Abstract
-
Background
Cubitus varus deformity in adults most commonly occurs as a late complication resulting from malunion of distal humeral fractures sustained during childhood. This deformity can cause cosmetic problems and anatomical deformities that hinder normal sports activities and potentially lead to long-term complications. Although various surgical techniques exist for correcting cubitus varus, this study investigated the clinical and functional outcomes of reverse V step-cut osteotomy.
-
Methods
In total, 15 patients underwent surgical treatment with reverse V step-cut osteotomy between 2012 and 2023. The mean age of the patients at the time of surgery was 46.3 years (range, 20–65 years). The preoperative carrying angle was ‒11.09° of varus, which was corrected to +12.81° of valgus postoperatively. The mean preoperative lateral prominence index (LPI) was ‒10.03, and the mean postoperative LPI improved to ‒4.48. A comparison to the unaffected side showed a P-value of 0.978, indicating similarity.
-
Results
Preoperatively, eight patients exhibited signs of posterolateral rotatory instability, and among them, three underwent concomitant lateral ulnar collateral ligament reconstruction. Seven patients reported ulnar nerve symptoms, and all underwent concurrent ulnar nerve release. Postoperatively, improvements in elbow pain, instability, and ulnar nerve symptoms were observed. One patient required reoperation due to malunion and insufficient correction, but no other complications were noted.
-
Conclusions
These outcomes demonstrate that reverse V step-cut osteotomy can be an effective treatment method for cubitus varus deformity in adults.
-
Level of evidence
IV.
-
Keywords: Elbow joint, Abnormalities, Joint instability, Osteotomy, Methods
Introduction
Varus deformity of the elbow in adults is most commonly caused by malunion of distal humerus fractures during childhood and is recognized as one of the most frequent late complications [
1], with a reported prevalence ranging from approximately 3% to 57% [
2]. While surgical correction is primarily considered for cosmetic reasons, the varus and internal rotation deformities of the elbow can also hinder normal sports activities. Additionally, long-term complications, snapping triceps syndrome [
3], posterolateral rotatory instability (PLRI) of the elbow, and ulnar neuropathy may develop [
4].
PLRI, a late complication, occurs when varus deformity generates a moment arm that induces external rotation due to triceps contraction. Repeated exposure to this abnormal torque causes stretching of the lateral collateral ligament complex, leading to excessive external rotation of the ulna relative to the humerus, ultimately initiating lateral rotatory instability. Consequently, patients may experience lateral elbow pain and recurrent instability. Prolonged instability over time can further lead to the development of arthritis [
3,
5,
6].
Ulnar nerve symptoms are hypothesized to result from various factors. Instability of the ulnar nerve caused by the internal rotation deformity of the elbow may be a contributing factor. Additionally, snapping or anteromedial displacement of the medial head of the triceps could compress the ulnar nerve, or a fibrous band located between the two heads of the flexor carpi ulnaris might irritate the nerve. These factors can collectively lead to tardy ulnar nerve palsy [
7]. In adults, surgical treatment may be required not only for cosmetic reasons but also to address these late complications.
Various supracondylar osteotomy techniques have been introduced for the surgical correction of varus deformity, including medial opening-wedge osteotomy, lateral closing-wedge osteotomy, three-dimensional osteotomy, and oblique osteotomy. However, the supracondylar region of the humerus is anatomically characterized by thin bony structures, making it challenging to maintain stable internal fixation. Due to these structural limitations, complications such as nonunion at the osteotomy site, recurrence of the deformity, and restriction of elbow range of motion have been reported following surgical treatment [
8-
10]. In 2004, Yun et al. [
11] introduced the reverse V-shaped step-cut osteotomy technique, which has been studied in pediatric populations. However, there is a lack of research on its application in adults. Therefore, this study aims to evaluate the clinical utility of reverse V-shaped step-cut osteotomy in adult patients.
Methods
Ethics Statement
The study was approved by the Institutional Review Board (IRB) of Haeundae Paik Hospital (IRB No. 2024-09-016-003) and conducted in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants, including consent for the use of clinical images.
Study Population
This study included 15 adult patients who underwent reverse V-shaped step-cut osteotomy, between 2012 and 2023. The patients' ages at the time of surgery ranged from 20 to 65 years, with a mean age of 46.3 years. The average follow-up period was 18 months.
Various methods exist for measuring varus deformity; however, this study employed the humeral-elbow-wrist angle (
Fig. 1), as it was suggested by Oppenheim et al. [
10] to most closely approximate the actual carrying angle (CA). This angle was measured on plain radiographs with the elbow fully extended and the forearm in external rotation. Varus angles were indicated with a negative (‒) sign, while valgus angles were denoted with a positive (+) sign.
Additionally, the lateral prominence index (LPI) (
Fig. 2) was measured and compared before and after surgery. The LPI represents the degree of medial and lateral protrusion relative to the humeral axis. It was calculated as the ratio of the distances measured from the most prominent medial and lateral points to the humeral axis on anteroposterior plain radiographs.
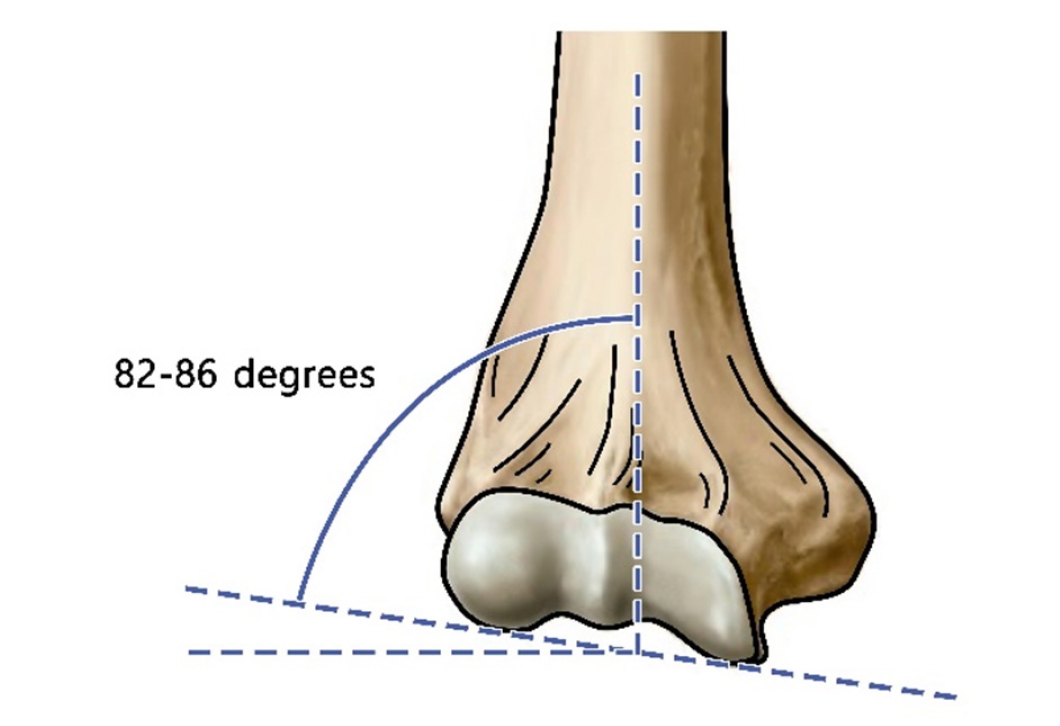
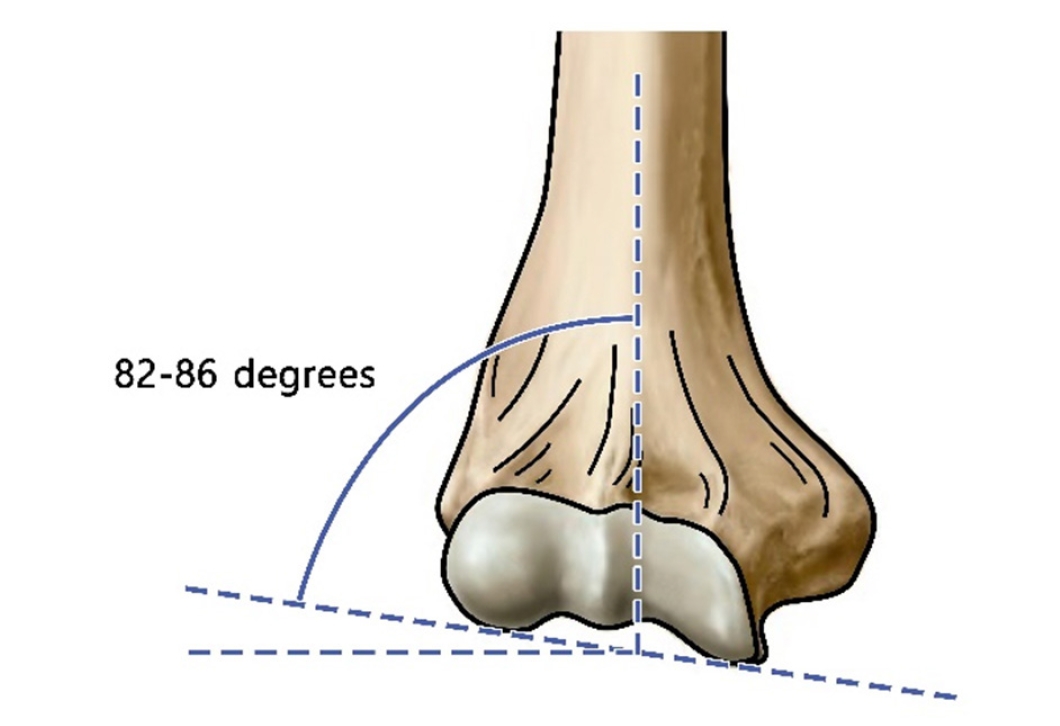
Furthermore, to evaluate the deformity of humerus itself, the distal humerus carrying angle (DHCA) was measured and compared. The DHCA is defined as the angle formed between the line connecting the trochlea and the capitellum of the humerus and the humeral axis (
Fig. 3).
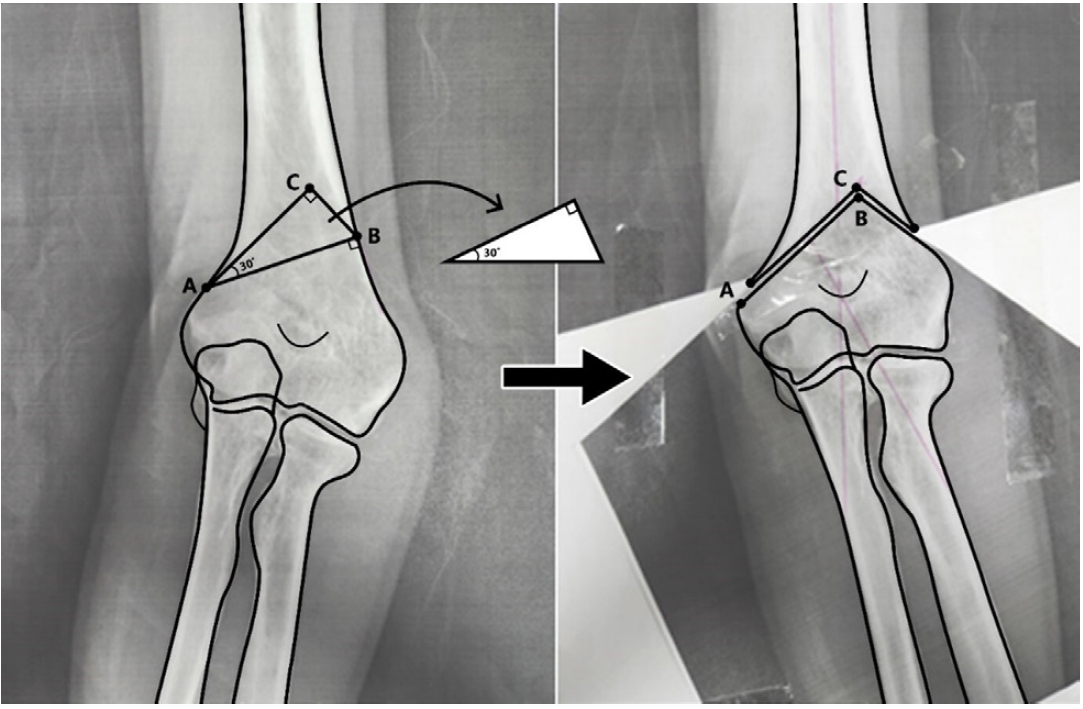
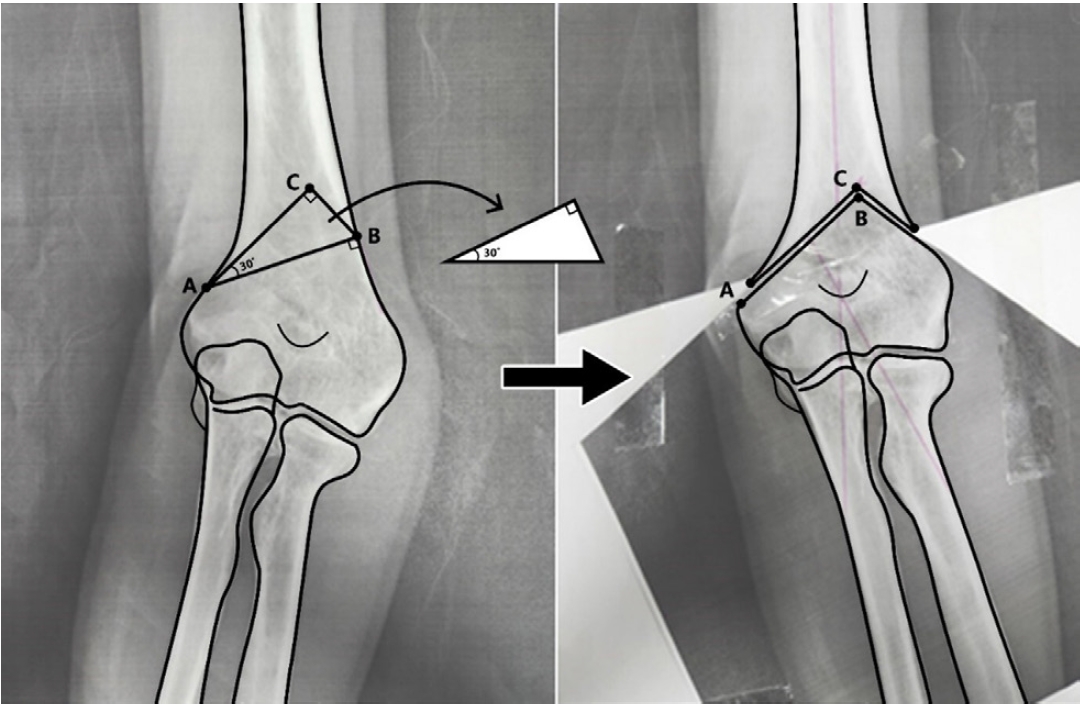
The preoperative osteotomy plan involved the following steps. First, point B was identified based on preoperative radiographs (
Fig. 4). Point B was defined as a location sufficiently proximal to the origin of the common extensor tendon at the lateral epicondyle, approximately 1 cm proximal to the olecranon fossa, and perpendicular to the lateral supracondylar ridge when it appears linear.
Point A was established by drawing a perpendicular line from point B to the radial border, where this line intersects the ulnar border. Point A is located proximal to the medial epicondyle. A right-angled triangle representing the target correction angle was then constructed, with the apex of the triangle designated as point C.
The right-angled triangle determined the area for osteotomy, and the osteotomy was performed such that the angle between line AB and the radial border was aligned at point C. Following the osteotomy, the distal humerus was rotated laterally and shifted medially so that points B and C met, completing the correction plan.
Surgical Technique
The surgery began with a posterior approach. Access to the posterior humerus was achieved using either a triceps-splitting or triceps-preserving approach. The preoperatively determined ABC points were marked with an electrocautery device, and the osteotomy was initiated along line AB. The osteotomized humerus was supported anteriorly to protect the neurovascular structures. Subsequently, osteotomies were performed along lines AC and BC to complete the procedure. To prevent interference with bone healing, decortication of the lateral distal cortical ridge was performed before insertion into the osteotomy site. After correcting the varus deformity, temporary fixation was achieved using K-wires, followed by definitive fixation with a metal plate and screws (
Fig. 5). The final correction angle was ensured through preoperative templating and intraoperative confirmation with fluoroscopy.
Results
All 15 patients (
Table 1) achieved bone union within an average of 1.1 years. Patient no. 2 in
Table 1 required reoperation due to persistent elbow pain and a positive varus stress test, which indicated insufficient correction and malunion. No other complications were observed in the remaining patients.
The mean preoperative CA was varus 11.09°, while the mean postoperative CA was valgus 12.81°. The Wilcoxon signed-rank test revealed a statistically significant correction (P<0.001). Additionally, the postoperative CA showed no significant difference from the contralateral, unaffected side (14.69°; P=0.33), indicating a comparable outcome.
The mean preoperative LPI was –10.03, while the mean postoperative LPI improved to –4.48. When comparing the postoperative LPI with that of the contralateral, unaffected side, the P-value was 0.978, indicating that the postoperative LPI closely approximated the LPI of the unaffected side.
The mean preoperative DHCA was 110.59°, which significantly decreased to a mean of 85.19° postoperatively. Statistical analysis revealed a significant difference between pre- and postoperative DHCA (P < 0.001). Additionally, the mean DHCA of the contralateral, unaffected side was 84.33°, and the comparison with the postoperative DHCA yielded a P-value of 0.978, indicating no significant difference. Thus, the DHCA showed a significant improvement postoperatively and became comparable to that of the unaffected side.
Among the 15 patients, seven reported ulnar nerve symptoms. Ulnar nerve release was performed in conjunction with the osteotomy for these patients, and all experienced symptomatic improvement following surgery.
Preoperative under-anesthesia examination revealed positive findings in the pivot shift test, a diagnostic test for PLRI, in eight patients. Among these, seven patients underwent concomitant lateral ulnar collateral ligament (LUCL) reconstruction. Postoperatively, no patients reported elbow instability or instability-related pain.
Discussion
Varus deformity can cause not only cosmetic concerns but also functional issues, such as PLRI and ulnar nerve symptoms [
6,
7]. In this study, eight out of 15 patients exhibited signs of PLRI, and three of these patients underwent concomitant LUCL reconstruction. According to O’Driscoll et al. [
6]'s research, varus deformity can lead to PLRI, and osteotomy is recommended for patients with a deformity angle exceeding 15°. Postoperatively, patients with PLRI symptoms experienced improvement in elbow pain and instability symptoms. Additionally, seven patients reported ulnar nerve symptoms, and all of them underwent ulnar nerve release. Even without anterior transposition of the ulnar nerve, correction via osteotomy and ulnar nerve release alone led to symptomatic improvement after surgery.
Several osteotomy techniques have been developed to correct varus deformity. Among these, lateral closing-wedge osteotomy is the most widely used due to its technical simplicity, ability to achieve substantial angular correction, and simultaneous correction of rotational deformities. However, major studies in the past have reported a relatively high complication rate, ranging from 24% to 47% [
10,
12,
13]. Additionally, since lateral closing-wedge osteotomy relies on a medial hinge, it has the drawback of potentially insufficiently correcting or even exacerbating the lateral prominence commonly associated with varus deformity [
4,
14]. Medial opening-wedge osteotomy has the disadvantage of being prone to instability at the osteotomy site and a higher risk of ulnar nerve injury, often necessitating ulnar nerve anterior transposition [
15]. In addition, techniques such as dome osteotomy [
16,
17], and oblique osteotomy [
18,
19] have also been reported.
The reverse V-shaped step-cut osteotomy used in this study allows for osteotomy to be performed near the center of rotation of angulation, enabling correction of the varus deformity through rotation. This approach also has the advantage of improving lateral prominence [
1,
11]. Indeed, a comparison of the LPI before and after surgery revealed a significant improvement. Additionally, compared to lateral closing-wedge osteotomy, the reverse V-shaped step-cut osteotomy provides a larger contact area after osteotomy, facilitating bone union. Furthermore, compared to the standard V-shaped step-cut osteotomy, the reverse approach offers a larger distal fragment, increasing the area available for fixation. The post-osteotomy structure forms a triangular column, anchored by the dense bone of the proximal segment, enhancing fixation [
12,
20].
However, the reverse V-shaped step-cut osteotomy may not be suitable for large angular corrections, as its right triangle design imposes geometric constraints. If the required correction angle exceeds the medial ridge extension and perpendicular to the lateral ridge, this method becomes impractical. Indeed, in this study, one case initially planned for this technique required a lateral closing-wedge osteotomy instead.
This study has several limitations. First, its retrospective design and small sample size limit the generalizability of the findings. Additionally, the absence of a comparative group using different osteotomy techniques restricts the ability to draw broader conclusions. Another limitation is the lack of preoperative functional assessments, making it difficult to fully evaluate the procedure's impact on functional recovery. Future research should include a larger cohort and longitudinal follow-up to track functional outcomes over time rather than relying on single-timepoint evaluations.
Conclusions
Reverse V step-cut osteotomy is a viable surgical option for adult cubitus varus correction, yielding significant improvements in anatomical alignment and functional outcomes. However, further research with larger cohorts and comparative studies is necessary to establish its broader clinical application.
Article Information
-
Author contributions
Conceptualization: HJK. Investigation: HJK. Methodology: JYB. Project administration: JYB. Visualization: JYB. Writing-original draft: HJK. Writing-review & editing: HJK, JYB. All authors read and approved the final manuscript.
-
Conflict of interests
None.
-
Funding
None.
-
Data availability
Contact the corresponding author for data availability.
Fig. 1.The humeral-elbow-wrist angle, which is defined as the angle of intersection of the humeral shaft line and the forearm line.

Fig. 2.The lateral prominence index (%), which is defined using the following formula: (BC‒AC)/AB×100. A, medial prominence; B, cross-link between a line connecting the lateral prominence; C, mid longitudinal axis of the humerus.

Fig. 3.The distal humerus carrying angle, which is defined as the angle formed between the line connecting the trochlea and the capitellum of the humerus and the humeral axis.
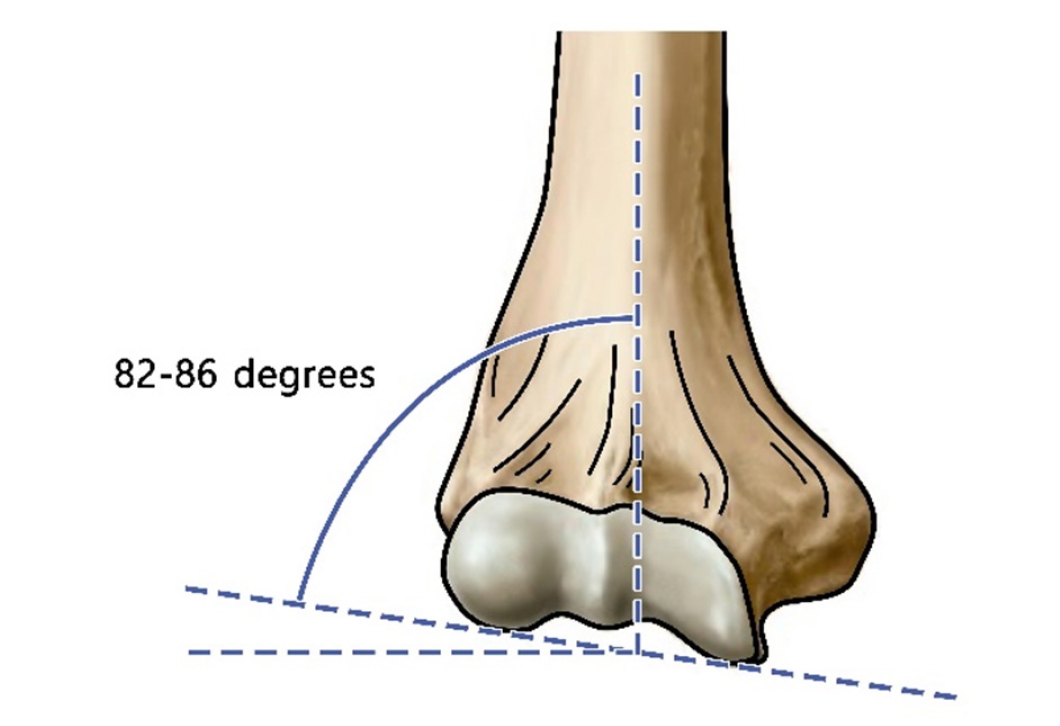
Fig. 4.Preoperative planning: line AB is drawn perpendicular to the lateral supracondylar ridge, positioned more than 1 cm above the olecranon fossa. The angle CAB represents the correction angle. After the triangle ABC is removed, point B is adjusted to meet point C.
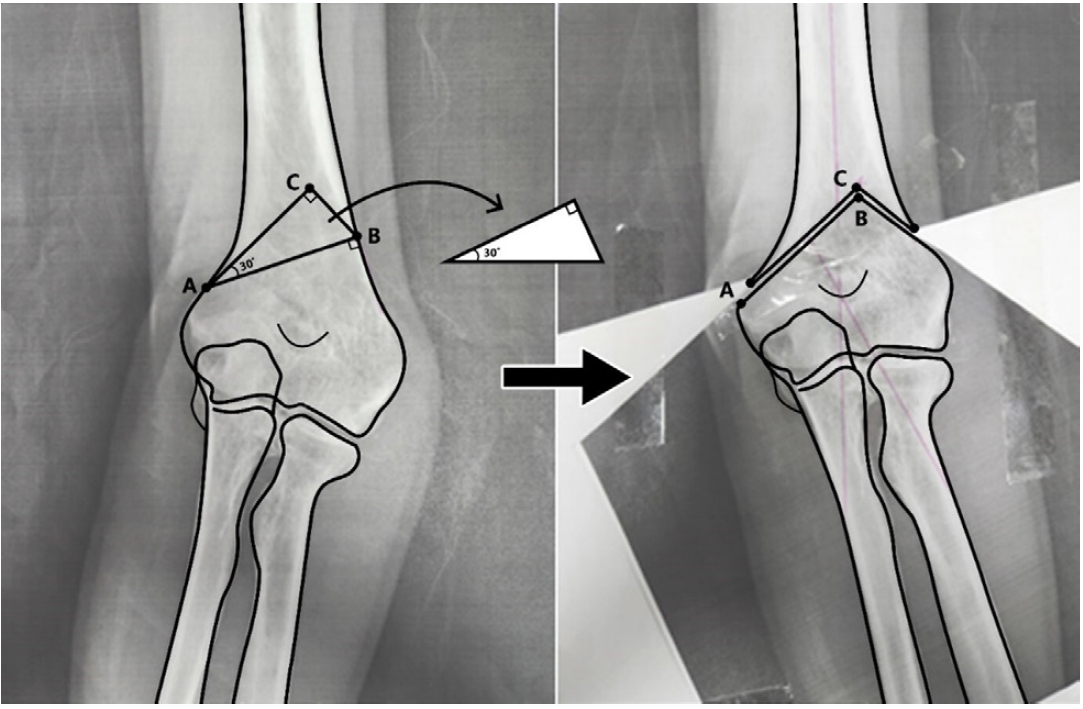
Fig. 5.A 62-year-old male patient (patient 3) who presented with a cubitus varus deformity: preoperative and postoperative clinical photographs and radiographs.

Table 1.Data of patients with cubitus varus deformity treated with reverse V step-cut osteotomy
|
Case |
Sex |
Age (yr) |
Preop CA
|
Postop CA |
LPI
|
Preop DHCA
|
Postop DHCA |
|
Injured |
Uninjured |
Uninjured |
Postop |
Injured |
Uninjured |
|
1 |
M |
63 |
‒2.4 |
12.1 |
12.8 |
‒10.50 |
2.91 |
92.7 |
82.1 |
81.5 |
|
2 |
F |
26 |
‒11.8 |
7.9 |
19.9 |
‒8.08 |
‒18.79 |
103.9 |
88.1 |
80.6 |
|
3 |
M |
62 |
‒7.6 |
18.5 |
7.3 |
‒10.89 |
‒27.74 |
115.5 |
82.4 |
105.8 |
|
4 |
F |
38 |
‒4.9 |
15.9 |
15.6 |
‒3.43 |
‒9.19 |
100.3 |
82.0 |
77.4 |
|
5 |
F |
49 |
‒14.9 |
21.6 |
8.1 |
2.35 |
‒2.64 |
115.9 |
84.3 |
88.1 |
|
6 |
M |
20 |
‒10.4 |
12.1 |
5.9 |
‒1.68 |
‒2.81 |
112.6 |
87.6 |
86.1 |
|
7 |
M |
22 |
‒9.1 |
15.0 |
11.7 |
‒9.78 |
‒4.52 |
107.9 |
87.6 |
86.5 |
|
8 |
M |
51 |
‒19.2 |
12.9 |
1.4 |
‒3.37 |
5.81 |
113.6 |
89.1 |
96.7 |
|
9 |
M |
65 |
‒25.6 |
9.3 |
5.4 |
3.96 |
‒11.62 |
120.0 |
84.5 |
86.4 |
|
10 |
M |
47 |
5.0 |
12.3 |
18.2 |
6.95 |
12.22 |
89.3 |
83.6 |
77.8 |
|
11 |
M |
59 |
‒22.9 |
14.9 |
14.6 |
‒3.35 |
19.24 |
124.2 |
81.0 |
85.3 |
|
12 |
F |
65 |
‒6.9 |
19.2 |
19.2 |
‒17.72 |
‒9.08 |
115.7 |
85.4 |
87.2 |
|
13 |
F |
33 |
‒0.2 |
15.2 |
20.5 |
‒6.13 |
‒6.79 |
107.8 |
82.4 |
71.8 |
|
14 |
M |
31 |
‒15.3 |
15.1 |
18.2 |
‒13.05 |
‒9.16 |
120.3 |
80.5 |
78.4 |
|
15 |
M |
64 |
‒20.2 |
18.3 |
13.5 |
‒15.36 |
‒10.40 |
119.1 |
84.3 |
88.6 |
References
- 1. Khurana A, Kumar N, Chugh V, Pattabiraman K, Singh J, Verma G. A systematic review of techniques for step cut osteotomy in cubitus varus: a comprehensive analysis. J Orthop 2023;49:81-9.ArticlePubMedPMC
- 2. Tellisi N, Abusetta G, Day M, Hamid A, Ashammakhi N, Wahab KH. Management of Gartland's type III supracondylar fractures of the humerus in children: the role audit and practice guidelines. Injury 2004;35:1167-71.ArticlePubMed
- 3. Kontogeorgakos VA, Mavrogenis AF, Panagopoulos GN, Lagaras A, Koutalos A, Malizos KN. Cubitus varus complicated by snapping medial triceps and posterolateral rotatory instability. J Shoulder Elbow Surg 2016;25:e208-12.ArticlePubMed
- 4. Kumar R, Rangasamy K, Raj Gopinathan N, Sudesh P, Goni VG. Is modified reverse step-cut osteotomy better than Yun's reverse V osteotomy in paediatric cubitus varus deformity correction? A prospective, double-blinded, randomized controlled trial. Int Orthop 2022;46:2041-53.ArticlePubMedPDF
- 5. Seo SG, Gong HS, Lee YH, Rhee SH, Lee HJ, Baek GH. Posterolateral rotatory instability of the elbow after corrective osteotomy for previously asymptomatic cubitus varus deformity. Hand Surg 2014;19:163-9.ArticlePubMed
- 6. O'Driscoll SW, Spinner RJ, McKee MD, et al. Tardy posterolateral rotatory instability of the elbow due to cubitus varus. J Bone Joint Surg Am 2001;83:1358-69.ArticlePubMed
- 7. Jeon IH, Oh CW, Kyung HS, Park IH, Kim PT. Tardy ulnar nerve palsy in cubitus varus deformity associated with ulnar nerve dislocation in adults. J Shoulder Elbow Surg 2006;15:474-8.ArticlePubMed
- 8. Bellemore MC, Barrett IR, Middleton RW, Scougall JS, Whiteway DW. Supracondylar osteotomy of the humerus for correction of cubitus varus. J Bone Joint Surg Br 1984;66:566-72.ArticlePubMedPDF
- 9. Labelle H, Bunnell WP, Duhaime M, Poitras B. Cubitus varus deformity following supracondylar fractures of the humerus in children. J Pediatr Orthop 1982;2:539-46.ArticlePubMed
- 10. Oppenheim WL, Clader TJ, Smith C, Bayer M. Supracondylar humeral osteotomy for traumatic childhood cubitus varus deformity. Clin Orthop Relat Res 1984;188:34-9.Article
- 11. Yun YH, Shin SJ, Moon JG. Reverse V osteotomy of the distal humerus for the correction of cubitus varus. J Bone Joint Surg Br 2007;89:527-31.ArticlePubMedPDF
- 12. DeRosa GP, Graziano GP. A new osteotomy for cubitus varus. Clin Orthop Relat Res 1988;236:160-5.Article
- 13. Gong MQ, Jiang XY, Wang MY. Treatment of cubitus varus deformity in adults with lateral closing wedge osteotomy. Zhonghua Yi Xue Za Zhi 2006;86:2201-4.PubMed
- 14. Wong HK, Lee EH, Balasubramaniam P. The lateral condylar prominence: a complication of supracondylar osteotomy for cubitus varus. J Bone Joint Surg Br 1990;72:859-61.ArticlePubMedPDF
- 15. King D, Secor C. Bow elbow (cubitus varus). J Bone Joint Surg Am 1951;33A:572-6.Article
- 16. Tien YC, Chih HW, Lin GT, Lin SY. Dome corrective osteotomy for cubitus varus deformity. Clin Orthop Relat Res 2000;380:158-66.Article
- 17. Hahn SB, Choi YR, Kang HJ. Corrective dome osteotomy for cubitus varus and valgus in adults. J Shoulder Elbow Surg 2009;18:38-43.ArticlePubMed
- 18. Mahaisavariya B, Laupattarakasem W. Osteotomy for cubitus varus: a simple technique in 10 children. Acta Orthop Scand 1996;67:60-2.ArticlePubMed
- 19. Laupattarakasem W, Mahaisavariya B, Kowsuwon W, Saengnipanthkul S. Pentalateral osteotomy for cubitus varus: clinical experiences of a new technique. J Bone Joint Surg Br 1989;71:667-70.ArticlePubMedPDF
- 20. Schlauch AM, Manske MC, Leshikar HB, Davids JR. Posttraumatic cubitus varus: respect the columns. J Pediatr Orthop 2024;44:e518-29.ArticlePubMed
 , Hyung Jun Koo, MD
, Hyung Jun Koo, MD








 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

