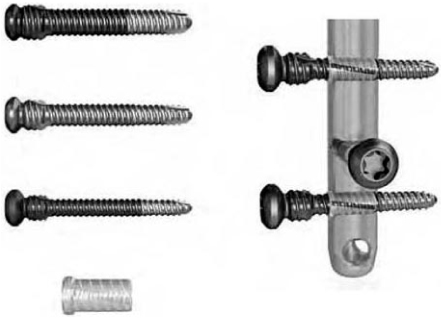
Expert nailing system.
Fig. 6
Angular stable locking system (ASLS).
Fig. 7
Lateral entry nail of proximal femur.
(A) Spiral fracture of the femoral shaft in a 25-year-old male.
(B) Nailing was performed with A2FN (Expert Asian Femoral Nail, AO).
(C) Simple fracture of the femoral shaft in a 37-year-old female.
(D) Nailing was performed with Sirus nail (Zimmer).
Fig. 8
Collinear reduction clamp can be used for reduction.
(A) Instrument.
(B, C) Intraoperative use.
Fig. 9
Periarticular wiring can be used for reduction.
(A) Instrument.
(B) Intraoperative use.
(C) Subtrochanteric fracture of femur in a 58-year-old female.
(D) Reduction was performed using wring and nailing was done.
(E) Follow-up x-rays 6 months after surgery showed good fracture healing with callus formation.
Fig. 10
(A) Spiral fracture of shaft in a 28-year-old female.
(B) Reduction was performed with polar screw (arrow).
Fig. 11
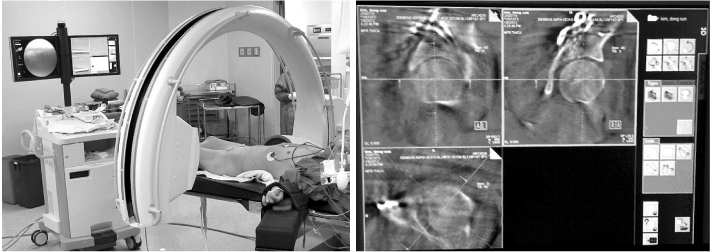
3-dimensional C-arm.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
Fig. 9
Fig. 10
Fig. 11
Updated Basic Principles of Internal Fixation of Fracture

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

