Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 28(4); 2015 > Article
-
Original Article
- Operative Treatment of Pediatric Distal Forearm Bothbone Fracture
- Sang-Uk Lee, M.D., Ph.D., Changhoon Jeong, M.D., Ph.D., Il-Jung Park, M.D., Ph.D., Jaeyoung Lee, M.D., Seman Oh, M.D., Kyung-Hoon Lee, M.D., Sanghyun Jeon, M.D.
-
Journal of the Korean Fracture Society 2015;28(4):237-244.
DOI: https://doi.org/10.12671/jkfs.2015.28.4.237
Published online: October 19, 2015
Department of Orthopaedic Surgery, The Catholic University of Korea, Bucheon St. Mary's Hospital, Bucheon, Korea.
- Address reprint requests to: Changhoon Jeong, M.D., Ph.D. Department of Orthopaedic Surgery, The Catholic University of Korea, Bucheon St. Mary's Hospital, 327 Sosa-ro, Wonmi-gu, Bucheon 14647, Korea. Tel: 82-32-340-7089, Fax: 82-32-340-2671, changhoonj@naver.com
• Received: August 8, 2015 • Revised: September 21, 2015 • Accepted: September 21, 2015
Copyright © 2015 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 418 Views
- 1 Download
Abstract
-
Purpose
- Pediatric patients with distal forearm bothbone fractures of surgical indication were treated with the Kapandji reduction technique for radius and flexible intramedullary nail for ulna at our institution. The purpose of this study is to evaluate clinical and radiological results.
-
Materials and Methods
- From February 2012 to June 2014, we retrospectively evaluated 16 out of 18 cases with distal forearm bothbone fractures treated with the Kapandji reduction technique for radius and flexible intramedullary nail for ulna with at least 1-year follow-up. The average age at operation was 9.1 years (7-13 years).
-
Results
- Adequate reduction for both radius and ulna was achieved for all cases, and none of the cases showed re-displacement until the last follow-up. Mean 6.6 weeks lapsed until bony union was observed for the radius. For the ulna, the mean was 6.5 weeks. All patients gained full wrist range of motion at the last visit.
-
Conclusion
- For pediatric distal forearm bothbone fractures, intrafocal Kapandji reduction and internal fixation with Kirschner wire for radius and reduction and internal fixation with a flexible intramedullary nail for ulna is the technique for handy reduction. Use of this technique can prevent re-displacement during the union process and achieve excellent clinical and radiologic results.
- 1. Randsborg PH, Gulbrandsen P, Saltytė Benth J, et al. Fractures in children: epidemiology and activity-specific fracture rates. J Bone Joint Surg Am, 2013;95:e42.
- 2. Canale ST, Beaty JH. Campbell's operative orthopaedics. 12th ed. Philadelphia: Elsevier Health Sciences; 2012. p. 1376.
- 3. Haddad FS, Williams RL. Forearm fractures in children: avoiding redisplacement. Injury, 1995;26:691-692.
- 4. McLauchlan GJ, Cowan B, Annan IH, Robb JE. Management of completely displaced metaphyseal fractures of the distal radius in children. A prospective, randomised controlled trial. J Bone Joint Surg Br, 2002;84:413-417.
- 5. Proctor MT, Moore DJ, Paterson JM. Redisplacement after manipulation of distal radial fractures in children. J Bone Joint Surg Br, 1993;75:453-454.PDF
- 6. Harring JA. Tachdjian's pediatric orthopaedics. 4th ed. Philadelphia, WE Saunders Co: 2008. p. 2556.
- 7. Pannu GS, Herman M. Distal radius-ulna fractures in children. Orthop Clin North Am, 2015;46:235-248.
- 8. Parikh SN, Jain VV, Youngquist J. Intrafocal pinning for distal radius metaphyseal fractures in children. Orthopedics, 2013;36:783-788.
- 9. Strohm PC, Müller CA, Boll T, Pfister U. Two procedures for Kirschner wire osteosynthesis of distal radial fractures. A randomized trial. J Bone Joint Surg Am, 2004;86:2621-2628.
- 10. Zamzam MM, Khoshhal KI. Displaced fracture of the distal radius in children: factors responsible for redisplacement after closed reduction. J Bone Joint Surg Br, 2005;87:841-843.
- 11. Jubel A, Andermahr J, Isenberg J, Issavand A, Prokop A, Rehm KE. Outcomes and complications of elastic stable intramedullary nailing for forearm fractures in children. J Pediatr Orthop B, 2005;14:375-380.
- 12. Smith VA, Goodman HJ, Strongwater A, Smith B. Treatment of pediatric both-bone forearm fractures: a comparison of operative techniques. J Pediatr Orthop, 2005;25:309-313.
- 13. Eichinger JK, Agochukwu U, Franklin J, Arrington ED, Bluman EM. A new reduction technique for completely displaced forearm and wrist fractures in children: a biomechanical assessment and 4-year clinical evaluation. J Pediatr Orthop, 2011;31:e73-e79.
- 14. Zimmermann R, Gschwentner M, Kralinger F, Arora R, Gabl M, Pechlaner S. Long-term results following pediatric distal forearm fractures. Arch Orthop Trauma Surg, 2004;124:179-186.PDF
- 15. McQuinn AG, Jaarsma RL. Risk factors for redisplacement of pediatric distal forearm and distal radius fractures. J Pediatr Orthop, 2012;32:687-692.
- 16. Satish BR, Vinodkumar M, Suresh M, Seetharam PY, Jaikumar K. Closed reduction and K-wiring with the Kapandji technique for completely displaced pediatric distal radial fractures. Orthopedics, 2014;37:e810-e816.
- 17. Choi KY, Chan WS, Lam TP, Cheng JC. Percutaneous Kirschner-wire pinning for severely displaced distal radial fractures in children. A report of 157 cases. J Bone Joint Surg Br, 1995;77:797-801.PDF
- 18. Miller BS, Taylor B, Widmann RF, Bae DS, Snyder BD, Waters PM. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: a prospective, randomized study. J Pediatr Orthop, 2005;25:490-494.
REFERENCES
Fig. 1

(A) Pin-leverage technique to lever up the distal fragment of the radius. (B) Nancy nail™ (flexible intramedullary nail) is inserted toward distal fragment (arrow) to achieve reduction.

Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

Operative Treatment of Pediatric Distal Forearm Bothbone Fracture
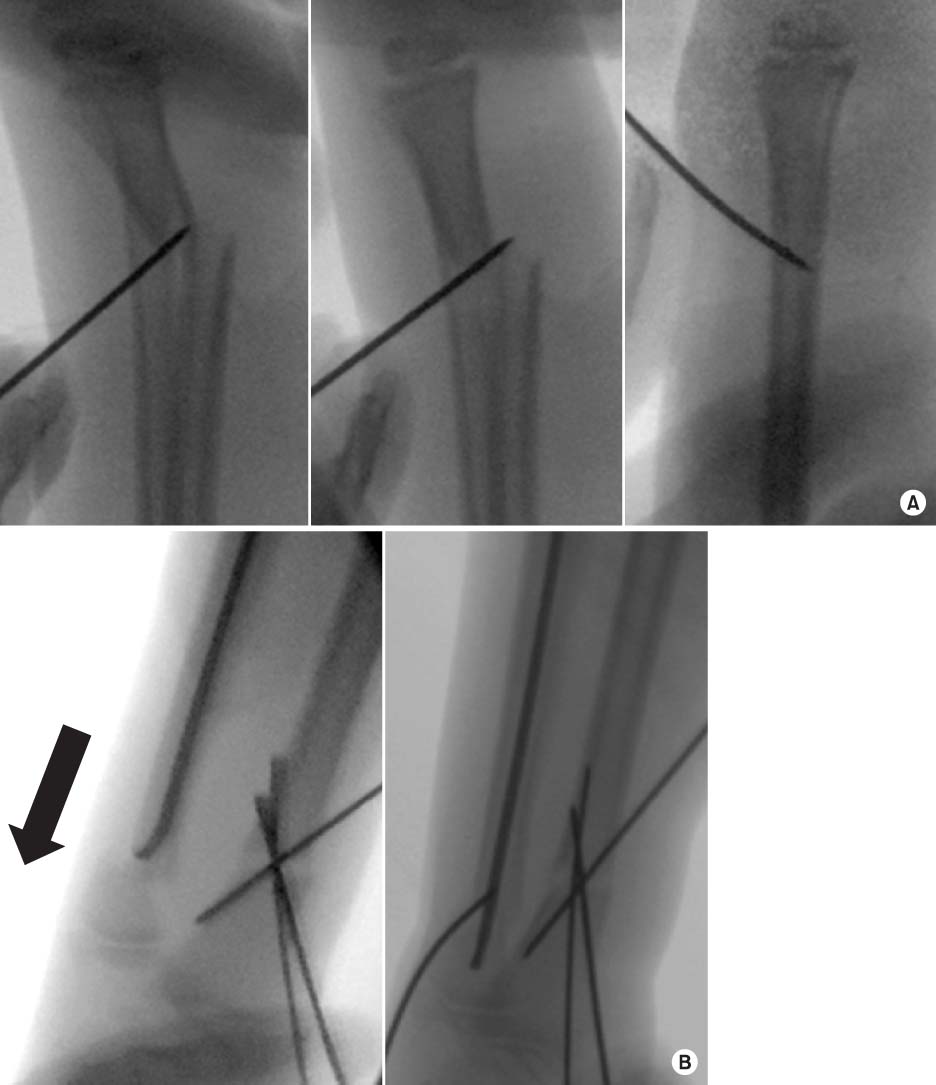
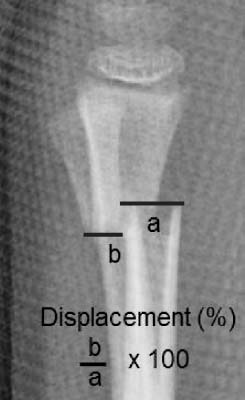

Fig. 1
(A) Pin-leverage technique to lever up the distal fragment of the radius. (B) Nancy nail™ (flexible intramedullary nail) is inserted toward distal fragment (arrow) to achieve reduction.
Fig. 2
Measurement of displacement (%). a: width of proximal segment, b: displaced distance.
Fig. 3
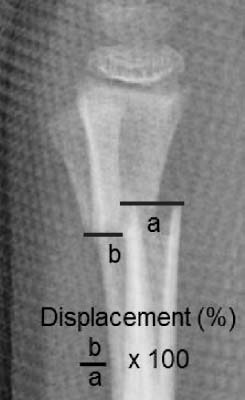
(A) Both distal radius and ulna fracture of an 11-year-old boy. (B) Immediate postoperative X-ray. (C) Eight months after surgery.
Fig. 1
Fig. 2
Fig. 3
Operative Treatment of Pediatric Distal Forearm Bothbone Fracture
Radiographic Measurements
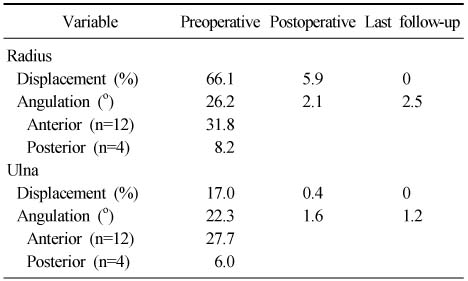
Table 1
Radiographic Measurements

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

