Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 30(1); 2017 > Article
-
Review Article
- Treatment Strategy of Infected Nonunion
- Hyoung-Keun Oh, M.D.
-
Journal of the Korean Fracture Society 2017;30(1):52-62.
DOI: https://doi.org/10.12671/jkfs.2017.30.1.52
Published online: January 20, 2017
Department of Orthopaedic Surgery, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea.
- Correspondence to: Hyoung-Keun Oh, M.D. Department of Orthopaedic Surgery, Inje University Ilsan Paik Hospital, 170 Juhwa-ro, Ilsanseo-gu, Goyang 10380, Korea. Tel: +82-31-910-7968, Fax: +82-31-910-7967, osd11@paik.ac.kr
Copyright © 2017 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,032 Views
- 16 Download
- 2 Crossref
Abstract
- The management of infected nonunion is based on a detailed evaluation of patients, the involved bone and soft tissues, stability of fixation, and type of bacterial pathogens. Preoperative surgical planning and strategies for each step is mandatory for the successful treatment of infected nonunion. The radical debridement of infected tissues, including the unstable implant, is one of the most important procedures. Adequate soft tissue coverage should be considered for the appropriate management of infection; a reconstructive procedure and stable skeletal stabilization by internal or external fixation is also necessary later. A restoration of bone defects and bony union can be accomplished with bone grafting, distraction osteogenesis, vascularized fibular grafting, and induced membrane technique.
- 1. Jain AK, Sinha S. Infected nonunion of the long bones. Clin Orthop Relat Res, 2005;(431):57-65.Article
- 2. Motsitsi NS. Management of infected nonunion of long bones: the last decade (1996-2006). Injury, 2008;39:155-160.Article
- 3. Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res, 1989;(243):36-40.Article
- 4. Ha SH. Treatment of Infected Nonunion. J Korean Fract Soc, 2007;20:206-214.Article
- 5. Schmidt AH, Swiontkowski MF. Pathophysiology of infections after internal fixation of fractures. J Am Acad Orthop Surg, 2000;8:285-291.Article
- 6. Kim JH, Yoon YC, Kim YW, Jung SH, Oh JK. Diagnosis and management of posttraumatic chronic osteomyelitis. J Korean Fract Soc, 2014;27:88-104.Article
- 7. Perry CR, Pearson RL, Miller GA. Accuracy of cultures of material from swabbing of the superficial aspect of the wound and needle biopsy in the preoperative assessment of osteomyelitis. J Bone Joint Surg Am, 1991;73:745-749.Article
- 8. Bose D, Kugan R, Stubbs D, McNally M. Management of infected nonunion of the long bones by a multidisciplinary team. Bone Joint J, 2015;97:814-817.ArticlePDF
- 9. Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg, 2005;13:417-427.Article
- 10. Maini L, Chadha M, Vishwanath J, Kapoor S, Mehtani A, Dhaon BK. The Ilizarov method in infected nonunion of fractures. Injury, 2000;31:509-517.Article
- 11. Kim HM, Park IJ, Kim YS, et al. Free vascularized fibular grafts for treatment of infected nonunion of the tibia. J Korean Fract Soc, 2006;19:163-169.Article
- 12. Ko HS, Kang YH, Kim DW, Ha JK. The treatment of infected non-union of long bones with plate and screws. J Korean Fract Soc, 2006;19:72-77.Article
- 13. Sadek AF, Laklok MA, Fouly EH, Elshafie M. Two stage reconstruction versus bone transport in management of resistant infected tibial diaphyseal nonunion with a gap. Arch Orthop Trauma Surg, 2016;136:1233-1241.ArticlePDF
- 14. Prasarn ML, Ahn J, Achor T, Matuszewski P, Lorich DG, Helfet DL. Management of infected femoral nonunions with a single-staged protocol utilizing internal fixation. Injury, 2009;40:1220-1225.Article
- 15. Han SK, Choi NY, Park SJ, Lee SK, Jang G, Lee IJ. Antibiotic cement-coated unreamed nailing for treatment of infected nonunion of long bone. J Korean Orthop Assoc, 2000;35:699-703.ArticlePDF
- 16. Holtom PD, Patzakis MJ. Newer methods of antimicrobial delivery for bone and joint infections. Instr Course Lect, 2003;52:745-749.
- 17. McKee MD, Wild LM, Schemitsch EH, Waddell JP. The use of an antibiotic-impregnated, osteoconductive, bioabsorbable bone substitute in the treatment of infected long bone defects: early results of a prospective trial. J Orthop Trauma, 2002;16:622-627.Article
- 18. Swiontkowski MF, Hanel DP, Vedder NB, Schwappach JR. A comparison of short- and long-term intravenous antibiotic therapy in the postoperative management of adult osteomyelitis. J Bone Joint Surg Br, 1999;81:1046-1050.ArticlePDF
- 19. Virani SR, Dahapute AA, Bava SS, Muni SR. Impact of negative pressure wound therapy on open diaphyseal tibial fractures: A prospective randomized trial. J Clin Orthop Trauma, 2016;7:256-259.Article
- 20. Chen CE, Ko JY, Pan CC. Results of vancomycin-impregnated cancellous bone grafting for infected tibial nonunion. Arch Orthop Trauma Surg, 2005;125:369-375.ArticlePDF
- 21. Stafford PR, Norris BL. Reamer-irrigator-aspirator bone graft and bi Masquelet technique for segmental bone defect nonunions: a review of 25 cases. Injury, 2010;41:Suppl 2. S72-S77.Article
- 22. Yin P, Zhang L, Li T, et al. Infected nonunion of tibia and femur treated by bone transport. J Orthop Surg Res, 2015;10:49. ArticlePDF
- 23. Oh CW, Song HR, Roh JY, et al. Bone transport over an intramedullary nail for reconstruction of long bone defects in tibia. Arch Orthop Trauma Surg, 2008;128:801-808.ArticlePDF
- 24. Oh CW, Apivatthakakul T, Oh JK, et al. Bone transport with an external fixator and a locking plate for segmental tibial defects. Bone Joint J, 2013;95:1667-1672.ArticlePDF
- 25. Fischer C, Doll J, Tanner M, et al. Quantification of TGF-β1, PDGF and IGF-1 cytokine expression after fracture treatment vs. non-union therapy via masquelet. Injury, 2016;47:342-349.Article
- 26. Mauffrey C, Hake ME, Chadayammuri V, Masquelet AC. Reconstruction of long bone infections using the induced membrane technique: tips and tricks. J Orthop Trauma, 2016;30:e188-e193.Article
- 27. Cho JW, Kim J, Kim HJ, Oh JK. Management of long bone fractures with severe bone defect. J Korean Fract Soc, 2015;28:205-214.Article
REFERENCES
Fig. 1

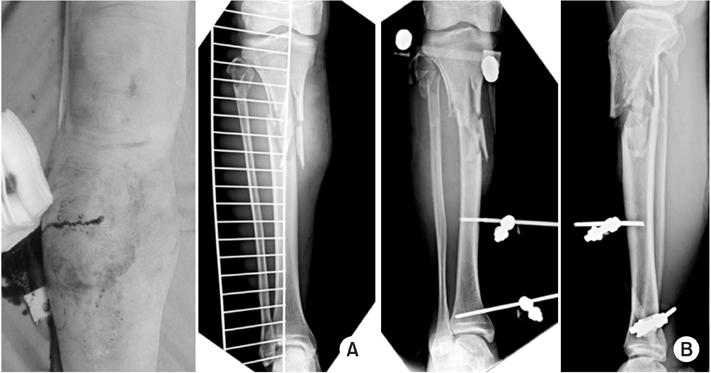
A 33-year-old male suffered from open femoral shaft fracture associated with complete femoral artery (arrow).

Fig. 2
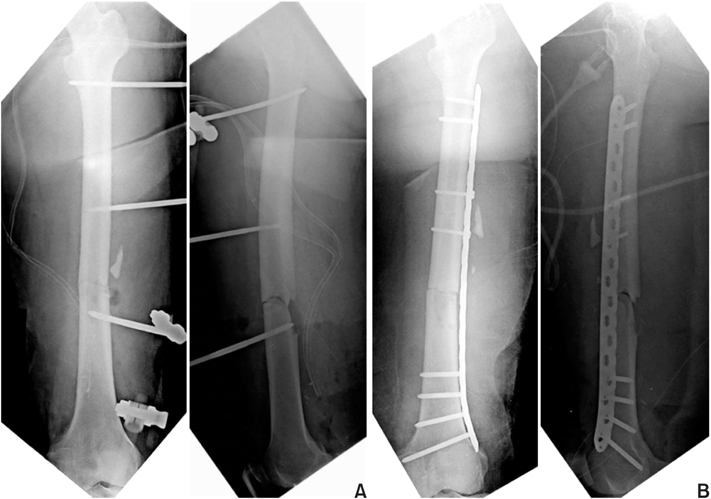
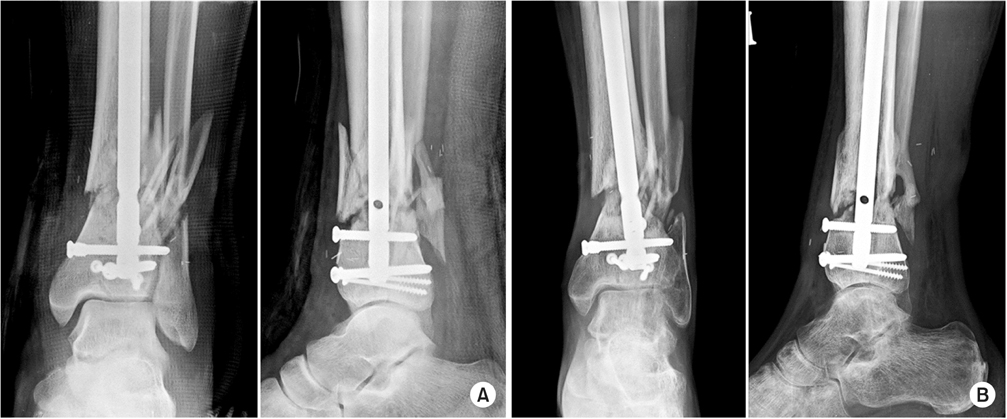
(A) A temporary external fixation was carried out after wound debridement and vascular reconstruction. (B) External fixation was converted to bridging-plate fixation after soft tissue healing.
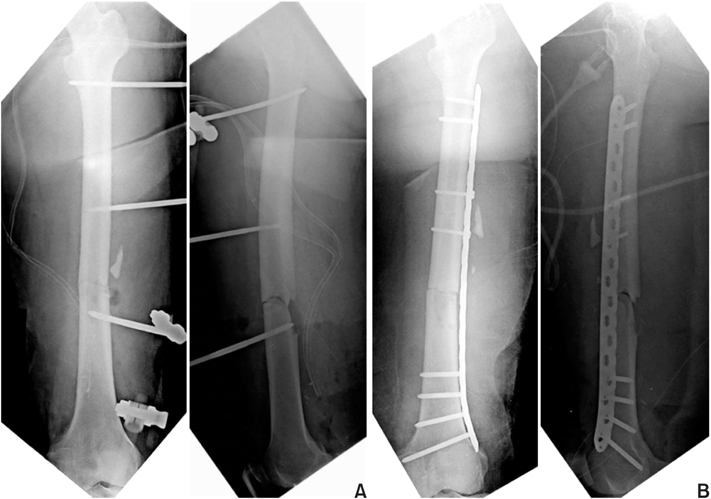
Fig. 3
(A) Plain X-ray taken 6 months after the injury shows delayed healing of the fracture without implant loosening. Tissue biopsy from the nonunion site revealed an infection, but there was no significant instability of the fracture, and infection was localized around the fracture site. After meticulous debridement of the infected tissue, autogenous cancellous bone graft and plate augmentation was performed. (B) Plain X-ray taken 12 months after revision surgery shows a solid bony union without recurrence of infection.
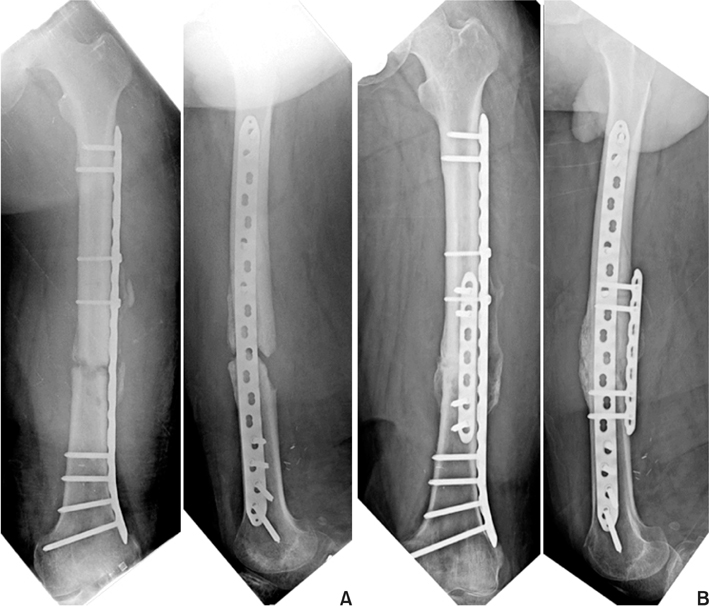
Fig. 4

Open type IIIc distal tibia and fibular fracture of a 31-year-old male was treated with vascular reconstruction and temporary external fixation.

Fig. 5
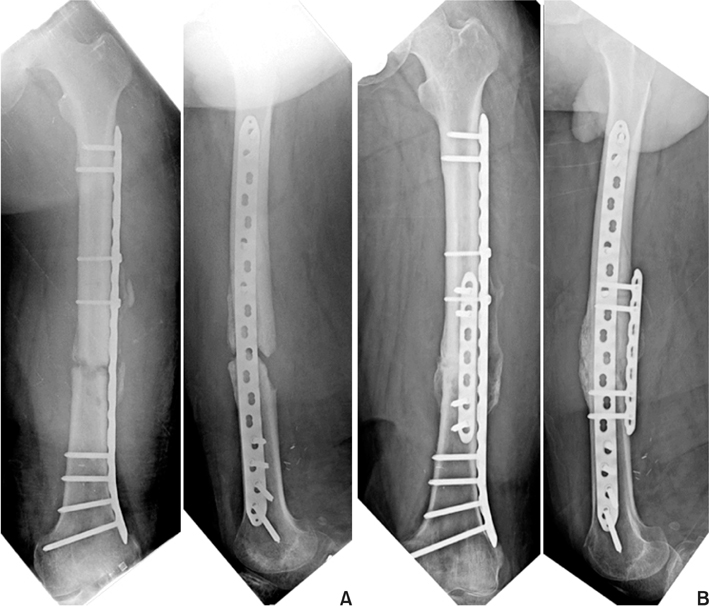
(A) Internal fixation with intramedullary nail was carried out after soft tissue healing. (B) Plain X-ray taken 7 months after the injury shows atrophic nonunion, and there was pus discharge from the previously open wound on the medial side.
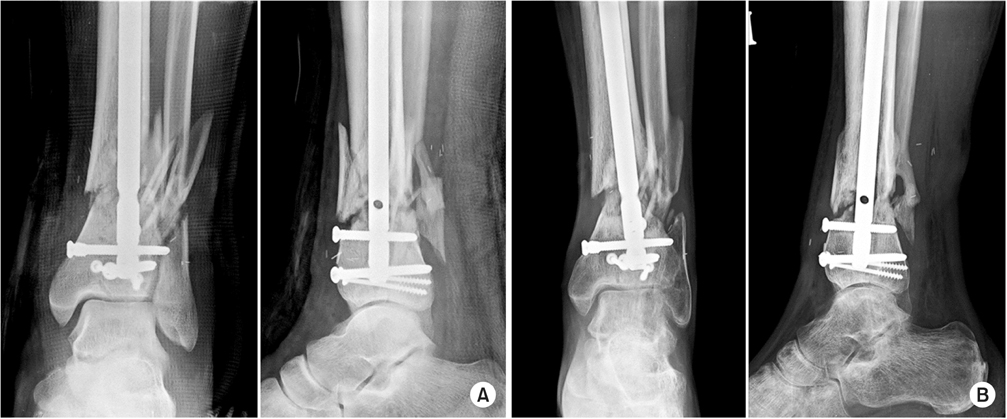
Fig. 6
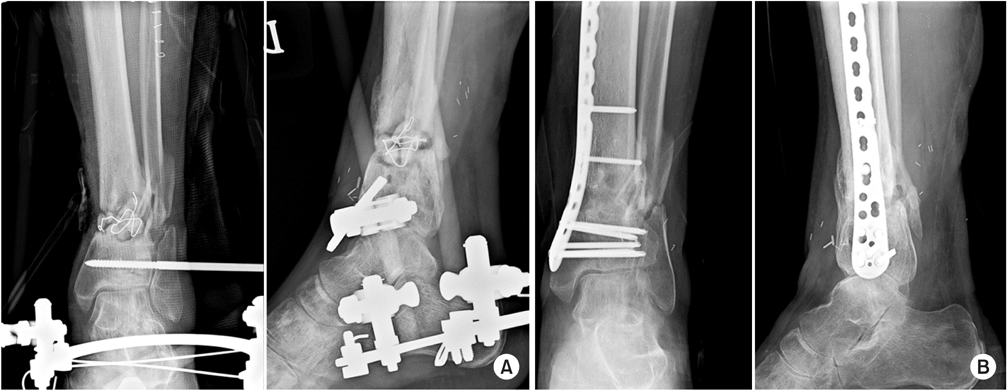
(A) Under the diagnosis of infected nonunion, radical debridement of the infected tissue was performed and the fracture was stabilized by an external fixator. The bone defect after debridement was filled by an anti-cement bead. (B) An X-ray from the final follow-up showed a solid bony union after autogenous bone graft and plate fixation.
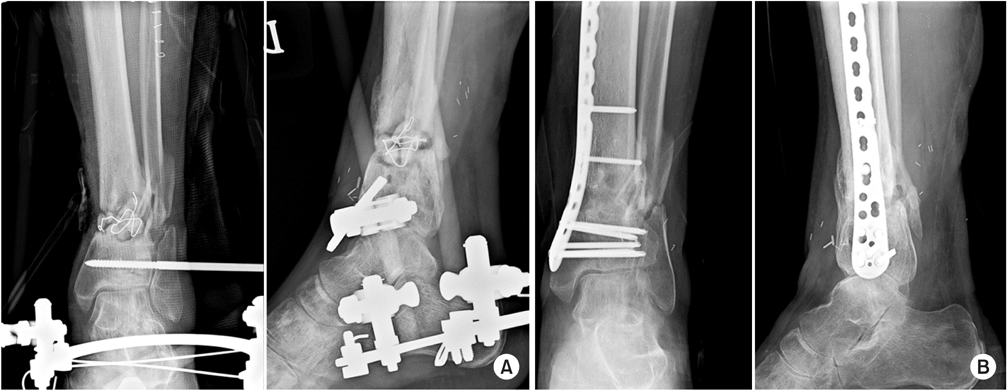
Fig. 7
(A) Clinical photography and X-ray show open comminuted proximal tibia fracture of a 72-year-old male. (B) Due to associated multiple injury, the fracture was stabilized by a temporary external fixator.
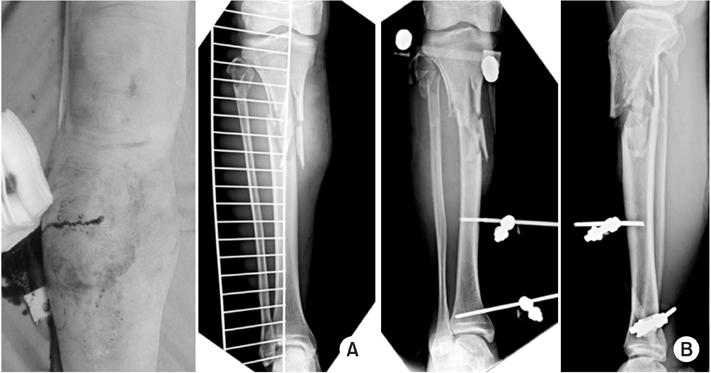
Fig. 8

(A) An X-rays and clinical photography taken 5 months after the injury showed infected nonunion after definite plate fixation with soft tissue defect. (B) The radical debridement of infected bone and soft tissue was carried out. The bone defect was filled by an anti-cement spacer (induced membrane technique) and soft tissue defect was covered by a free flap.

Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Systematic Diagnosis and Treatment Principles for Acute Fracture-Related Infections
Jeong-Seok Choi, Jun-Hyeok Kwon, Seong-Hyun Kang, Yun-Ki Ryu, Won-Seok Choi, Jong-Keon Oh, Jae-Woo Cho
Journal of the Korean Fracture Society.2023; 36(4): 148. CrossRef - The Antibiotic Cement Coated Nail and Masquelet Technique for the Treatment of Infected Nonunion of Tibia with Bone Defect and Varus Deformity: A Case Report
Min Gu Jang, Jae Hwang Song, Dae Yeung Kim, Woo Jin Shin
Journal of the Korean Fracture Society.2022; 35(1): 26. CrossRef
Treatment Strategy of Infected Nonunion

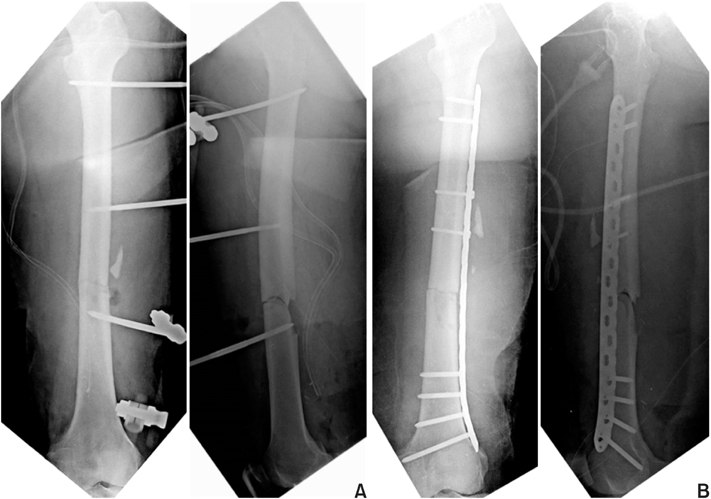
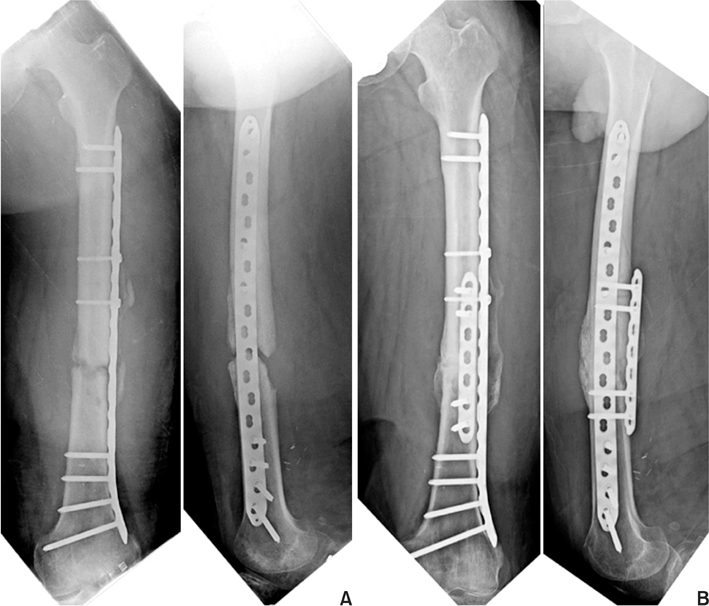

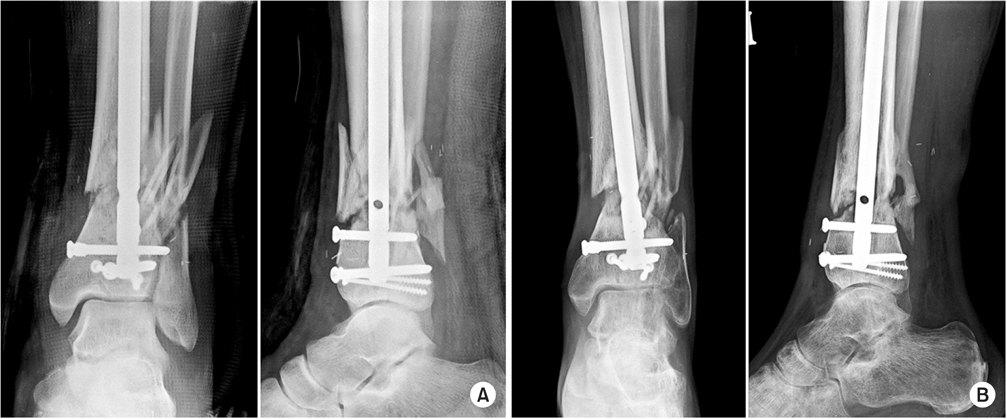
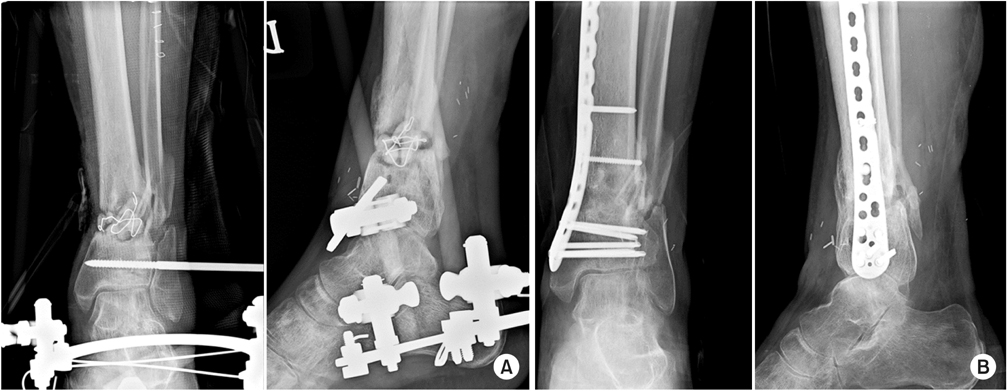
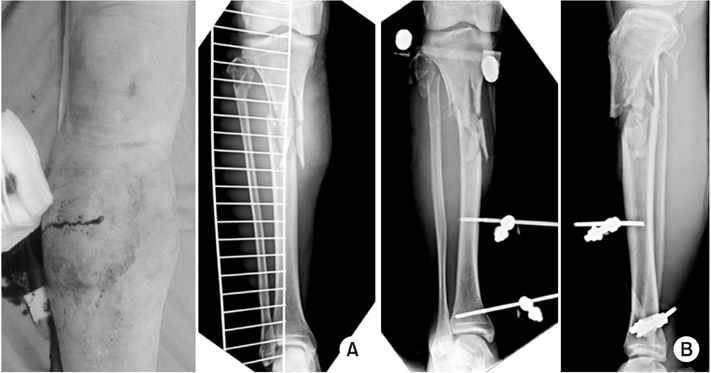


Fig. 1
A 33-year-old male suffered from open femoral shaft fracture associated with complete femoral artery (arrow).
Fig. 2
(A) A temporary external fixation was carried out after wound debridement and vascular reconstruction. (B) External fixation was converted to bridging-plate fixation after soft tissue healing.
Fig. 3
(A) Plain X-ray taken 6 months after the injury shows delayed healing of the fracture without implant loosening. Tissue biopsy from the nonunion site revealed an infection, but there was no significant instability of the fracture, and infection was localized around the fracture site. After meticulous debridement of the infected tissue, autogenous cancellous bone graft and plate augmentation was performed. (B) Plain X-ray taken 12 months after revision surgery shows a solid bony union without recurrence of infection.
Fig. 4
Open type IIIc distal tibia and fibular fracture of a 31-year-old male was treated with vascular reconstruction and temporary external fixation.
Fig. 5
(A) Internal fixation with intramedullary nail was carried out after soft tissue healing. (B) Plain X-ray taken 7 months after the injury shows atrophic nonunion, and there was pus discharge from the previously open wound on the medial side.
Fig. 6
(A) Under the diagnosis of infected nonunion, radical debridement of the infected tissue was performed and the fracture was stabilized by an external fixator. The bone defect after debridement was filled by an anti-cement bead. (B) An X-ray from the final follow-up showed a solid bony union after autogenous bone graft and plate fixation.
Fig. 7
(A) Clinical photography and X-ray show open comminuted proximal tibia fracture of a 72-year-old male. (B) Due to associated multiple injury, the fracture was stabilized by a temporary external fixator.
Fig. 8
(A) An X-rays and clinical photography taken 5 months after the injury showed infected nonunion after definite plate fixation with soft tissue defect. (B) The radical debridement of infected bone and soft tissue was carried out. The bone defect was filled by an anti-cement spacer (induced membrane technique) and soft tissue defect was covered by a free flap.
Fig. 9
An X-ray from the last follow-up showed solid bony union after autogenous bone graft and plate fixation after infection control.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
Fig. 9
Treatment Strategy of Infected Nonunion

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

