Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 27(1); 2014 > Article
-
Original Article
- Treatment and Prognosis of Femoral Insufficiency Fracture Associated with Prolonged Bisphosphonate Use
- Ki Chan An, M.D., Dae Hyun Park, M.D., Guemin Gong, M.D., Ju-Young Kim, M.D., Sang-Bum Kim, M.D., Seung-Yeob Sakong, M.D.
-
Journal of the Korean Fracture Society 2014;27(1):10-16.
DOI: https://doi.org/10.12671/jkfs.2014.27.1.10
Published online: January 17, 2014
Department of Orthopedic Surgery, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- Address reprint requests to: Dae Hyun Park, M.D. Department of Orthopedic Surgery, Busan Paik Hospital, Inje University College of Medicine, 75 Bokji-ro, Busanjin-gu, Busan 614-735, Korea. Tel: 82-51-890-6257, Fax: 82-51-892-6619, ronin211@naver.com
Copyright © 2014 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 572 Views
- 0 Download
- 1 Crossref
Abstract
-
Purpose
- This study was conducted to investigate and identify an appropriate fracture treatment method by analyzing patients in whom a femoral incompetence fracture occurred after receiving a long-term bisphosphonate administration.
-
Materials and Methods
- The subjects of this study were 13 cases out of ten patients among those who had a history of receiving bisphosphonate for more than five years and had a fracture or an imminent fracture with a characteristic radiological finding in the femoral subtrochanteric region and the interfemoral region. The period of the drug administration, bone density, the existence of a prodromal symptom, and bilateral fracture were investigated.
-
Results
- In seven out of the 13 cases, the patients complained of painat the femoral and pelvic parts as a prodrome (53.8%), and three of them showed a bilateral fracture (30%). An imminent fracture with a prodrome was observed in six cases (46.2%); for three of these cases, a prophylactic fixture pexis was performed by inserting a metal nail into the medullary cavity, and in two out of these three, a complete fracture was found within 11 months on average (3 to 19 months). In the three prophylactic fixture pexis performed cases, no postoperative complications were found, and a radiological finding of concrescence was seen within one year after the operation. Among the nine operation performed cases after the fracture, non-union was found in two.
-
Conclusion
- In the patients who have received bisphosphonate for a long periodof time, a prodome may be a useful indicator of a fracture in the femoral subtrochanteric region and the interfemoral region; therefore, a careful observation is necessary. A prophylactic internal fixation is recommended for patients with imminent fracture with a prodome since they have a high risk of a complete fracture is high in them.
- 1. Arkan SSN, Bakir KK, Göran OS. Bisphosphonate-induced femoral fragility fractures: what do we know? Orthop Res Rev, 2010;2:27-34.
- 2. Banffy MB, Vrahas MS, Ready JE, Abraham JA. Nonoperative versus prophylactic treatment of bisphosphonate-associated femoral stress fractures. Clin Orthop Relat Res, 2011;469:2028-2034.PubMedPMC
- 3. Boivin G, Meunier PJ. Changes in bone remodeling rate influence the degree of mineralization of bone. Connect Tissue Res, 2002;43:535-537.
- 4. Currey JD. Effects of differences in mineralization on the mechanical properties of bone. Philos Trans R Soc Lond B Biol Sci, 1984;304:509-518.PubMedPDF
- 5. Fowler JR, Craig MR. Association of low-energy femoral shaft fractures and bisphosphonate use. Orthopedics, 2012;35:e38-e40.PubMed
- 6. Gates BJ, Sonnett TE, Duvall CA, Dobbins EK. Review of osteoporosis pharmacotherapy for geriatric patients. Am J Geriatr Pharmacother, 2009;7:293-323.
- 7. Girgis CM, Sher D, Seibel MJ. Atypical femoral fractures and bisphosphonate use. N Engl J Med, 2010;362:1848-1849.
- 8. Isaacs JD, Shidiak L, Harris IA, Szomor ZL. Femoral insufficiency fractures associated with prolonged bisphosphonate therapy. Clin Orthop Relat Res, 2010;468:3384-3392.
- 9. Kwek EB, Goh SK, Koh JS, Png MA, Howe TS. An emerging pattern of subtrochanteric stress fractures: a long-term complication of alendronate therapy? Injury, 2008;39:224-231.
- 10. Leslie WD, O'Donnell S, Jean S, et al. Osteoporosis Surveillance Expert Working Group. Trends in hip fracture rates in Canada. JAMA, 2009;302:883-889.
- 11. Luckman SP, Hughes DE, Coxon FP, Graham R, Russell G, Rogers MJ. Nitrogen-containing bisphosphonates inhibit the mevalonate pathway and prevent post-translational prenylation of GTP-binding proteins, including Ras. J Bone Miner Res, 1998;13:581-589.PDF
- 12. Morris CD, Einhorn TA. Bisphosphonates in orthopaedic surgery. J Bone Joint Surg Am, 2005;87:1609-1618.
- 13. Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab, 2005;90:1294-1301.
- 14. Park JG, Song KS, Jung HJ, Lee JS, Lee TJ, Kim KS. Bilateral femoral subtrochanteric insufficiency fractures after long-term bisphosphonate therapy. J Korean Orthop Assoc, 2010;45:146-150.
- 15. Puah KL, Tan MH. Bisphosphonate-associated atypical fracture of the femur: spontaneous healing with drug holiday and re-appearance after resumed drug therapy with bilateral simultaneous displaced fractures--a case report. Acta Orthop, 2011;82:380-382.
- 16. Rodan GA, Reszka AA. Osteoporosis and bisphosphonates. J Bone Joint Surg Am, 2003;85:Suppl 3. 8-12.
- 17. Russell RG, Watts NB, Ebetino FH, Rogers MJ. Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int, 2008;19:733-759.PDF
- 18. Shane E, Burr D, Ebeling PR, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res, 2010;25:2267-2294.
- 19. Wasserman N, Yerramshetty J, Akkus O. Microcracks colocalize within highly mineralized regions of cortical bone tissue. Eur J Morphol, 2005;42:43-51.
REFERENCES
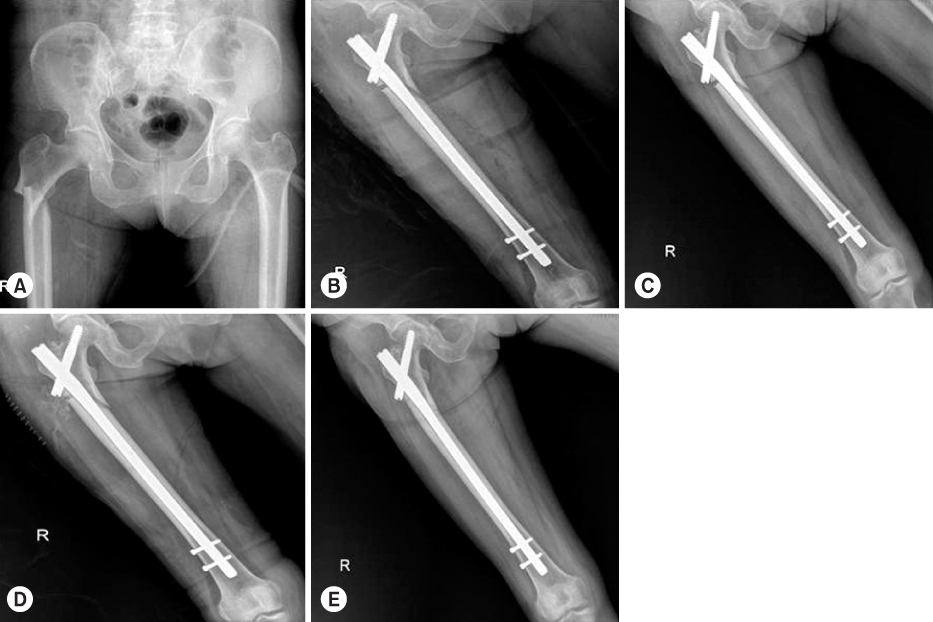
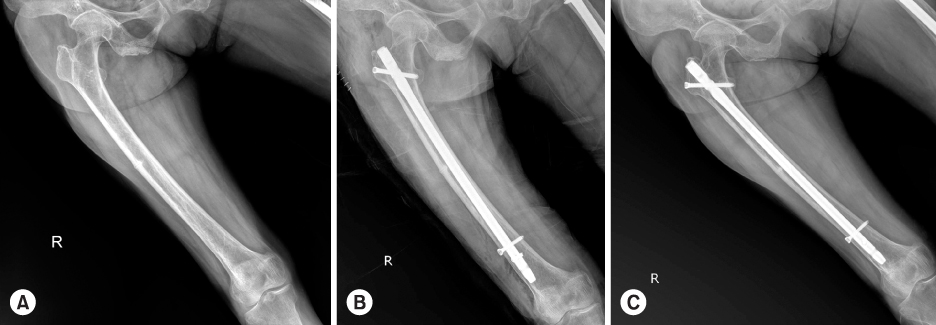
Figure & Data
REFERENCES
Citations

- Subtrochanteric Fracture Reduction during Intramedullary Nailing: Technical Note
Gyu Min Kong
Journal of the Korean Fracture Society.2019; 32(2): 107. CrossRef
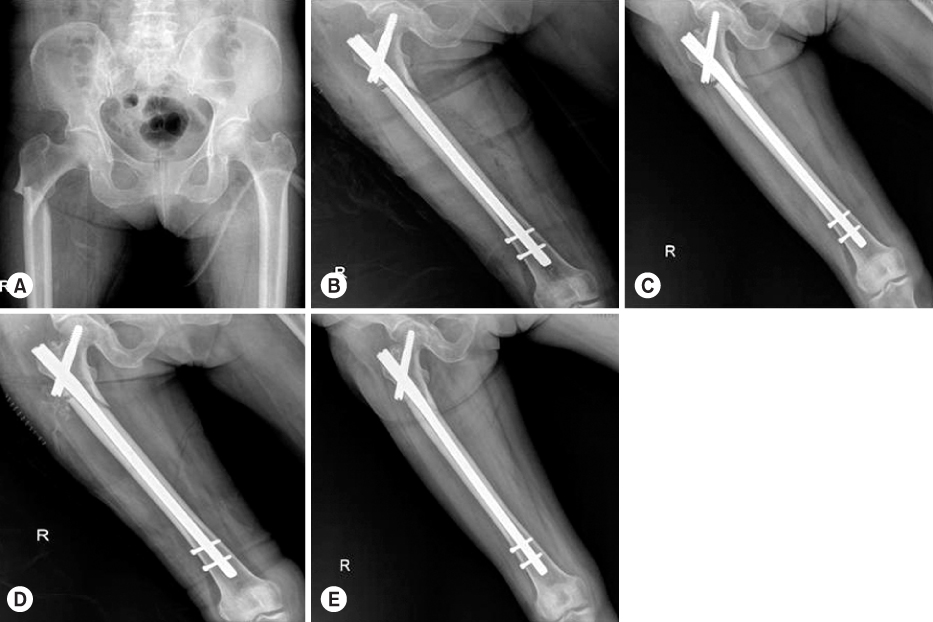

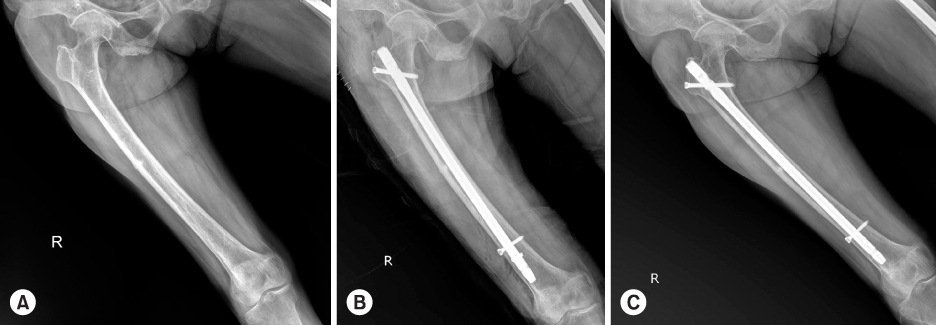
Fig. 1
Fig. 2
Fig. 3
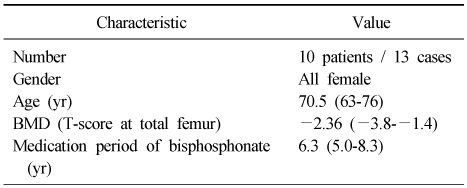
Baseline Characteristics of the Patient
Values are presented as median (range). BMD: Bone mineral density.
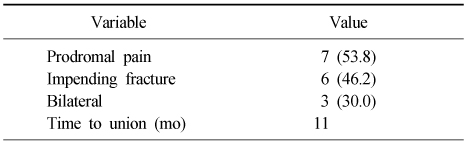
Character of Insufficiency Fracture
Values are presented as number (%) or only number.
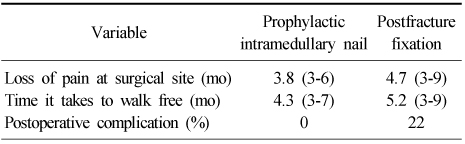
Comparison of Prophylactic Fixation and Postfracture Fixation
Values are presented as median (range) or percent.
Values are presented as median (range). BMD: Bone mineral density.
Values are presented as number (%) or only number.
Values are presented as median (range) or percent.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

