Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 30(1); 2017 > Article
-
Original Article
- Treatment of Wide Gap Non-Unions in Lower Extremities
- Doohoon Sun, M.D., Ph.D., Byeong-Seop Park, M.D., Taehyeon Jeon, M.D., Seung-Koo Rhee, M.D., Ph.D.
-
Journal of the Korean Fracture Society 2017;30(1):1-8.
DOI: https://doi.org/10.12671/jkfs.2017.30.1.1
Published online: January 20, 2017
Department of Orthopaedic Surgery, Daejeon Sun Hospital, Daejeon, Korea.
- Correspondence to: Seung-Koo Rhee, M.D., Ph.D. Department of Orthopaedic Surgery, Daejeon Sun Hospital, 29 Mokjung-ro, Jung-gu, Daejeon 34811, Korea. Tel: +82-42-220-8860, Fax: +82-42-220-8864, Skrhee@catholic.ac.kr
• Received: October 16, 2016 • Revised: December 12, 2016 • Accepted: December 30, 2016
Copyright © 2017 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 399 Views
- 5 Download
Abstract
-
Purpose
- To analyze the end results of the treatment for patients with wide gap non-unions of the long bones in the lower extremities.
-
Materials and Methods
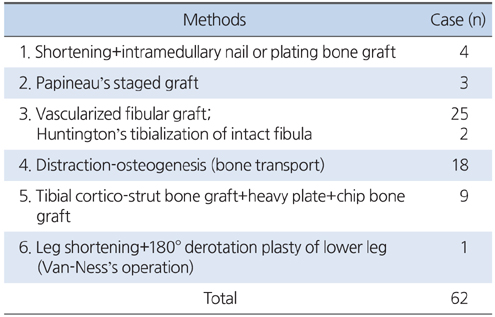
- A total of 62 cases of wide gap unions, with a mean age of 38 years, were included for analysis. Study cohort included six children under the age of seven years. The average size of established bone defect was 7 cm (4-23 cm). Bone defects under 7 cm were treated with plating and various bone grafts, and those over 7 cm were managed with vascularized fibular graft (VFG), distraction-osteogenesis, tibial strut, plating and etc. Two boys with a defect of the whole tibia but with an intact fibula were treated with tibialization of intact fibula and with rotation-plasty of the leg. Their end results were evaluated by the time of bony union in accordance with the treatment of defect size of the long bone as well as their age.
-
Results
- Bony unions were obtained for an average period of at least 27 months. Fifty-one cases showed an average leg-length discrepancy of 2.8 cm, and 11 cases showed no leg-length discrepancy. The VFG, distraction-osteogenesis, and tibial cortical-strut graft and plating were the most effective methods for non-unions of wide, long bone defections (>7 cm). The prognosis was more favorable in children, muscular femur, and in cases with tibial defect but intact fí bula.
-
Conclusion
- Various bone union techniques should be considered carefully, considering the ages of patients and the size of bone defects. Due to severe physical and mental disabilities of patients during the long-treatment period, specialized orthopedic doctors for trauma and mental care were necessary.
- 1. Crist BD, Ferguson T, Murtha YM, Lee MA. Surgical timing of treating injured extremities: an evolving concept of urgency. Instr Course Lect, 2013;62:17-28.
- 2. Finkemeier CG, Schmidt AH, Kyle RF, Templeman DC, Varecka TF. A prospective, randomized study of intramedullary nails inserted with and without reaming for the treatment of open and closed fractures of the tibial shaft. J Orthop Trauma, 2000;14:187-193.
- 3. Wang HT, Erdmann D, Fletcher JW, Levin LS. Anterolateral thigh flap technique in hand and upper extremity reconstruction. Tech Hand Up Extrem Surg, 2004;8:257-261.
- 4. Duan X, Al-Qwbani M, Zeng Y, Zhang W, Xiang Z. Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database Syst Rev, 2012;1:CD008241.
- 5. Young S, Lie SA, Hallan G, Zirkle LG, Engesæter LB, Havelin LI. Risk factors for infection after 46,113 intramedullary nail operations in low- and middle-income countries. World J Surg, 2013;37:349-355.
- 6. Papineau LJ. Excision-graft with deliberately delayed closing in chronic osteomyelitis. Nouv Presse Med, 1973;2:2753-2755.
- 7. Papineau LJ, Alfageme A, Dalcourt JP, Pilon L. Chronic osteomyelitis: open excision and grafting after saucerization (author's transl). Int Orthop, 1979;3:165-176.
- 8. Huntington TW. VI. Case of bone transference: use of a segment of fibula to supply a defect in the tibia. Ann Surg, 1905;41:249-251.
- 9. Van-Ness CP. Rotation-plasty for congenital defects of the femur. Making use of the ankle of the shortened limb to control the knee joint of the prosthesis. J Bone Joint Surg Br, 1950;31:12-16.
- 10. Ilizarov GA, Deviatov AA, Trokhova VG. Surgical lengthening of the shortened lower extremities. Vestn Khir Im I I Grek, 1972;108:100-103.
- 11. Ring D, Jupiter JB, Gan BS, Israeli R, Yaremchuk MJ. Infected nonunion of the tibia. Clin Orthop Relat Res, 1999;(369):302-311.
- 12. Shahid M, Hussain A, Bridgeman P, Bose D. Clinical outcomes of the Ilizarov method after an infected tibial non union. Arch Trauma Res, 2013;2:71-75.
- 13. Taylor GI, Miller GD, Ham FJ. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg, 1975;55:533-544.
- 14. El-Gammal TA, El-Sayed A, Kotb MM. Hypertrophy after free vascularized fibular transfer to the lower limb. Microsurgery, 2002;22:367-370.
- 15. Ikeda K, Tomita K, Hashimoto F, Morikawa S. Long-term follow-up of vascularized bone grafts for the reconstruction of tibial nonunion: evaluation with computed tomographic scanning. J Trauma, 1992;32:693-697.
- 16. Hsu RW, Wood MB, Sim FH, Chao EY. Free vascularised fibular grafting for reconstruction after tumour resection. J Bone Joint Surg Br, 1997;79:36-42.
- 17. Lazar E, Rosenthal DI, Jupiter J. Free vascularized fibular grafts: radiographic evidence of remodeling and hypertrophy. AJR Am J Roentgenol, 1993;161:613-615.
- 18. Wada T, Usui M, Nagoya S, Isu K, Yamawaki S, Ishii S. Resection arthrodesis of the knee with a vascularised fibular graft. Medium- to long-term results. J Bone Joint Surg Br, 2000;82:489-493.
- 19. de Boer HH, Wood MB. Bone changes in the vascularised fibular graft. J Bone Joint Surg Br, 1989;71:374-378.
- 20. Bos KE, Besselaar PP, vd Eijken LW, Raaymakers EL. Failure of hypertrophy in revascularised fibula grafts due to stress protection. Microsurgery, 1996;17:366-370.
- 21. Chew WY, Low CK, Tan SK. Long-term results of free vascularized fibular graft. A clinical and radiographic evaluation. Clin Orthop Relat Res, 1995;(311):258-261.
- 22. Hahn E. Eine methode, pseudarthrosen der tibia mit grossen knockendefekt zur heilung zu bringen. Zentralbl f Chir, 1884;11:337-341.
- 23. Kim SS, Cha HS. Rotation-plasty for the treatment of the malignant bone tumor - 2 cases reports. J Korean Orthop Assoc, 1983;18:794-798.
- 24. Kim JM, Rhee SK, Kim Y, Shin JH. A rotaion-plasty for focal femoral deficiency due to chronic osteomyelitis. J Korean Orthop Assoc, 1989;24:84-88.
REFERENCES
Fig. 1
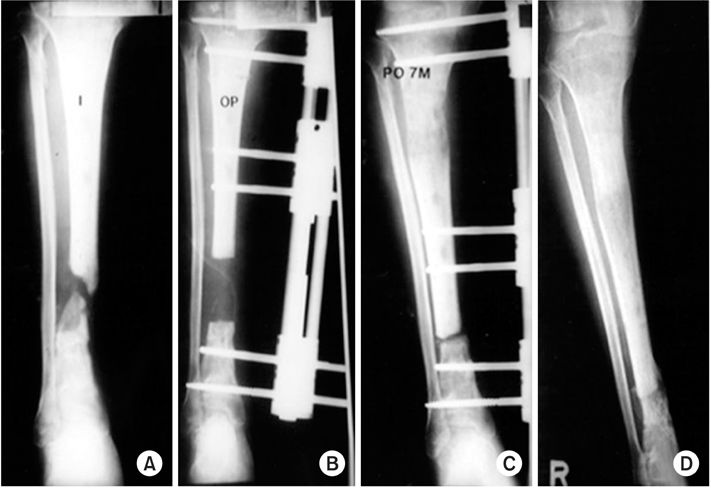
A 46-year-old male. (A) An open segmental 6 cm defect of tibiawas treated with two trials of sauscerization. Finally, an 8 cm defect was noted (B) and distraction osteogenesis for 4 months was performed (C). During the process, no skin problems on pin tracts, and pain was tolerable. (D) Nine months after the trauma, bony union was successful, knee motions were normal, with limited ankle motions, 0° dorsiflexion and 20° palmar flexion only.
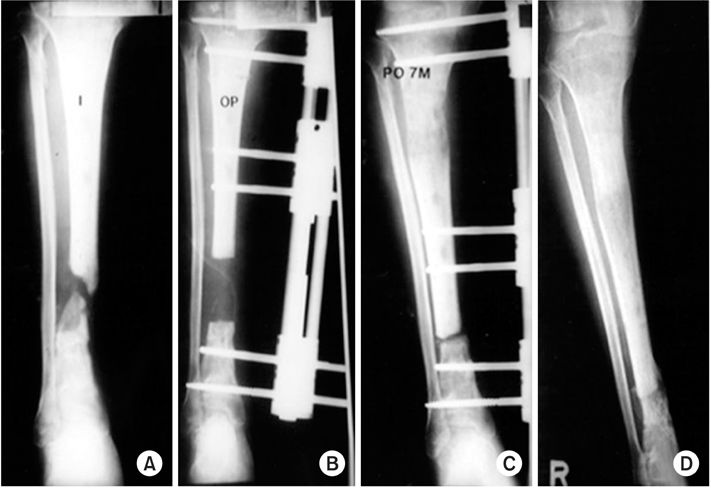
Fig. 2
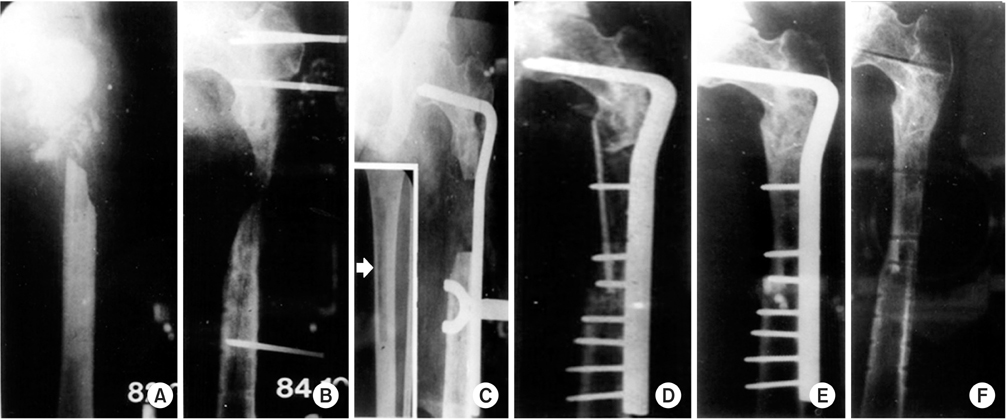
A 19-year-old female. A severe compound fracture on the proximal femur from a gun shot injury (A); sauscerization was performed 6 times and split skin grafts was done 2 times (B). (C) After cessation of chronic osteomyelitis, a tibial cortico-strut and cancellous chip bone grafts (arrow) with heavy duty condylar plate fixation was performed. Four-and-half years later, a solid bony union was obtained (D, E), but a shortening of the limb by 2 cm was noted (F).
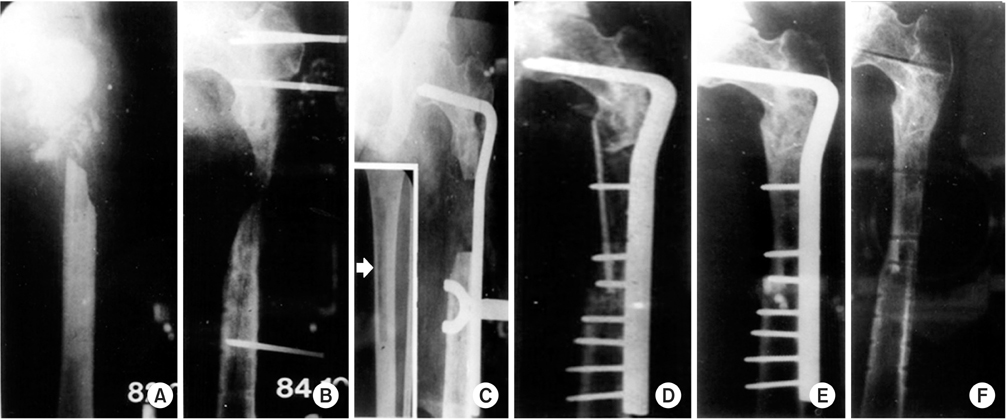
Fig. 3
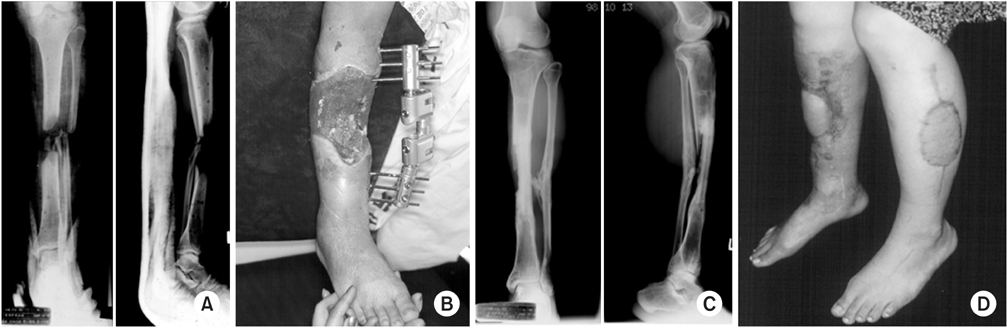
A 34-year-old male. A 6 cm of tibial (A) and wide skin defects (B) was treated by a 12 cm osteo-cutaneous vascularized fibular graft after 8 weeks of trauma; 7 months later, the grafted fibula was united well and hypertrophied (C), and partial weight bearing was possible (D).
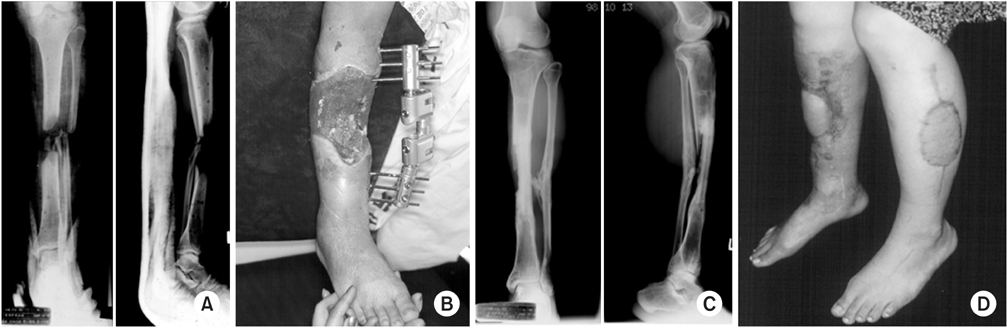
Fig. 4

An 8-year-old boy. A staged medial transport (tibialization) of intact fibula with a 6-week interval (B, C) for the whole defected tibial shaft but intact fibula (A) was observed after performing a wide-split thickness skin graft two times, 3 months after a traffic accident. (D) Six months after the operations, the grafted fibular was united and hypertrophied well, but limping, serious edema by venous stasis on leg was noted. The knee and ankle joint motions were very limitted—nearly stiff—but walking was also possible with a cane. However, the patient and parents were happy for saving the leg.

Fig. 5

A 52-year-old male. An open comminuted fracture on proximal tibia (A) was treated with sauscerization, rotational skin flap, and the 12 cm vascularized fibular graft for 5 cm of bone defect two months after a traffic accident (B). The fracture was occurred because it was too weak to bear any weight, and so a condylar plate with cancellous chip bone graft was performed 4 months after the trauma (C), and the knee range of motion was 10° to 60°.

Fig. 6
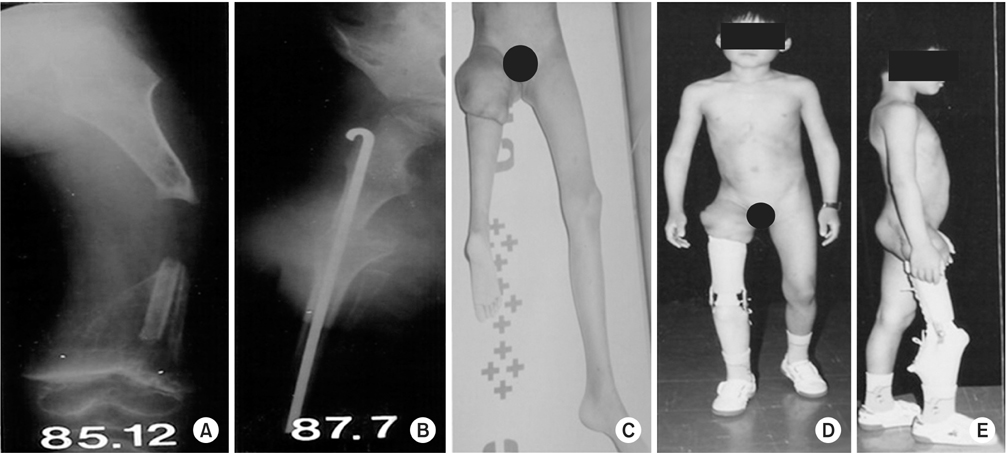
(A) A 7-year-old boy had suffered from an uncontrollable osteomyelitis of the femur, with a 14 cm wide segmental defect, despite 6 attempts of sauscerization and 2 attempts of vascularized fibular graft. Initially, an above-the-knee amputaion was seriously considered. However, we performed the Van-Ness's operation associated with a sacrifice of the knee joint, including the infected distal femur and the proximal tibia, and performrd a 180° rotation-plasty of the leg (B, C) to aquire the knee function with ankle. (D, E) He was well tolerated with the rotated foot, which was good to control the brace as a below–knee stump, and the heel functioned as a patella to support the body weight. Nonetheless, psychosocial attention will be required later. We revieved an agreement by patient to carry photoes exposed the face in this paper.
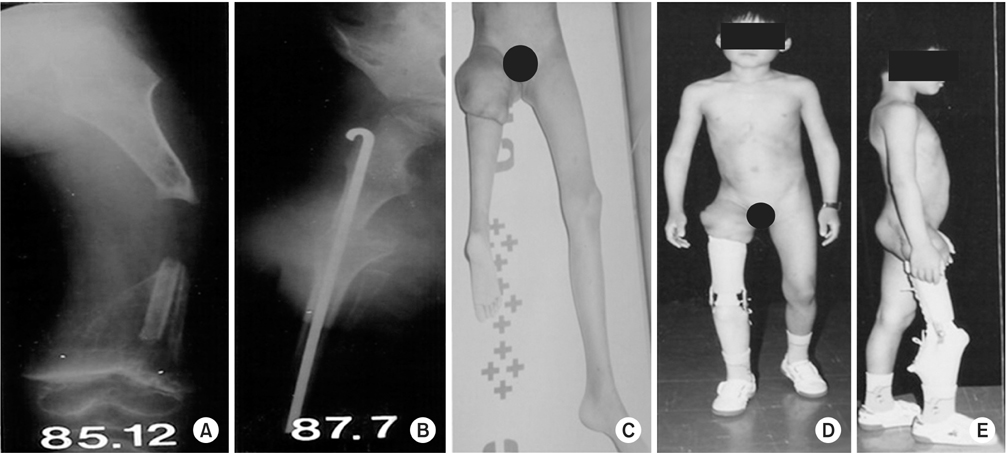
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

Treatment of Wide Gap Non-Unions in Lower Extremities

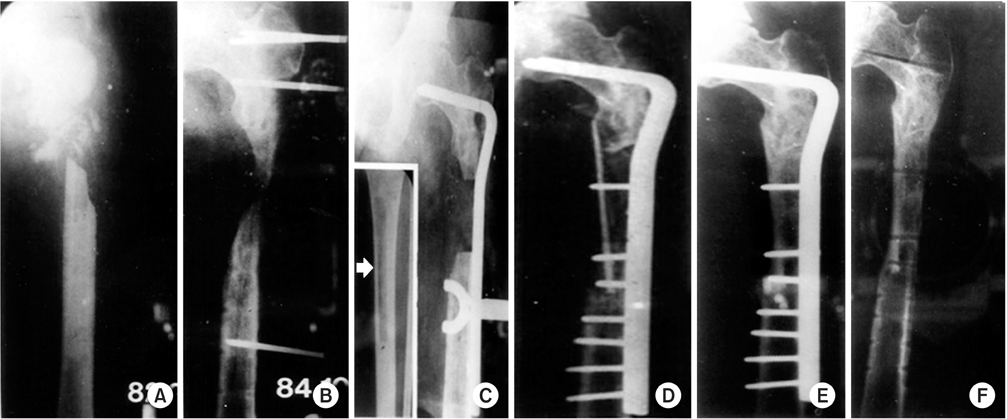
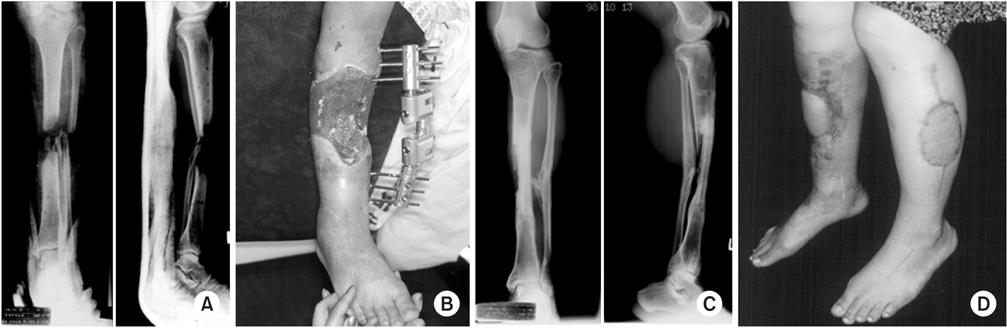

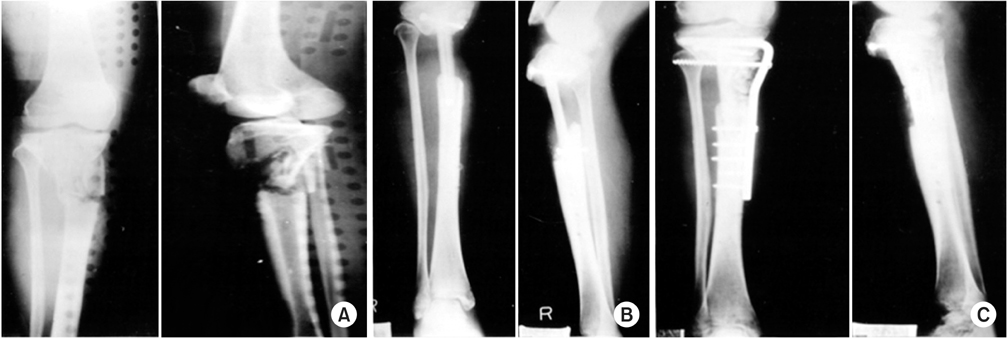
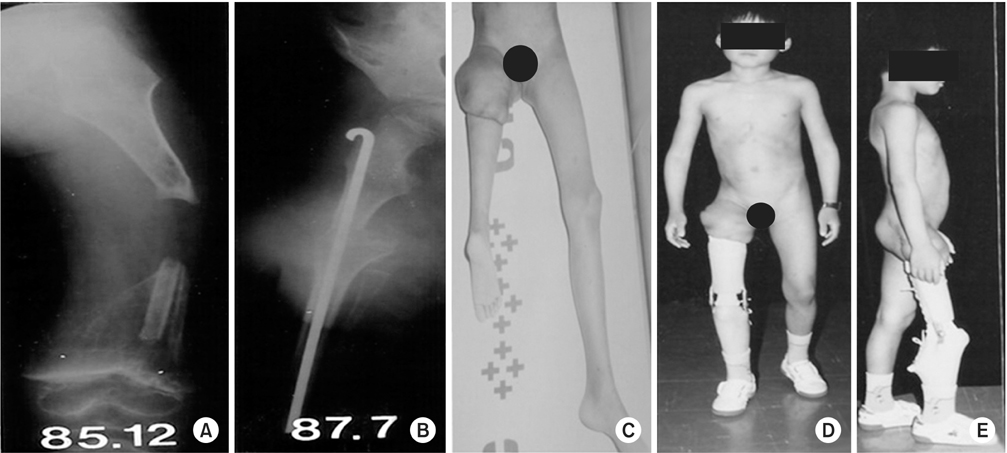
Fig. 1
A 46-year-old male. (A) An open segmental 6 cm defect of tibiawas treated with two trials of sauscerization. Finally, an 8 cm defect was noted (B) and distraction osteogenesis for 4 months was performed (C). During the process, no skin problems on pin tracts, and pain was tolerable. (D) Nine months after the trauma, bony union was successful, knee motions were normal, with limited ankle motions, 0° dorsiflexion and 20° palmar flexion only.
Fig. 2
A 19-year-old female. A severe compound fracture on the proximal femur from a gun shot injury (A); sauscerization was performed 6 times and split skin grafts was done 2 times (B). (C) After cessation of chronic osteomyelitis, a tibial cortico-strut and cancellous chip bone grafts (arrow) with heavy duty condylar plate fixation was performed. Four-and-half years later, a solid bony union was obtained (D, E), but a shortening of the limb by 2 cm was noted (F).
Fig. 3
A 34-year-old male. A 6 cm of tibial (A) and wide skin defects (B) was treated by a 12 cm osteo-cutaneous vascularized fibular graft after 8 weeks of trauma; 7 months later, the grafted fibula was united well and hypertrophied (C), and partial weight bearing was possible (D).
Fig. 4
An 8-year-old boy. A staged medial transport (tibialization) of intact fibula with a 6-week interval (B, C) for the whole defected tibial shaft but intact fibula (A) was observed after performing a wide-split thickness skin graft two times, 3 months after a traffic accident. (D) Six months after the operations, the grafted fibular was united and hypertrophied well, but limping, serious edema by venous stasis on leg was noted. The knee and ankle joint motions were very limitted—nearly stiff—but walking was also possible with a cane. However, the patient and parents were happy for saving the leg.
Fig. 5
A 52-year-old male. An open comminuted fracture on proximal tibia (A) was treated with sauscerization, rotational skin flap, and the 12 cm vascularized fibular graft for 5 cm of bone defect two months after a traffic accident (B). The fracture was occurred because it was too weak to bear any weight, and so a condylar plate with cancellous chip bone graft was performed 4 months after the trauma (C), and the knee range of motion was 10° to 60°.
Fig. 6
(A) A 7-year-old boy had suffered from an uncontrollable osteomyelitis of the femur, with a 14 cm wide segmental defect, despite 6 attempts of sauscerization and 2 attempts of vascularized fibular graft. Initially, an above-the-knee amputaion was seriously considered. However, we performed the Van-Ness's operation associated with a sacrifice of the knee joint, including the infected distal femur and the proximal tibia, and performrd a 180° rotation-plasty of the leg (B, C) to aquire the knee function with ankle. (D, E) He was well tolerated with the rotated foot, which was good to control the brace as a below–knee stump, and the heel functioned as a patella to support the body weight. Nonetheless, psychosocial attention will be required later. We revieved an agreement by patient to carry photoes exposed the face in this paper.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Treatment of Wide Gap Non-Unions in Lower Extremities
Treatment of Wide Gap Non-Unions of the Lower Legs
Table 1
Treatment of Wide Gap Non-Unions of the Lower Legs

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

