Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 21(2); 2008 > Article
-
Original Article
- The Results of Surgical Treatment for Nonunion of Phalanges in the Hand
- Hee Dong Kim, M.D., Yoon Hong Kim, M.D., Yong Soo Choi, M.D., Heun Guyn Jung, M.D.
-
Journal of the Korean Fracture Society 2008;21(2):140-144.
DOI: https://doi.org/10.12671/jkfs.2008.21.2.140
Published online: April 30, 2008
Department of Orthopaedic Surgery, Kwangju Christian Hospital, Gwangju, Korea.
- Address reprint requests to: Heun Guyn Jung, M.D. Department of Orthopaedic Surgery, Kwangju Christian Hospital, 264, Yangrim-dong, Nam-gu, Gwangju 503-715, Korea. Tel: 82-62-650-5064, Fax: 82-62-650-5066, handmicro@naver.com
Copyright © 2008 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 455 Views
- 3 Download
Abstract
-
Purpose
- To evaluate the results of internal fixation and autogenous bone graft for the phalangeal nonunion in the hand.
-
Materials and Methods
- From Feb. 2000 until May 2006, thirteen cases that had been treated for non-union of phalanges in the hand were investigated retrospectively. Seven cases were treated with mini-plate fixation and autogenous cancellous graft and six cases with Kirschner wire fixation and autogenous cancellous graft. We analyzed bony union period radiographically and clinical results according to Belsky's score.
-
Results
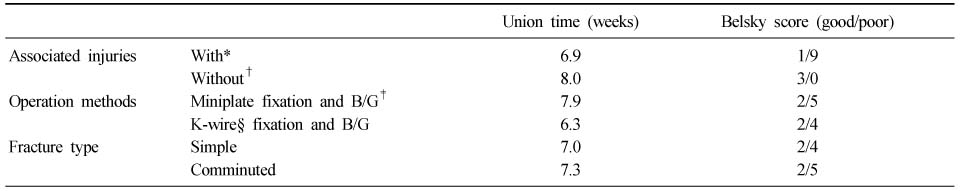
- Thirteen cases obtained bony union. Seven cases of mini-plate fixation and bone graft, and six cases of K-wire fixation and bone graft achieved the bony union postoperatively on average 7.9 weeks and 6.3 weeks, respectively. Clinical results were "good" in four cases and "poor" in nine cases according to the Belsky's score. Only one of ten cases with associated injuries, such as tendon, nerve, arterial injuries and other finger fractures in the injured hand, had the good clinical result, but all three cases without associated injuries had the good one.
-
Conclusion
- Internal fixation and autogenous bone graft can be a successful treatment of phalangeal nonunion. However, more careful choice of surgical treatment methods and preoperative explanation of poor post-operative results or complications should be made for phalangeal nonunion with associated injuries in the finger because of poor outcome in those cases.
- 1. Barton NJ. Fractures of the shafts of the phalanges of the hand. Hand, 1979;11:119-133.ArticlePDF
- 2. Belsky MR, Eaton RG, Lane LB. Closed reduction and internal fixation of proximal phalangeal fractures. J Hand Surg Am, 1984;9:725-729.Article
- 3. Borgeskov S. Conservative treatment of phalangeal and metacarpal fractures. Ugeskr Laeger, 1967;129:349-353.
- 4. Boyd HB, Lipinski SW, Wiley JH. Observation on non-union of the shafts of the long bones, with statistiscal analysis of 842 patients. J Bone Joint Surg Am, 1961;43:159-168.
- 5. Jupiter JB, Koniuch MP, Smith RJ. The management of delayed union and nonunion of the metacarpals and phalanges. J Hand Surg Am, 1985;10:457-466.
- 6. Littler JW. Metacarpal reconstruction. J Bone Joint Surg Am, 1947;29:723-737.
- 7. Patankar H, Patwardhan D. Nonunion in a fracture of the proximal phalanx of the thumb. J Orthop Trauma, 2000;14:219-222.Article
- 8. Ring D. Malunion and nonunion of the metacarpals and phalanges. Instr Course Lect, 2006;55:121-128.Article
- 9. Van Oosterom FJ, Brete GJ, Ozdemir C, Hovius SE. Treatment of phalangeal fractures in severely injured hands. J Hand Surg Br, 2001;26:108-111.ArticlePDF
REFERENCES
A 36-year-old man sustained proximal phalanx fracture of the thumb and K-wires fixation was done at local clinic. At the time of injury of the hand, associated injury was not detected.

A 26-year-old man sustained the multiple comminuted fractures of the left hand in a motor vehicle accident. Degloving wound in the dorsum of the hand and third phalangeal bony exposure were detected. And the injuries of extensor tendon and digital nerve of the left third finger were involved.

Demographic data of patients
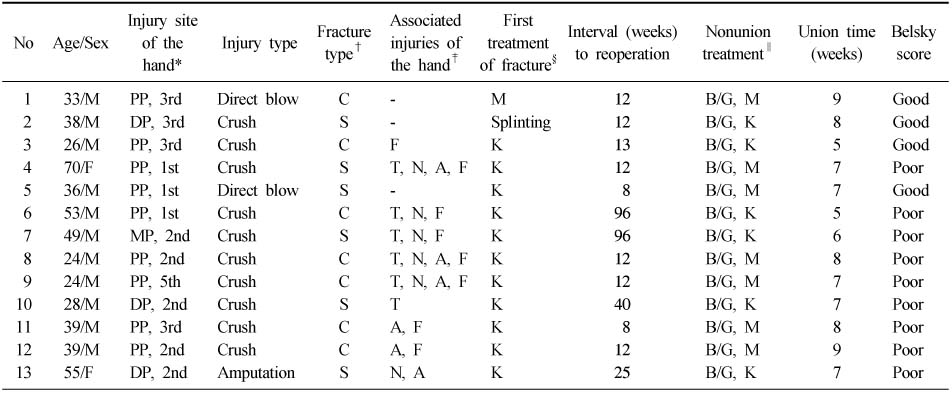
*PP: Proximal phalanx, MP: Middle phalanx, DP: Distal phalanx. 1st, 2nd, 3rd, 4th, and 5th means each fingers, †C: Comminuted fracture, S: Simple fracture, ‡T: Tendon injury, N: Nerve injury, A: Artery injury, F: Other finger fracture in the injured hand, §M: Miniplate fixation, K: Kirschner wire fixation, ∥B/G: Autogenous bone graft.
Figure & Data
REFERENCES
Citations



Fig. 1
Fig. 2
Demographic data of patients
*PP: Proximal phalanx, MP: Middle phalanx, DP: Distal phalanx. 1st, 2nd, 3rd, 4th, and 5th means each fingers, †C: Comminuted fracture, S: Simple fracture, ‡T: Tendon injury, N: Nerve injury, A: Artery injury, F: Other finger fracture in the injured hand, §M: Miniplate fixation, K: Kirschner wire fixation, ∥B/G: Autogenous bone graft.
Relationships of associated injuries, treatment methods and fracture type to bony union time and clinical results
*With: Group with the associated injury, †Without: Group without the associated injury, ‡B/G: Autogenous bone graft, §K-wire: Kirschner wire.
*PP: Proximal phalanx, MP: Middle phalanx, DP: Distal phalanx. 1st, 2nd, 3rd, 4th, and 5th means each fingers, †C: Comminuted fracture, S: Simple fracture, ‡T: Tendon injury, N: Nerve injury, A: Artery injury, F: Other finger fracture in the injured hand, §M: Miniplate fixation, K: Kirschner wire fixation, ∥B/G: Autogenous bone graft.
*With: Group with the associated injury, †Without: Group without the associated injury, ‡B/G: Autogenous bone graft, §K-wire: Kirschner wire.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

