Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 20(1); 2007 > Article
-
Original Article
- Comminuted Pilon Fractures: Comparative Outcome Analysis according to Surgical Techniques
- You-Jin Kim, M.D., Hong-Geun Jung, M.D., Ph.D., Joo-Hong Lee, M.D., Woo-Sup Byun, M.D., Sung-Tae Lee, M.D., Ph.D.
-
Journal of the Korean Fracture Society 2007;20(1):6-12.
DOI: https://doi.org/10.12671/jkfs.2007.20.1.6
Published online: June 14, 2016
Department of Orthopedic Surgery, Dankook University College of Medicine, Cheonan, Korea.
*Department of Orthopedic Surgery, Konkuk University School of Medicine, Seoul, Korea.
- Address reprint requests to: Hong-Geun Jung, M.D., Ph.D. Department of Orthopedic Surgery, Konkuk University School of Medicine, 4-12, Hwayang-dong, Gwangjin-gu, Seoul 143-729, Korea. Tel: 82-2-2030-7609, Fax: 82-2-2030-7630, jungfoot@hanmail.net
Copyright © The Korean Fracture Society. All rights reserved
- 1,076 Views
- 10 Download
- 1 Crossref
Abstract
-
Purpose
- To evaluate the overall surgical outcome of the tibial pilon comminuted fractures and perform the comparative analysis between the limited internal fixation-external fixation group and the delayed open reduction-internal fixation (ORIF) group.
-
Materials and Methods
- From June 1997 to June 2004, 17 tibial pilon comminuted fractures were treated with the limited internal fixation-external fixation (6 cases) or the delayed open reduction-internal fixation (11 cases). The average age of the patients was 47.7 years (range: 41~63 years), male was fourteen patients, female was three. Follow-up period was average 33.6 months (range: 12~84 months). The clinical outcomes were evaluated by using AOFAS ankle-hindfoot score and patient satisfaction was also evaluated.
-
Results
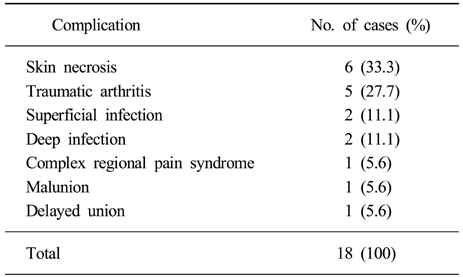
- AOFAS score at final follow-up was 80.4 points, and 88% of the patients were satisfied with the results. AOFAS scores of the external fixation group and the delayed ORIF group were average 77.0 points and 82.2 points respectively, which did not show the statistical difference (p>0.05). Bony union was achieved at average 16.0 weeks. There were 18 complications such as skin necrosis.
-
Conclusion
- We have achieved relatively encouraging functional results and high patient satisfaction for pilon comminuted fractures, without significant result difference between the two surgical techniques.
- 1. Anglen JO. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma, 1999;13:92-97.Article
- 2. Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe t-ibial pilon fractures: a study of three techniques. J Orthop Trauma, 2001;15:153-160.Article
- 3. Bone L, Stegemann P, McNamara K, Seibel R. External fixation of severely comminuted and open tibial pilon fractures. Clin Orthop Relat Res, 1993;292:101-107.Article
- 4. Bourne RB, Rorabeck CH, Macnab J. Intra-articular fractures of the distal tibia: the pilon fracture. J Trauma, 1983;23:591-596.
- 5. Burwell HN, Charnley AD. The treatment of displaced fractures at the ankle by rigid internal fixation and early joint movement. J Bone Joint Surg Br, 1965;47:634-660.ArticlePDF
- 6. Etter C, Ganz R. Long-term results of tibial plafond fractures treated with open reduction and internal fixation. Arch Orthop Trauma Surg, 1991;110:277-283.ArticlePDF
- 7. Giordano CP, Koval KJ. Treatment of fracture blisters: a prospective study of 53 cases. J Orthop Trauma, 1995;9:171-176.Article
- 8. Kellam JF, Waddell JP. Fractures of the distal tibial metaphysis with intra-articular extension - the distal tibial explosion fracture. J Trauma, 1979;19:593-601.Article
- 9. Leung F, Kwok HY, Pun TS, Chow SP. Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury, 2004;35:278-283.Article
- 10. Mast J, Spiegel PG, Pappas J. Fractures of the tibial pilon. Clin Orthop Relat Res, 1988;230:68-82.Article
- 11. Ovadia DN, Beals RK. Fractures of the tibial plafond. J Bone Joint Surg Am, 1986;68:543-551.Article
- 12. Park JT, Ahn GY, Shin YS, Lee YT. A clinical analysis of the tibial pilon fractures with open reduction. J Korean Soc Fract, 1997;10:816-822.Article
- 13. Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma, 1999;13:85-91.Article
- 14. Pierce RO Jr, Heinrich JH. Comminuted intra-articular fractures of the distal tibia. J Trauma, 1979;19:828-832.Article
- 15. Pollak AN, McCarthy ML, Bess RS, Agel J, Swiontkowski MF. Outcomes after treatment of high-energy tibial plafond fractures. J Bone Joint Surg Am, 2003;85:1893-1900.Article
- 16. Ruedi TP, Allgower M. The operative treatment of intraarticular fractures of the lower end of the tibia. Clin Orthop Relat Res, 1979;138:105-110.
- 17. Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma, 1999;13:78-84.Article
- 18. Sohn HM, Lee JY, Ha SH, Choi SM. Treatment of tibial pilon fractures with two-staged delayed open reduction and internal fixation. J Korean Orthop Assoc, 2005;40:188-194.ArticlePDF
- 19. Song KJ, Jung JW, Lee JH, Park MS, Hwang BY. Clinical evaluation for the tibial pilon fractures. J Korean Soc Fract, 1996;9:200-204.Article
- 20. Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res, 1993;292:108-117.
- 21. Tscherne H, Gotzen L. External articular transfixation of joint injuries with severe soft tissue damage. In: Tscherne H, Gotzen L, editors. Fractures with soft tissue injuries. Berlin: Springer-Verlag; 1984. p. 103-117.
- 22. Varela CD, Vaughan TK, Carr JB, Slemmons BK. Fracture blisters: clinical and pathological aspects. J Orthop Trauma, 1993;7:417-427.Article
REFERENCES
(A) This 43 year-old male had a fall injury and sustained a Ruedi-Allgower type III open pilon fracture.

(A) Initial radiograph shows type III severely comminuted pilon fracture of a 42 year-old male.
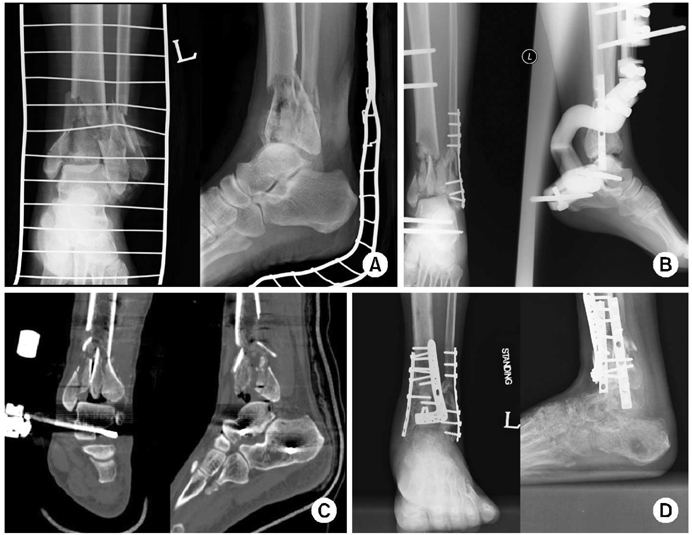
Figure & Data
REFERENCES
Citations

- The Result of Using an Additional Mini-Locking Plate for Tibial Pilon Fractures
Suenghwan Jo, Jun Young Lee, Boseon Kim, Kang Hyeon Ryu
Journal of the Korean Fracture Society.2017; 30(2): 75. CrossRef

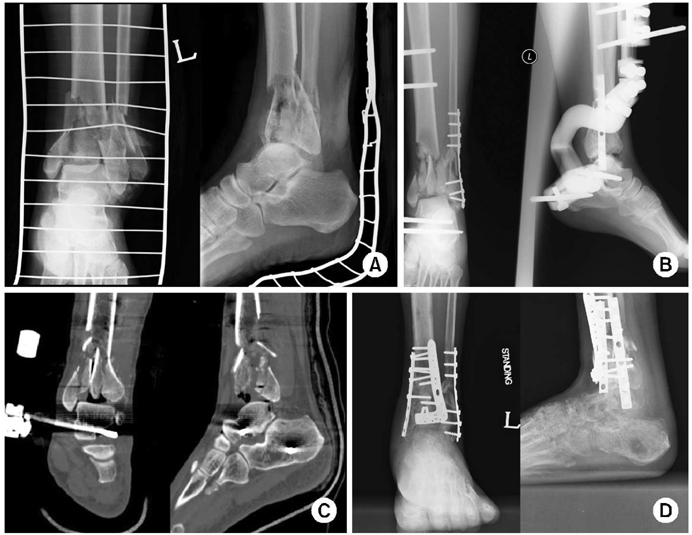
Fig. 1
Fig. 2
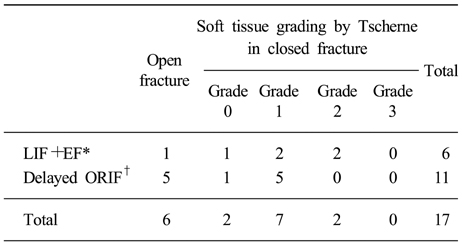
Distribution of open fractures and soft tissue injury patterns in closed fractures
*LIF+EF: Limited internal fixation with external fixation, †ORIF: Open reduction and internal fixation.
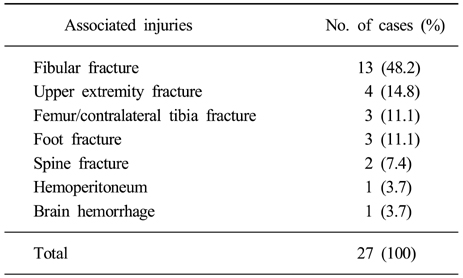
Associated injuries
Demographic data of the patients
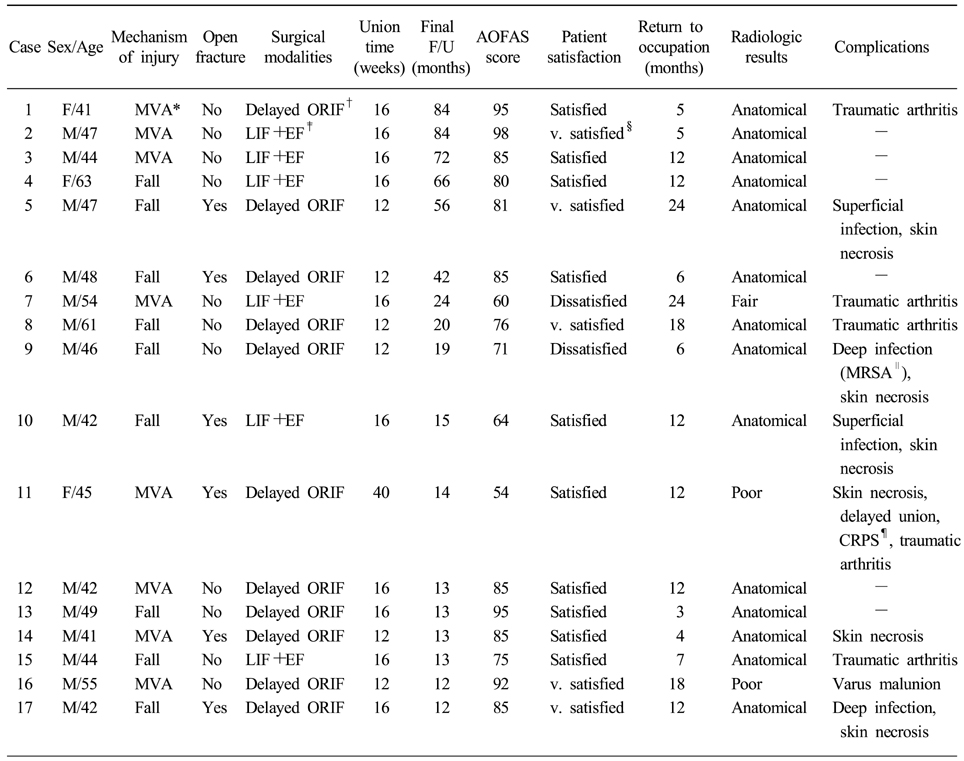
*MVA: Motor vehicle accident, †ORIF: Open reduction and internal fixation, ‡LIF+EF: Limited internal fixation with external fixation, §v. satisfied: Very satisfied, ∥MRSA: Methicillin resistant staphylococcus aureus, ¶CRPS: Complex regional pain syndrome.
Postoperative complications
*LIF+EF: Limited internal fixation with external fixation, †ORIF: Open reduction and internal fixation.
*MVA: Motor vehicle accident, †ORIF: Open reduction and internal fixation, ‡LIF+EF: Limited internal fixation with external fixation, §v. satisfied: Very satisfied, ∥MRSA: Methicillin resistant staphylococcus aureus, ¶CRPS: Complex regional pain syndrome.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

