- Skip Navigation
- Skip to contents

Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(3); 2020 > Article
- Original Article Comparison of a Novel Box-Frame External Fixator and Conventional Delta-Frame External Fixator in the Staged Treatment of Distal Tibia Fractures
- Yong-Cheol Yoon, MinKyu Shin, Chang-Wug Oh, Jong-Keon Oh
-
Journal of Musculoskeletal Trauma 2020;33(3):125-133.
DOI: https://doi.org/10.12671/jkfs.2020.33.3.125
Published online: July 31, 2020

2Department of Orthopedic Surgery, Gachon University College of Medicine, Incheon, Korea

3Department of Orthopedic Surgery, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea

4Department of Orthopedic Surgery, Korea University Guro Hospital, College of Medicine, Korea University, Seoul, Korea

- 1,925 Views
- 16 Download
- 2 Crossref
- 0 Scopus
Abstract
Purpose
Distal tibia fractures with severe soft-tissue edema or intra-articular fractures are treated by staged operations using external fixators. Definitive surgery that maintains ligamentotaxis has been difficult using existing fixators. This study introduced a novel ‘box-frame’ external fixator and evaluated its clinical usefulness.
Materials and Methods
This study included 45 patients (32 males, 13 females) diagnosed with distal tibia fractures who underwent staged operations between March 2012 and March 2016, with a follow-up of at least one year. The patients were divided into two groups. In one group, fixation was performed with a box-frame external fixator (Group A). In the other group, fixation was performed with a delta-frame external fixator (Group B). The following outcomes were evaluated: the time until definitive surgery, operative time of the definitive surgery, radiation exposure time, bone union, time to achieve bone union, postsurgical complications, American Orthopaedic Foot & Ankle Society anklehindfoot score, and ankle range of motion.
Results
Compared to the delta-frame, the box-frame showed a statistically significant reduction in the mean radiation-exposure time and operative time during the definitive surgery by 58 seconds and 25 minutes, respectively. The differences in the time until definitive surgery, bone union, time to achieve bone union, postsurgical complications, and functional scores were not significant.
Conclusion
The box-frame external fixator can be a useful treatment method in the staged surgery of distal tibia fractures.
- Keywords: Distal tibia fracture, Staged operation, External fixator, Box-frame
Published online Jul 24, 2020.
https://doi.org/10.12671/jkfs.2020.33.3.125
Comparison of a Novel Box-Frame External Fixator and Conventional Delta-Frame External Fixator in the Staged Treatment of Distal Tibia Fractures
 , M.D., Ph.D.,
MinKyu Shin
, M.D., Ph.D.,
MinKyu Shin , M.D.,*
Chang-Wug Oh
, M.D.,*
Chang-Wug Oh , M.D., Ph.D.,†
and Jong-Keon Oh
, M.D., Ph.D.,†
and Jong-Keon Oh , M.D., Ph.D.‡
, M.D., Ph.D.‡
- Orthopaedic Trauma Division, Trauma Center, Gachon University College of Medicine, Incheon, Korea.
-
*Department of Orthopedic Surgery, Gachon University College of Medicine, Incheon, Korea.
-
†Department of Orthopedic Surgery, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea.
-
‡Department of Orthopedic Surgery, Korea University Guro Hospital, College of Medicine, Korea University, Seoul, Korea.
- Orthopaedic Trauma Division, Trauma Center, Gachon University College of Medicine, Incheon, Korea.
- Correspondence to: Jong-Keon Oh, M.D., Ph.D. Department of Orthopedic Surgery, Korea University Guro Hospital, College of Medicine, Korea University, 148 Gurodong-ro, Guro-gu, Seoul 08308, Korea. Tel: +82-2-2626-3088, Fax: +82-2-2626-1064, Email: jkoh@korea.ac.kr
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-
Abstract
Purpose
Distal tibia fractures with severe soft-tissue edema or intra-articular fractures are treated by staged operations using external fixators. Definitive surgery that maintains ligamentotaxis has been difficult using existing fixators. This study introduced a novel ‘box-frame’ external fixator and evaluated its clinical usefulness.
Materials and Methods
This study included 45 patients (32 males, 13 females) diagnosed with distal tibia fractures who underwent staged operations between March 2012 and March 2016, with a follow-up of at least one year. The patients were divided into two groups. In one group, fixation was performed with a box-frame external fixator (Group A). In the other group, fixation was performed with a delta-frame external fixator (Group B). The following outcomes were evaluated: the time until definitive surgery, operative time of the definitive surgery, radiation exposure time, bone union, time to achieve bone union, postsurgical complications, American Orthopaedic Foot & Ankle Society ankle-hindfoot score, and ankle range of motion.
Results
Compared to the delta-frame, the box-frame showed a statistically significant reduction in the mean radiation-exposure time and operative time during the definitive surgery by 58 seconds and 25 minutes, respectively. The differences in the time until definitive surgery, bone union, time to achieve bone union, postsurgical complications, and functional scores were not significant.
Conclusion
The box-frame external fixator can be a useful treatment method in the staged surgery of distal tibia fractures.
Introduction
Extra- and intra-articular distal tibia fractures account for 7% to 10% of all tibia fractures and present as a complex injury accompanying fibular fractures in 70% to 85% of cases.1) In addition, complications including delayed bone union, non-union, skin tissue necrosis, and joint stiffness commonly occur due to anatomical characteristics that are associated with increased vulnerability to accompanying injuries of the surrounding soft tissues, including severe comminution due to insufficient surrounding soft tissues, relatively poor blood supply, and thin periosteum.2) Open fractures due to high-energy flexion and rotational forces are also commonly involved.3)
The treatment of this subset of fractures remains controversial and challenging for most orthopedic surgeons. Some authors have suggested that bridging external fixation, with or without limited internal fixation, should be employed for high velocity injuries.4) Others suggest that primary open reduction and internal fixation (OR/IF) should be performed to avoid articular incongruence and the development of axial malalignment.5) However, a two-staged procedure involving primary external fixation and conversion to OR/IF is generally the treatment of choice when treating soft tissue swelling and comminuted fracture.6,7,8) This minimizes soft tissue complications and reduces problems caused by the external fixator itself.
During the conversion of conventional external fixation to definitive internal fixation, the external fixator must be removed prior to or during surgery. This facilitates surgical access to the fracture site and visualization of the fracture reduction and articular congruity using the C-arm. However, there is a high risk of loss of the previously achieved reduction, and articular incongruence may develop after removal of the external fixator, thereby prolonging the operative time and making it more difficult to perform definitive surgery.
To overcome such difficulties, we developed a novel box-frame type of external fixator that can offer parallel linkage between the posterior side of the tibial long axis and the calcaneus, correct the alignment of the fracture site using spanning and ligamentotaxis of the fracture site, maintain external fixators during definitive surgery, and aid in articular reduction and plate fixation. Herein, we report clinically satisfactory outcomes achieved using this box-frame type of external fixator.
Materials and Methods
1. Patient data
Of the patients who were diagnosed with distal tibia fractures between March 2012 and March 2016 at Korea University Guro Hospital and Gachon University Gil Hospital and were treated by staged operations, 45 who were followed-up for at least 1 year were selected for this retrospective analysis. The study included 32 males and 13 females with an mean age of 47.85 years (range, 14–81 years) at the time of surgery. There were 38 cases of closed fractures and 7 cases of open fractures. The mean follow-up period was 17.8 months (range, 12–36 months). The mechanisms of injury included falling down in 12 cases, traffic accidents in 20 cases, slipping in 9 cases, and direct trauma in 4 cases (Table 1). Patients with pathologic fractures, active malignancy, and infections were excluded. The fractures were classified according to the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification using radiographs taken prior to surgery; there were 16, 8, and 21 cases of class 43A, 43B, and 43C fractures, respectively. Class 44 ankle fractures were excluded.9) Staged surgery was performed only when there was severe contamination or severe soft tissue damage or swelling or when the fracture type involved the intra-articular or metaphyseal fracture. Definitive surgery with plates was conducted after achieving soft tissue stabilization and improvement in blood flow following the initial external fixation. The study design and data collection were approved by the institutional review board of the Human Experimental and Ethics Committee of Gachon University Gil Hospital (IRB No. GCIRB 2019-173).
Table 1
Patient Demographic Data and Injury Characteristics
Box-frame external fixators were applied to 27 patients and delta-frame external fixators were applied to 18 patients. All surgeries were conducted by two orthopedic trauma specialists with >10 years of surgical experience. All surgeries conducted prior to designing the box-frame external fixator used the delta-frame external fixators, while those conducted after designing the box-frame used the box-frame external fixators.
2. Surgical procedure
Patients under general or spinal anesthesia were placed in a supine position. To obtain a good anteroposterior (AP) view of the ankle, the lower leg was internally rotated by placing a bump under the buttock area of the affected side. For the patients with an open fracture, thorough and systematic debridement and irrigation were performed while intravenously injecting first-generation cephalosporin as an empirical antibiotic. If the soft tissue was in good condition or the wound was clean, primary closure was performed whenever possible. A topical negative pressure device was applied in the cases of large soft tissue defects.
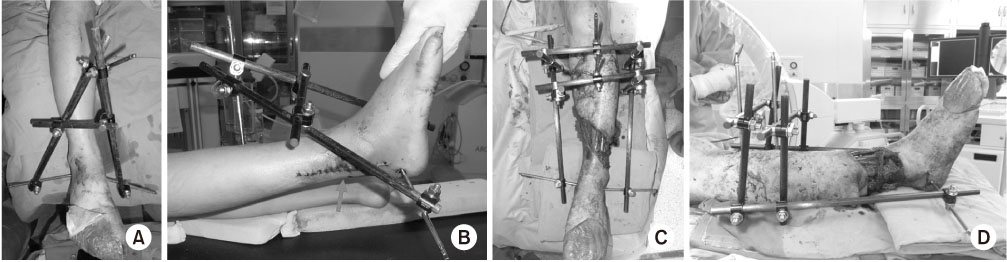
Box-frame external fixators were applied upon completion of massive debridement and copious irrigation. After predicting the length required for the placement of the plate used to fix the fracture site, two 6-mm Schanz pins were inserted into the anterior crest of the tibia while securing a sufficient distance from the proximal end of the plate to prevent the location of the pin from disturbing the procedure and to prevent infection. The tibia shaft is triangular in shape, and insertion of the half pin into the anterior crest, which is an edge rather than a surface, in an AP direction is difficult. Hence, an inner and outer sleeve with a sharp tip was prepared to prevent slipping and tilting. After creating a pilot hole using a 4.3-mm drill bit, the inner sleeve was removed and a 6-mm Schanz pin was inserted through the outer sleeve (Fig. 1). A 6-mm Schanz pin was inserted into each of the medial and lateral sides of the calcaneus through careful blunt dissection at the distal 3/4 point of the line linking the medial malleolar tip and the posteroinferior medial calcaneus to prevent neurovascular complications due to pin insertion. Since the calcaneus is relatively brittle, Schanz pins are directly inserted without creating a pilot hole to increase the pull-out strength.
Fig. 1
Clinical photographs of the delta-frame external fixator (A, B) and the box-frame external fixator (C, D). The bar of the delta-frame is located across the wound where the surgical approach is made (arrow); hence, the external fixator must be removed for internal fixation during definitive surgery. In contrast, the box-frame external fixator allows for exposure of the entire lower leg, enabling easier bone or soft tissue surgery.
Next, a 20- to 25-cm bar in the direction perpendicular to the sagittal plane of the tibial long axis was assembled with a Schanz pin using a clamp. An additional bar was connected in the direction perpendicular to the coronal plane. To complete the construction of the box-frame external fixator, additional rods were placed parallel to the long axis of the tibia, one laterally and one medially. These rods connected the calcaneal Schanz pins with the initial construct assembled at the proximal portion of the tibia. To achieve reduction by ligamentotaxis, traction was applied prior to attaching the two final rods. After assembling the external fixator construct, AP and lateral radiographs were taken with a C-arm to verify reduction and alignment. Special attention was also given to planning for definitive fixation. Importantly, the external fixator did not obstruct areas where the implant could potentially be placed during conversion to definitive internal fixation. Once the swelling and inflammation in the soft tissue subsided, definitive fixation was performed with the fixator in situ.
Since the definitive surgery was performed while maintaining the application of the box-frame external fixator, the presence of any foreign body in the clamp had to be checked and the foreign body removed to ensure disinfection. Then, povidone-iodine was sprayed over the external fixator. The entire surface of the external fixator and the skin were thoroughly wiped with alcohol using a brush. Again, the external fixator and the skin were draped with povidone-iodine using a sprayer and a brush. Special attention was paid not to manipulate the clamp during the procedure. When adjustment of the clamp was inevitably required, the adjustment was made while spraying the alcohol over the clamp and the gloves were changed. Definitive surgery was performed as the ligamentotaxis of the external fixator was kept the same and this allows fair vision of joint space without any additional manipulation; hence, impacted articular fragments can also be reduced and fixed stably and the surgery can be performed according to the preoperative plan.
In the application of the delta-frame external fixator, the locations of the Schanz pins insertions into the tibia and the calcaneus were the same; however, the bar was not parallel to the tibial long axis and the medial and lateral tibia were both directly linked to a calcaneal pin using a rod (Fig. 1). Definitive surgery was conducted after confirming a decrease in soft tissue swelling and the absence of any signs of infection. Unlike the application of the box-frame external fixator, the external fixator was removed prior to the surgery. When careful determination of the presence of an intra-articular lesion is requried, the surgery was conducted by inserting 6 mm Schanz pins into the tibia and talus, installing the femoral distractor, and using a spanning external fixator.
3. Clinical and radiological evaluation
For the intraoperative evaluation, the time from the temporary external fixator application to the definitive surgery, operative time, and radiation exposure time during definitive surgery for the patients in whom the box-frame external fixator was used (Group A) and the patients in whom the delta-frame external fixator was used (Group B) were retrospectively analyzed based on the medical records.
For the postoperative clinical evaluation, the range of motion (ROM) of the ankle measured at the final follow up was evaluated using the American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot score; scores of ≥90, 80–90, and ≤80 were considered excellent, satisfactory, and unsatisfactory, respectively.5)
During the radiological evaluation, the time of bone union and alignment were evaluated. Bone union was defined as bone continuity on at least three surfaces in the AP and lateral views and the absence of pain at the fracture site. Malunion was defined by AP angular or varus/valgus deformity ≥10° and shortening of the affected tibia >10 mm compared to the intact tibia. Each complication was evaluated.7,8)
An independent sample t-test was used to determine statistically significant differences in the parametric means. If the parametric analysis proved unacceptable, a nonparametric method (the Mann–Whitney U test) was used. IBM SPSS Statistics (ver. 21.0; IBM, Armonk, NY USA) was used for all statistical analyses, and a p-value <0.05 was considered to indicate statistical significance.
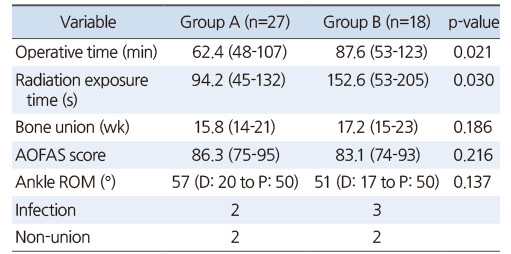
Results
In both groups, neither infection nor reduction loss around the pin-site was found while waiting for definitive surgery. The mean operative time of the definitive surgery was 62.4 minutes (range, 48–107 minutes) in Group A and 87.6 minutes (range, 53–123 minutes) in Group B (p=0.021). In addition, the mean radiation exposure time was 94.2 seconds (range, 45–132 seconds) in Group A and 152.6 seconds (range, 53–205 seconds) in Group B (p=0.030; Table 2). The mean time from the application of the temporary external fixator to the definitive surgery was 12 days (range, 10–17 days) in Group A and 13 days (range, 8–20 days) in Group B, showing no difference between the two groups.
Table 2
Outcomes of Box-Frame and Delta-Frame Groups
Except for the 4 cases that presented with non-union, bone union occurred in 15.8 weeks in Group A and 17.2 weeks in Group B on mean, presenting no statistically significant difference (p=0.186). Although no statistically significant differences were found in angular deformity, ankle ROM, or the AOFAS score between the two groups, there were higher AOFAS scores in Group A than in Group B (Table 2).
Postsurgical complications of angular deformity ≥5° were observed in the final radiologic evaluation, with 2 cases of posterior angulation in Group A and 3 cases of valgus deformity in Group B. However, none of the cases in either group presented as malunion with an angular deformity ≥10°. Non-union was encountered in 2 cases from each of the two groups; all of the non-union cases resulted from open fractures, and bone union was achieved after conducting autogenous bone graft and plate augmentation. Superficial wound infection was encountered in 2 cases from Group A and 3 cases from Group B. Of the 5 wound infection cases, 4 improved with the use of antibiotics alone and 1 case (Group A, Gustilo grade II) recovered through debridement plus antibiotics.
Discussion
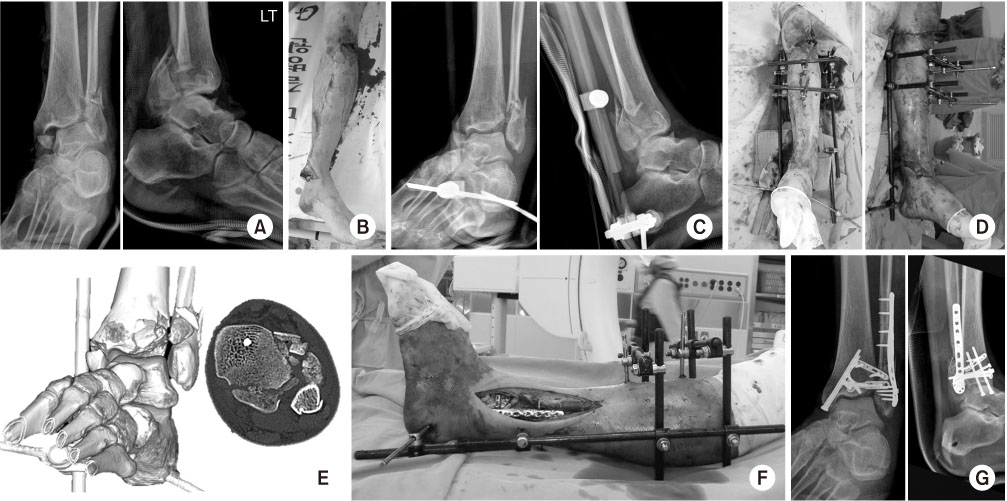
In this study, compared to the conventional delta-frame external fixator, the box-frame external fixator provided better surgical visualization and sufficient space and allowed the surgery to be performed while maintaining ligamentotaxis (Fig. 1,2). This led to a reduction not only in the operative time but also in the radiation exposure as it can directly influence the health of both the operator and the patient. Furthermore, the use of a box-frame external fixator helps the easy anatomic reduction and eliminates the need to re-situate the external fixator on the tibia shaft and talus body to secure a better view of the joint (Fig. 3).
Fig. 2
(A) A simple ankle anteroposterior and lateral radiograph of a 71-year-old female patient presenting with an AO classification 43-B2 fracture and type II open fracture caused by a pedestrian traffic accident. (B, C) The alignment of the fracture site was corrected by conducting irrigation and debridement and applying the box-frame external fixator. (D, E) After allowing the soft tissue to rest for 10 days, tibia-fibular plating using a minimally invasive plate osteosynthesis technique was performed while maintaining the box-frame without other reduction. (F) Full bony union of the fracture site was achieved five months after surgery.
Fig. 3
(A, B) A 54-year-old male patient who visited the hospital due to a traffic accident was diagnosed with ankle dislocation based on a physical examination and with a bilateral ankle fracture, posterior malleolar fracture, and medial gap widening based on simple ankle anteroposterior and lateral radiographs. (C, D) The valgus alignment of the ankle joint was corrected after performing traction by conducting irrigation and debridement and applying the box-frame external fixator. (E) Computed tomography performed afterward revealed the presence of a pilon fracture accompanying the anterior tibia intra-articular fracture. (F, G) Internal fixation was performed using the ligamentotaxis of the box-frame external fixator.
Box frame external fixator is a square-shaped fixator that was designed from the idea of overcoming the inconvenience that temporary external fixator had to be removed when definitive surgery was performed to treat distal tibial fracture. This is the external fixator of the most optimal shape that satisfies all of complicated condition including maintaining the ligamentotaxis the same, providing good vision of surgical field during definitive surgery, and not disturbing the surgeon's procedure. These advantages can reduce radiation exposure and operative time and secure fixation strength with relatively simple method that is easy to follow by looking at pictures.
In terms of decreasing both infection rates and soft tissue complication rates with the use of an external fixator, many studies have reported good to excellent results for high velocity injuries.10,11,12) However, this cannot be regarded as a definitive treatment for these types of fractures, as secondary surgery with OR/IF is almost always essential. Depending on the location, the shape of the external fixator may vary by the severity and pattern of the fractures; in many studies, delta-frame external fixators have been positioned by placing half pins in a triangular shape on the anterior tibia shaft, the medial side of the foot, and the lateral side of the foot and aligned through the distraction of the fracture site.13,14,15) The advantage of the delta-frame external fixator is that it is stable as a bar is located on the shortest line linking the two pins regardless of the long axis. However, this also represents a disadvantage of the delta-frame external fixator, since it disrupts the view of the surgeons and the approach, reduction, and plate fixation processes, thereby necessitating removal of the external fixator to secure access for screw insertion. Moreover, the removal of the delta-frame breaks the ligamentotaxis and requires an additional procedure of ex-fix placement during the surgery in order to check the intra-articular lesion, thereby prolonging the operative time.
One study compared clinical outcomes between a unilateral ankle spanning external fixator and a hybrid ankle sparing external fixator that combined a unilateral frame with the Ilizarov system and reported a higher occurrence of malunion and traumatic osteoarthritis with the ankle spanning external fixator.16) This is thought to be because ligamentotaxis was not achieved by the traction of one axis alone with the unilateral external fixator. The Ilizarov external fixator has two or more wires that allow the alignment of the ankle joint to be maintained during the traction. However, the ability to maintain the Ilizarov fixator during OR/IF in definitive surgery is not expected due to the circular ring and wire of the Ilizarov. Good outcomes have been achieved through the use of the hybrid external fixator during definitive surgery depending on the condition of the soft tissue and the fracture pattern.17,18) However, anatomic reduction and stable fixation, which are the principle foundations of articular fracture treatment, are difficult to ensure with this type of external fixator, and long-term application may lead to increased risk of ankle joint stiffness and pin site infection.19)
Using another method of treatment, Tornetta et al.20) reported satisfactory outcomes after performing limited OR/IF in combination with the circular external fixator for the treatment of a pilon fracture, which is difficult to treat. However, this method also does not provide a direct view of the joint; hence, accurate reduction and fixation are still challenging and its use is limited in type C1 and C2 intra-articular simple fractures because the external fixator pins need to remain until bony consolidation is complete, which may inconvenience the patient. This highlights the difficulty of the treatment of pilon fractures despite the many treatment methods that have been proposed.21,22)
When proceeding with staged surgery keeping the external fixator intact, concerns of infection due to the external fixator may arise. Hak et al.23) reported that standard povidone-iodine alone was not sufficient to suppress the bacteria and that numerous bacterial colonies may exist on and be contacted through the crevices of the clamp while loosening it; in addition, a number of studies have argued that the infection rate must be reduced by performing many steps of pre-draping procedure.23,24,25) In the present study, every surgery was performed using a three-step disinfection procedure and the infection rates were not higher in the patients who underwent surgery after removal of the external fixator. When loosening of the clamp was needed, alcohol was sprayed around the clamp and the superficial glove was changed.
The box-frame external fixator configuration has some disadvantages. Structurally, it is not as rigid as the delta-frame or ankle spanning frames. Thus, it is recommended as a temporary fixation for distal tibia-fibula fractures prior to conversion to definitive internal fixation. We believe that its stability may be increased by using a single Denham pin instead of two half pins in the calcaneus, since this reduces the bending forces caused by the cantilever mechanism. In the cases of severe articular comminution and joint depression, ligamentotaxis may not provide adequate reduction and distraction of the spanning external fixator may interrupt the articular fracture reduction. However, because this is due to a fracture characteristic rather than a problem with the box-frame fixator, it can be resolved by loosening the distal clamps of the box-frame fixator during surgery.
This study was limited by the relatively small number of patients, as only patients who underwent fixation through staged operations, rather than all patients with distal tibia fractures, were included. Patient compliance was not considered in this study. A relatively short follow-up period limited the evaluation of clinical outcomes such as traumatic arthritis, which is a late-stage complication occurring in some intra-articular fracture patients. However, the effectiveness of this fixation method was still evident considering that the severe complications of general fractures usually occur at an early stage postoperatively. Lastly, this was a retrospective study to evaluate the effectiveness of the box-frame external fixator based on clinical and radiologic outcomes; further prospective research is required.
Conclusion
In staged operations for distal tibia fractures, application of the box-frame external fixator enabled reduction and fixation using ligamentotaxis through spanning without removal of the external fixators during definitive surgery. Therefore, box-frame fixation may be a useful method that reduces the operative time and radiation exposure, makes the surgery relatively easy, and provides both excellent surgical visualization and sufficient space for all stages of the procedure.
Financial support:None.
Conflict of interests:None.
References
-
Müller FJ, Nerlich M. Tibial pilon fractures. Acta Chir Orthop Traumatol Cech 2010;77:266–276.
-
Citations

- Temporary Circular External Fixation for Spanning the Traumatized Ankle Joint
Nando Ferreira, Niel Bruwer, Adriaan Jansen van Rensburg, Ernest Muserere, Shao-Ting Jerry Tsang
JBJS Essential Surgical Techniques.2024;[Epub] CrossRef - Temporary circular external fixation for spanning the traumatised ankle joint: A cohort comparison study
William D. Harrison, Franklin Fortuin, Matthieu Durand-Hill, Etienne Joubert, Nando Ferreira
Injury.2022; 53(10): 3525. CrossRef

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS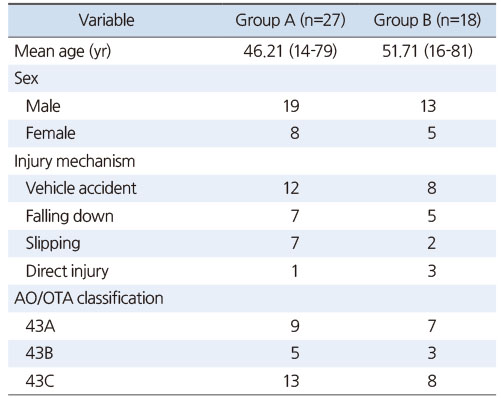

 Cite
Cite

