Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 21(3); 2008 > Article
-
Original Article
- Anterolateral Thigh Island Flap
- Jae-Hoon Lee, M.D., Il-Hoen Choi, M.D.
-
Journal of the Korean Fracture Society 2008;21(3):207-212.
DOI: https://doi.org/10.12671/jkfs.2008.21.3.207
Published online: July 31, 2008
Department of Orthopaedic Surgery, East-West Neo Medical Center, College of Medicine, Kyunghee University, Seoul, Korea.
- Address reprint requests to: Jae-Hoon Lee, M.D. Department of Orthopaedic Surgery, East-West Neo Medical Center, College of Medicine, Kyunghee University, 149, Sangil-dong, Gangdong-gu, Seoul 134-090, Korea. Tel: 82-2-440-6153, Fax: 82-2-440-6296, ljhortho@yahoo.co.kr
Copyright © 2008 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 510 Views
- 0 Download
Abstract
-
Purpose
- To present the author's experience using the anterolateral thigh island flap for reconstruction of soft tissue defects around the hip and perineum.
-
Materials and Methods
- Proximal based anterolateral thigh island flaps were performed to reconstruct the soft tissue defects at the perineum (3 patients) and the greater trochanter of the hip (one patient) in 4 patients. All patients were male. Mean age was 43 years (range, 32 to 50 years) and mean follow-up was 8 months (range, 6 to 13 months). The causes of the defects were traffic accident in 2 cases, necrotizing fasciitis 1 case, and pressure sore 1 case. Average size of the flap was 14×9 cm. Fasciocutaneous flaps were performed in 3 patients and musculocutaneous flap was performed in one patient.
-
Results
- All flaps were survived. There were no necrosis of the flaps. One flap presented venous congestion after surgery, which resolved with the decompression of the pedicle. Reconstruction with the anterolateral thigh island flap resulted in no recurrence of the infection or ulcer and good esthetic contour.
-
Conclusion
- The anterolateral thigh island flap is a reliable flap for reconstruction around the perineum and hip joint.
- 1. Burke TW, Morris M, Roh MS, Levenback C, Gershenson DM. Perineal reconstruction using single gracilis myocutaneous flaps. Gynecol Oncol, 1995;57:221-225.
- 2. Chen CY, Hsieh CH, Kuo YR, Jeng SF. An anterolateral thigh perforator flap from the ipsilateral thigh for soft-tissue reconstruction around the knee. Plast Reconstr Surg, 2007;120:470-473.
- 3. Gravivanis AI, Tsoutsos DA, Karakitsos D, et al. Application of the pedicled anterolateral thigh flap to defects from the pelvis to the knee. Microsurgery, 2006;26:432-438.PDF
- 4. Hallock GG. The proximal pedicled anterolateral thigh flap for lower limb coverage. Ann Plast Surg, 2005;55:466-469.
- 5. Hsieh CH, Huang KF, Jeng SF, Tsai HH, Yang JC, Chiang YC. Reconstruction of open pelvic fracture skin defect with an anterolateral thigh island flap: a case report. J Trauma, 2007;62:1277-1280.
- 6. Jain AK, DeFranzo AJ, Marks MW, Loggie BW, Lentz S. Reconstruction of pelvic exenterative wounds with transpelvic rectus abdominis flaps: a case series. Ann Plast Surg, 1997;38:115-122.
- 7. Kimata Y, Uchiyama K, Sekido M, et al. Anterolateral thigh flap for abdominal wall reconstruction. Plast Reconstr Surg, 1999;103:1191-1197.
- 8. Lee JT, Cheng LF, Lin CM, Wang CH, Huang CC, Chien SH. A new technique of transferring island pedicled anterolateral thigh and vastus lateralis myocutaneous flaps for reconstruction of recurrent ischial pressure sores. J Plast Reconstr Aesthet Surg, 2007;60:1060-1066.
- 9. Luo S, Raffoul W, Piaget F, Egloff DV. Anterolateral thigh fasciocutaneous flap in the difficult perineogenital reconstruction. Plast Reconst Surg, 2000;105:171-173.
- 10. Pan SC, Yu JC, Shieh SJ, Lee JW, Huang BM, Chiu HY. Distally based anterolateral thigh flap: an anatomic and clinical study. Plast Reconstr Surg, 2004;114:1768-1775.
- 11. Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg, 1984;37:149-159.
- 12. Yildirim S, Avci G, Akan M, Misirlioğlu A, Akoz T. Anterolateral thigh flap in the treatment of postburn flexion contractures of the knee. Plast Reconstr Surg, 2003;111:1630-1637.
- 13. Yu P, Sanger JR, Matloub HS, Gosain A, Larson D. Anterolateral thigh fasciocutaneous island flaps in perineoscrotal recosntruction. Plast Reconstr Surg, 2002;109:610-616.
- 14. Zhou G, Zhang QX, Chen GY. The earlier clinic experience of the reverse-flow anterolateral thigh island flap. Br J Plast Surg, 2005;58:160-164.
REFERENCES
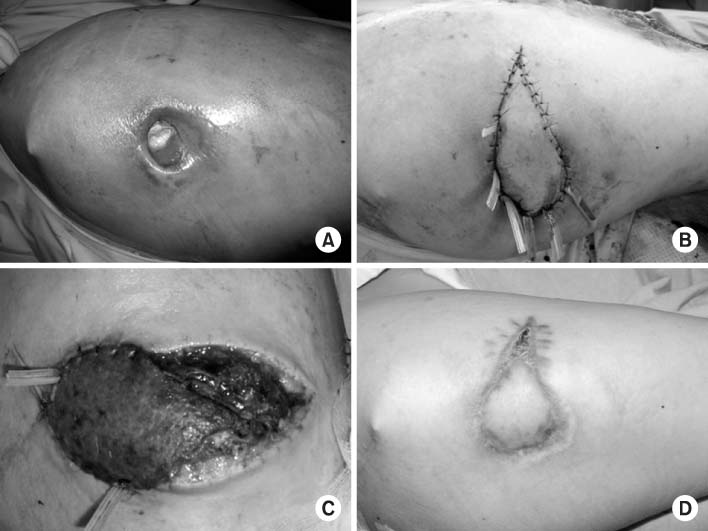
Fig. 1
(B) Design of the flap sized 12×9 cm at ipsilateral anterolateral thigh.
(C) The flap was raised as an island flap connected to the descending branch of the lateral circumflex femoral artery. The flap was transferred to cover the perineal defect.
(D) The flap had an acceptable contour and scar around perineum at 6 months follow-up.
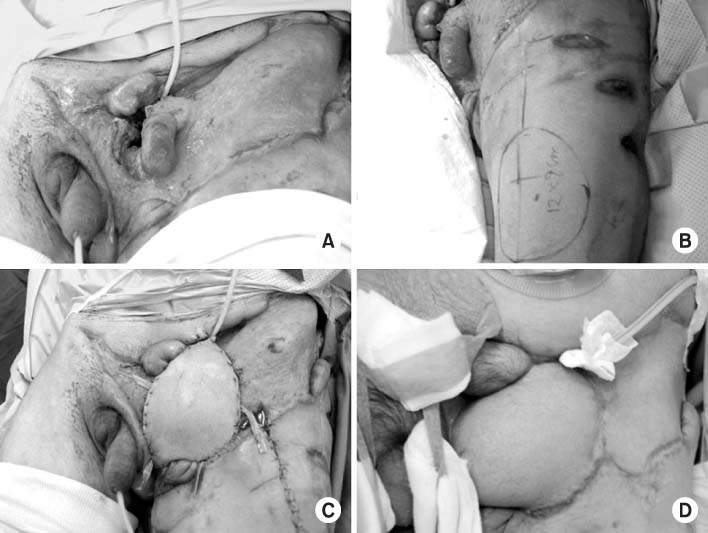
(A) Preoperative appearance of a 46-year-old man with a soft tissue defect of approximately 25×12 cm with the exposure of left scrotum in the left perineal area.
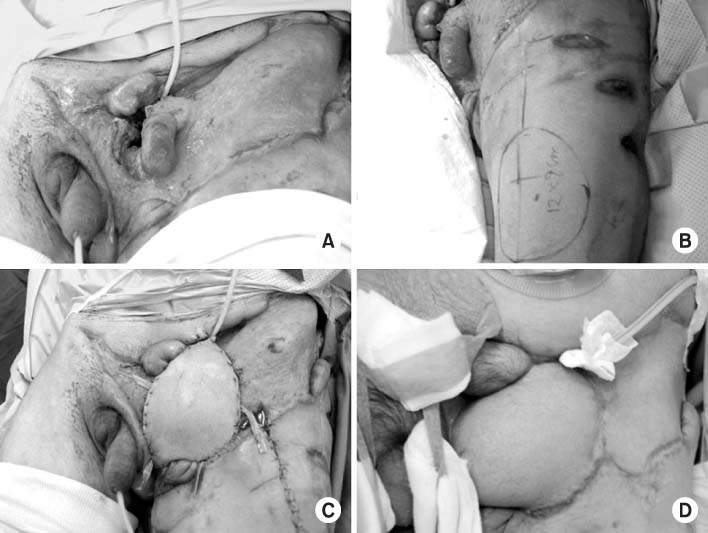
Fig. 2
(B) Soft tissue defect of a 25×15 cm in the perineal and suprapubic area was noted.
(C) The defect was covered with a 20×15 cm sized anterolateral thigh island flap.
(D) Acceptable contour and infection control around perineum was obtained after 9 months follow-up.
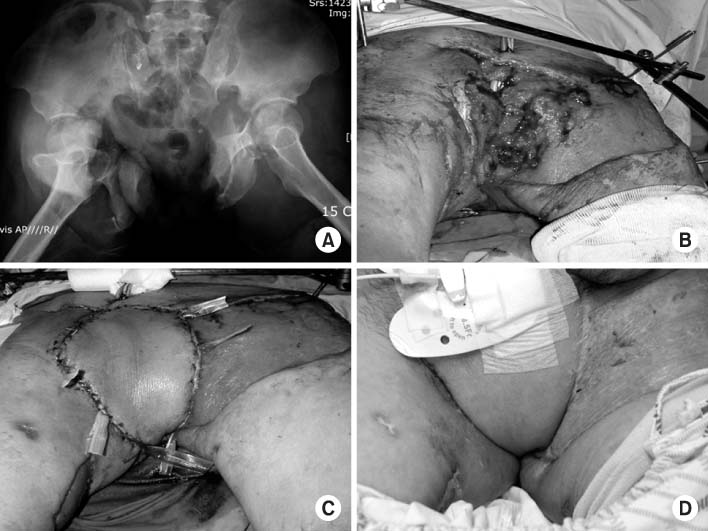
(A) Radiograph of acetabular and displaced open pelvic fracture (Tile type C2).
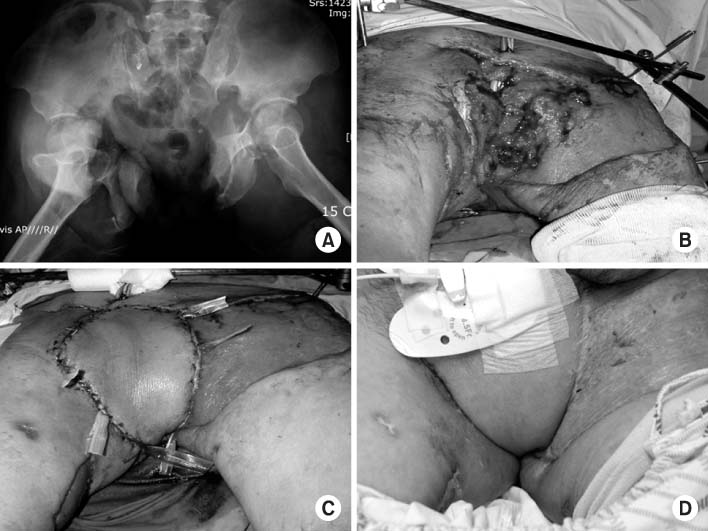
Fig. 3
(B) The island flap of 8×5 cm was raised from the right thigh and passed through a subcutaneous tunnel to cover the soft tissue defect.
(C) Two days after the operation, the venous congestion was noticed. The decompression of the vascular pedicle was done to resolve the venous insufficiency.
(D) The appearance of the flap 6 months after surgery.
(A) Pressure sore at the right greater trochanteric area in a paraplegia patient was noted.
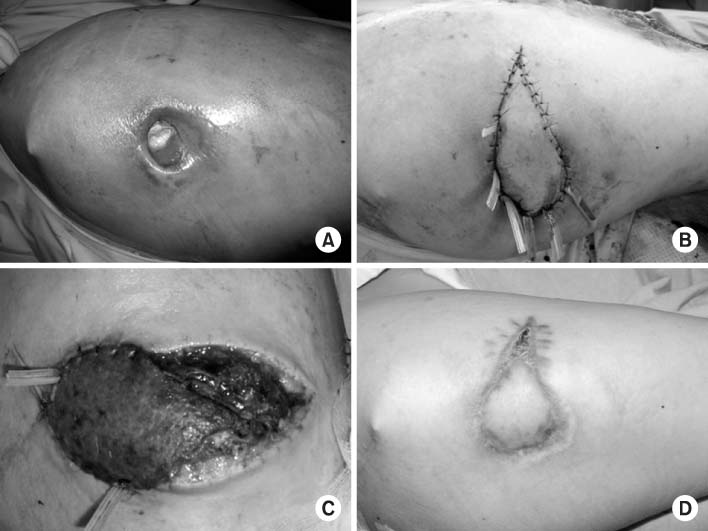
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

Anterolateral Thigh Island Flap
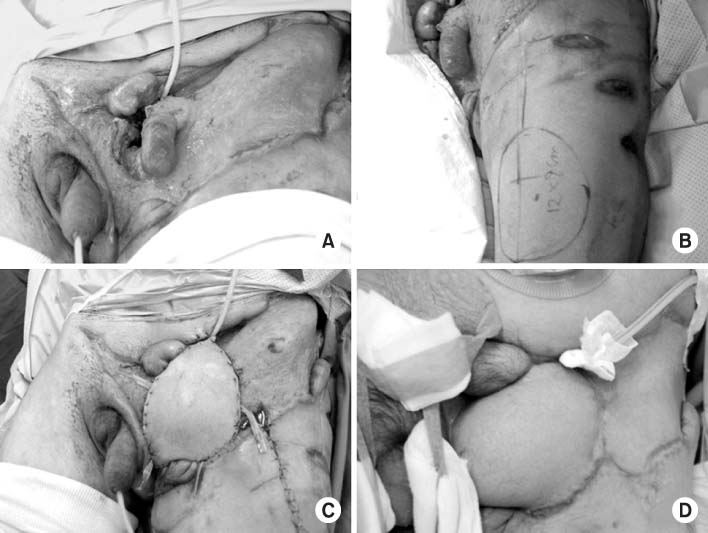
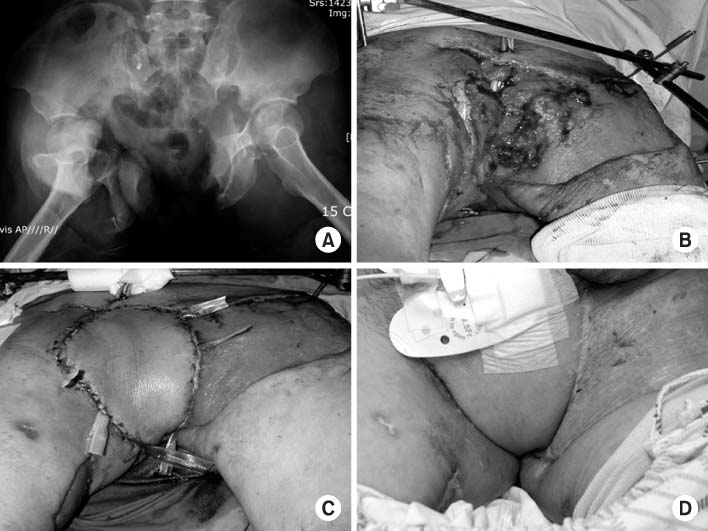
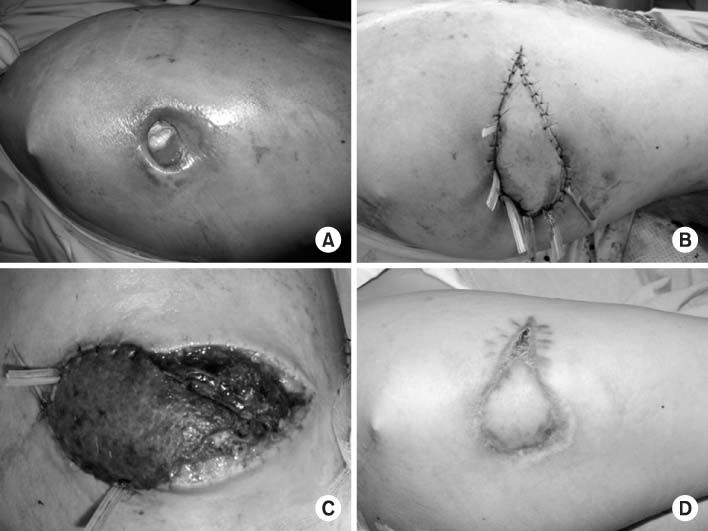
Fig. 1
(A) Preoperative appearance of a 46-year-old man with a soft tissue defect of approximately 25×12 cm with the exposure of left scrotum in the left perineal area.
(B) Design of the flap sized 12×9 cm at ipsilateral anterolateral thigh.
(C) The flap was raised as an island flap connected to the descending branch of the lateral circumflex femoral artery. The flap was transferred to cover the perineal defect.
(D) The flap had an acceptable contour and scar around perineum at 6 months follow-up.
Fig. 2
(A) Radiograph of acetabular and displaced open pelvic fracture (Tile type C2).
(B) Soft tissue defect of a 25×15 cm in the perineal and suprapubic area was noted.
(C) The defect was covered with a 20×15 cm sized anterolateral thigh island flap.
(D) Acceptable contour and infection control around perineum was obtained after 9 months follow-up.
Fig. 3
(A) Pressure sore at the right greater trochanteric area in a paraplegia patient was noted.
(B) The island flap of 8×5 cm was raised from the right thigh and passed through a subcutaneous tunnel to cover the soft tissue defect.
(C) Two days after the operation, the venous congestion was noticed. The decompression of the vascular pedicle was done to resolve the venous insufficiency.
(D) The appearance of the flap 6 months after surgery.
Fig. 1
Fig. 2
Fig. 3
Anterolateral Thigh Island Flap

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

