Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(4); 2020 > Article
- Case Report Axillary Artery Rupture after Shoulder Dislocation That Was Treated with a Self-Expanding Stent - A Case Report -
- HaengJin OHE, Daehyun Hwang, Inkeun Park, Minki Lee, Jun-Ku Lee
-
Journal of Musculoskeletal Trauma 2020;33(4):217-221.
DOI: https://doi.org/10.12671/jkfs.2020.33.4.217
Published online: October 31, 2020
2Departments of Radiology, Inje University Seoul Paik Hospital, Seoul, Korea
3Departments of Orthopedic Surgery, Inje University Seoul Paik Hospital, Seoul, Korea
- 1,256 Views
- 7 Download
- 0 Crossref
- 0 Scopus
Abstract
raumatic shoulder dislocations are one of the most common major dislocations in the general population. Injury to major vessels is rarely reported as a complication of shoulder dislocations. This case report presents the traumatic dissection of the axillary artery after a simple shoulder dislocation that was managed successfully with the placement of a self-expanding stent. With the clinical manifestations of a brachial plexus injury and progressive vascular compromise in the affected arm, a major vascular injury was detected on an angiogram, and a self-expanding stent was deployed. Through immediate diagnosis and prompt intervention, serious complications, such as hypovolemic shock and even death, were averted, ultimately achieving a favorable patient outcome.
Published online Oct 22, 2020.
https://doi.org/10.12671/jkfs.2020.33.4.217
Axillary Artery Rupture after Shoulder Dislocation That Was Treated with a Self-Expanding Stent: A Case Report
 , M.D.,
Daehyun Hwang
, M.D.,
Daehyun Hwang , M.D., Ph.D.,*
Inkeun Park
, M.D., Ph.D.,*
Inkeun Park , M.D.,†
Minki Lee
, M.D.,†
Minki Lee , M.D.,†
and Jun-Ku Lee
, M.D.,†
and Jun-Ku Lee , M.D., Ph.D.†
, M.D., Ph.D.†
Abstract
Traumatic shoulder dislocations are one of the most common major dislocations in the general population. Injury to major vessels is rarely reported as a complication of shoulder dislocations. This case report presents the traumatic dissection of the axillary artery after a simple shoulder dislocation that was managed successfully with the placement of a self-expanding stent. With the clinical manifestations of a brachial plexus injury and progressive vascular compromise in the affected arm, a major vascular injury was detected on an angiogram, and a self-expanding stent was deployed. Through immediate diagnosis and prompt intervention, serious complications, such as hypovolemic shock and even death, were averted, ultimately achieving a favorable patient outcome.
Traumatic shoulder dislocation is one of the most common major dislocations in the general population. Common complications are glenoid labral injury (Bankart lesion), glenoid rim fracture (bony Bankart lesion), fracture of the greater tuberosity of the humeral head, and osteochondral fracture of the posterior humeral head (Hill–Sachs lesion). Indeed, there have been only a few case reports on neurovascular injury of the upper arm and shoulder due to dislocation, and most of the cases resulted from traction injuries in the supraclavicular region of the brachial plexus after manual reduction.1) Some authors have reported the injury of major vessels or nerves around the shoulder joint due to dislocation, but most of the cases were caused by high-energy trauma or recurrent dislocation.1,2) The purpose of this report is to present a case of axillary artery rupture after shoulder dislocation that was successfully treated with the insertion of a self-expanding stent, and thereby avoided the need for open surgical repair.
Case Report
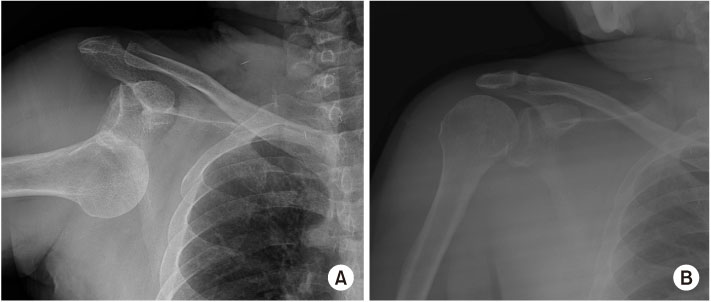
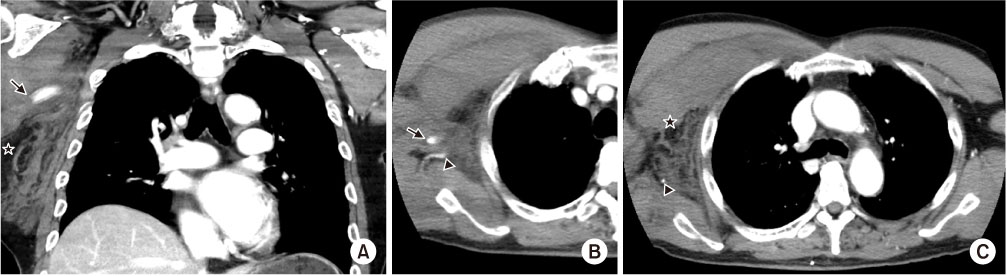
A 74-year-old male patient visited our hospital in a drunken state, complaining of right shoulder pain with limited motion after falling on the ground in a subway station. He had no specific medical history or incidences of shoulder dislocations in the past. The vital signs were stable with a blood pressure (BP) of 100/60 mmHg and heart rate (HR) of 78 beats/min. There was a 2-cm sized, superficial eyebrow laceration. A simple anteroposterior radiograph of the shoulder confirmed the anterior dislocation of the humeral head (Fig. 1A). There was no distal motor or sensory impairment of the forearm and hand on the affected side. The dislocated shoulder was reduced at the first attempt using the traction-counter traction technique under analgesic cover and without sedation. After confirmation of adequate reduction by follow-up radiography, the patient's condition was monitored in the emergency room (Fig. 1B). Within half an hour, the right chest and axilla were found to be swollen, and the patient started complaining of pain, numbness, and weakness of the right arm. Palpation over the brachial artery at the elbow joint revealed a faint pulse, as also in the radial artery at the wrist. The BP was 125/64 mmHg with a HR of 82 beats/min. Computed tomography with contrast enhancement of the chest showed active leakage of contrast media from the third part of the axillary artery and loss of arterial enhancement distally (Fig. 2). His BP decreased to 97/56 mmHg and the HR was 89 beats/min before intervention.
Fig. 1
Plain X-ray image. (A) Anteroposterior radiograph showing anteriorly dislocated shoulder joint. (B) After proper reduction without a deformity.
Fig. 2
Chest computed tomography with contrast enhancement. (A) Discontinuation of the axillary artery (arrow) with hematoma deposition (asterisk). (B) Last axial cut of the visible axillary artery (arrow) with a subscapular branch (arrowhead) in an axial setting. (C) Non-visualization of the axillary artery with only the subscapular artery showing patency (arrowhead) and the prominent right chest wall swelling with hematoma (asterisk) compared to the opposite side.
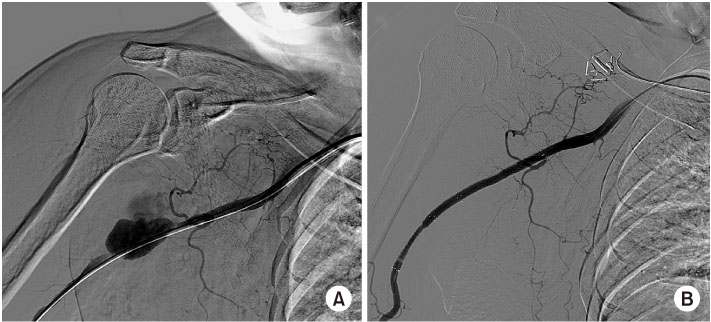
Under local anaesthesia, angiography of the right axillary artery was performed via a femoral artery access, and extravasation of contrast media from the distal third portion of the axillary artery was seen, confirming a rupture & dissection of the main branch of the axillary artery (Fig. 3A). A 0.035-inch Terumo floppy guide wire was positioned across the bleeding site, and we attempted a prolonged balloon inflation (Mustang®, 4 mm×6 mm; Boston Scientific, Marlborough, MA, USA) to control the bleeder. Repeat angiography showed persistent active leakage of contrast media from the lesion. In a second attempt, we deployed a self-expanding stent (Zilver® Flex™, 6 mm×8 mm; Cook Medical, Bloomington, IN, USA) with prolonged postballooning over the lesion. Complete angiography demonstrated no further extravasation of contrast media from the lesion and good patency and flow in the distal arteries (Fig. 3B). After completion of stenting, a strong brachial pulse was palpated as the blood flow was restored through the previously blocked vessel. His upper limb had developed a motor weakness of grade II (shoulder abduction, elbow flexion, and wrist dorsiflexion) and grade III (elbow extension and finger flexion). The post procedural period was uneventful and he was discharged on post procedural day 9. His shoulder dislocation was managed with the Velpeau arm sling immobilizer for a month, following which active range of shoulder motion was allowed. During assessments at the out-patient department, we found an improvement of the neuropathy, and the patient regained normal function at 3 months, with full range of shoulder motion and complete recovery of the distal motor and sensory functional impairment. Overall, after one year of follow up, the patient did not complain of any further dislocations or symptoms related to the affected shoulder.
Fig. 3
(A) Right upper limb angiogram demonstrates leakage of dye in the distal third portion of the axillary artery. (B) Revascularization after intraluminal stenting demonstrates patent distal flow without further leakage.
Discussion
We present a case of axillary artery injury with upper arm neuropraxia after shoulder dislocation caused by a simple fall at ground level in a 74-year-old male patient.
In the rare instances of major vessel or nerve injury due to dislocation, the axillary artery is most commonly damaged during anterior dislocation of the shoulder, and more than 90% of the reported injuries involve its third portion, beyond the lower edge of the pectoralis minor.1,2,3) Additionally, because of loss of arterial elasticity, older patients are more prone to sustain vascular injury. Likewise, more than 90% of vascular injury following shoulder dislocation involve patients older than 50 years.4)
There are three possible mechanisms of injury by anterior dislocation of the humeral head. The first mechanism involves the sudden kinking of the brachial artery between the lower edge of the pectoralis major and the upper edge of the teres major muscles. Gibson5) suggested that when the shoulder is anteriorly dislocated, the hyper-abducted humeral head exposes the arteries of the upper arm and bends it against the fulcrum of the edge of the muscles, leading to vascular injury. Secondly, in patients with history of shoulder dislocation, the initial injury may cause inflammation of the tissues around the artery, which can make it rather stiff and vulnerable to tensile forces.6) Lastly, direct or transmitted pressure by the dislocated humeral head on a non-elastic atherosclerotic artery in the elderly can also be a possible cause of arterial rupture.2) In the literature, most of the cases were caused by high-energy trauma or recurrent dislocation.1,2) However, our patient presented with axillary artery rupture after shoulder dislocation from a ground-level fall with concomitant eyebrow laceration.
Acute upper arm ischaemia after dislocation should be treated with urgent anatomical reduction with thorough examination of the neurovascular structures. It is widely known as a pathognomonic triad, wherein the presence of an axillary mass, anterior shoulder dislocation, and the absence of a distal pulse are evidences of acute arterial rupture. Early diagnosis is crucial since a delay can lead to fatal consequences.3,4)
Traditionally, open surgical repair of the axillary artery is performed through sternotomy or thoracotomy exposure.7) These procedures are time-consuming and pose a risk of collateral injury to the surrounding neurovascular structures. Endovascular repair including stent insertion has the advantages of lowering the need for general anaesthesia and preserving the neurovascular structures around the damaged blood vessels. However, endovascular interventions in the peripheral circulation have proven problematic as endovascular stenting is generally effective only in the relatively larger inflow arteries with focal lesions.7,8) Additionally, the long-term durability of stents have not been established and the procedure is mainly indicated in patients with decreased life expectancy.7) In small sized arteries, there are concerns for thrombosis triggered by the metallic stent and technical difficulties.8,9) Furthermore, there are possibilities that when a stent is deployed near a joint, it may break or move in the future, due to its exaggerated bending and twisting with skeletal movements.8) The axillary artery, in particular, has several branches emerging from it and endovascular stenting may impede these collaterals. Nevertheless, Xenos et al.7) compared covered stent insertion and surgical restoration for the subclavian and axillary arteries, and those arteries damaged by blunt or penetrating injuries. In 23 patients (16 who underwent open repair and 7 who underwent amendable endovascular repair), the short-term follow-up results were similar, but stent insertion had the advantage of shorter procedural times and lesser blood loss. Only one patient presented with arterial occlusion 9 months after the stent placement.
In our case, through immediate diagnosis and prompt interventional management, we averted serious complications, such as hypovolemic shock or even death and lasting neurological deficits, ultimately achieving a favourable outcome without occlusion in the one year of follow up.
Furthermore, brachial plexus injuries occur commonly with axillary arterial injuries, ranging from 27% to 60%, and are often due to the close proximity to the artery, which can cause long-term disability to the patients.3) Recent studies suggest that if patients show neurovascular compromise, early exploration to establish the extent of lesion can increase the chances of axonal regrowth and re-innervation of the distal musculature.10) In this case, serial neurologic examinations were conducted regularly and the brachial plexus palsy completely recovered after 3 months without further management.
In conclusion, axillary artery rupture due to shoulder dislocation can occur in the elderly population. Given the emergent circumstances that surround an arterial rupture and the complications associated with surgical repair, endovascular stenting can be an innovative rescue therapy if it is properly applied.
Financial support:None.
Conflict of interests:None.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

