Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 30(4); 2017 > Article
-
Original Article
- Comparison of the Treatment Results between Reduction with Percutaneous Wiring and Reduction without Percutaneous Wiring in Reverse Oblique Trochanteric Fractures (AO Classification 31-A3.3)
-
Jae Woo Park, M.D.
 , Oog Jin Shon, M.D., Ph.D.
, Oog Jin Shon, M.D., Ph.D. , Seung Wan Lim, M.D.
, Seung Wan Lim, M.D.
-
Journal of the Korean Fracture Society 2017;30(4):192-197.
DOI: https://doi.org/10.12671/jkfs.2017.30.4.192
Published online: October 25, 2017
Department of Orthopedic Surgery, Yeungnam University Medical Center, Yeungnam University College of Medicine, Daegu, Korea.
- Correspondence to: Oog Jin Shon, M.D., Ph.D. Department of Orthopedic Surgery, Yeungnam University Medical Center, 170 Hyeonchung-ro, Nam-gu, Daegu 42415, Korea. Tel: +82-53-620-3640, Fax: +82-53-628-4020, ospark@ynu.ac.kr
Copyright © 2017 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 339 Views
- 0 Download
Abstract
-
Purpose
- The aim of this study was to investigate the utility of percutaneous wiring in the reduction of reverse oblique trochanteric fractures (AO classification 31-A3.3) by analyzing the treatment results with or without the use of percutaneous wiring.
-
Materials and Methods
- Thirty-five cases from January 2008 to August 2014 that could be followed-up for at least one year were selected among patients with unstable trochanteric fractures who underwent either internal fixation or open reduction. Seventeen patients underwent surgery with percutaneous wire fixation but another 18 patients underwent surgery without it. All patients received a closed reduction and internal fixation with an intramedullary nail. The factors evaluated were as follows: the length of operation, loss of blood, length of in-hospital stay, lower limb function scale, return to preinjury daily life, change in femur neck shaft angle, postoperative gap of the fracture site, time taken for bone attachment, quality of post-operative reduction, and complications.
-
Results
- No significant difference in the mean operative time, loss of blood, length of in hospital stay, lower limb function scale, return to pre-injury daily life, change in femur neck shaft angle, postoperative gap of the fracture site, and quality of postoperative reduction was observed between the two groups. A significant difference was noted in the time taken for bone attachment (p=0.032). Bone attachment took 13.3 weeks (9–17 weeks) on average when fixed with percutaneous wiring and no patient was found to have any complications. When treated without percutaneous wiring, however, bone attachment took 17.8 weeks (12.5–28.0 weeks) on average and three cases resulted in delayed union.
-
Conclusion
- Percutaneous wiring is a recommended treatment option for patients with an unstable trochanteric fracture.
- 1. Nikolaou VS, Papathanasopoulos A, Giannoudis PV. What's new in the management of proximal femoral fractures? Injury, 2008;39:1309-1318.Article
- 2. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br, 2002;84:1093-1110.
- 3. de Vries JS, Kloen P, Borens O, Marti RK, Helfet DL. Treatment of subtrochanteric nonunions. Injury, 2006;37:203-211.Article
- 4. Loizou CL, McNamara I, Ahmed K, Pryor GA, Parker MJ. Classification of subtrochanteric femoral fractures. Injury, 2010;41:739-745.Article
- 5. Kennedy MT, Mitra A, Hierlihy TG, Harty JA, Reidy D, Dolan M. Subtrochanteric hip fractures treated with cerclage cables and long cephalomedullary nails: a review of 17 consecutive cases over 2 years. Injury, 2011;42:1317-1321.Article
- 6. Apivatthakakul T, Phaliphot J, Leuvitoonvechkit S. Percutaneous cerclage wiring, does it disrupt femoral blood supply? A cadaveric injection study. Injury, 2013;44:168-174.Article
- 7. Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther, 1999;79:371-383.
- 8. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am, 1995;77:1058-1064.Article
- 9. Asher MA, Tippett JW, Rockwood CA, Zilber S. Compression fixation of subtrochanteric fractures. Clin Orthop Relat Res, 1976;(117):202-208.Article
- 10. Kinast C, Bolhofner BR, Mast JW, Ganz R. Subtrochanteric fractures of the femur. Results of treatment with the 95 degrees condylar blade-plate. Clin Orthop Relat Res, 1989;(238):122-130.
- 11. Siebenrock KA, Müller U, Ganz R. Indirect reduction with a condylar blade plate for osteosynthesis of subtrochanteric femoral fractures. Injury, 1998;29:Suppl 3. C7-C15.Article
- 12. Trafton PG. Subtrochanteric-intertrochanteric femoral fractures. Orthop Clin North Am, 1987;18:59-71.Article
- 13. Apivatthakakul T, Phornphutkul C. Percutaneous cerclage wiring for reduction of periprosthetic and difficult femoral fractures. A technical note. Injury, 2012;43:966-971.Article
- 14. Perren SM, Fernandez Dell'Oca A, Lenz M, Windolf M. Cerclage, evolution and potential of a Cinderella technology. An overview with reference to periprosthetic fractures. Acta Chir Orthop Traumatol Cech, 2011;78:190-199.Article
- 15. Apivatthakakul T, Phornphutkul C, Bunmaprasert T, Sananpanich K, Fernandez Dell'Oca A. Percutaneous cerclage wiring and minimally invasive plate osteosynthesis (MIPO): a percutaneous reduction technique in the treatment of Vancouver type B1 periprosthetic femoral shaft fractures. Arch Orthop Trauma Surg, 2012;132:813-822.ArticlePDF
- 16. Afsari A, Liporace F, Lindvall E, Infante A Jr, Sagi HC, Haidukewych GJ. Clamp-assisted reduction of high subtrochanteric fractures of the femur. J Bone Joint Surg Am, 2009;91:1913-1918.Article
- 17. Kim JW, Park KC, Oh JK, Oh CW, Yoon YC, Chang HW. Percutaneous cerclage wiring followed by intramedullary nailing for subtrochanteric femoral fractures: a technical note with clinical results. Arch Orthop Trauma Surg, 2014;134:1227-1235.ArticlePDF
- 18. Müller T, Topp T, Kühne CA, Gebhart G, Ruchholtz S, Zettl R. The benefit of wire cerclage stabilisation of the medial hinge in intramedullary nailing for the treatment of subtrochanteric femoral fractures: a biomechanical study. Int Orthop, 2011;35:1237-1243.ArticlePDF
REFERENCES
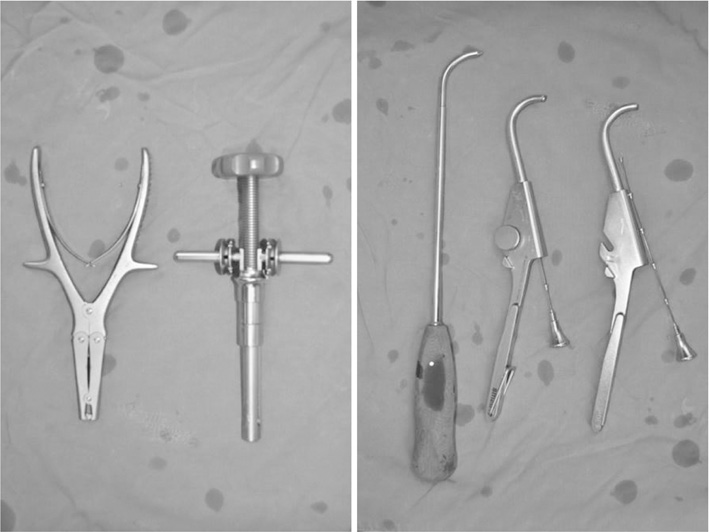
After anatomical reduction was achieved, a nail was inserted and then final reduction was made with percutaneous cerclage wiring.

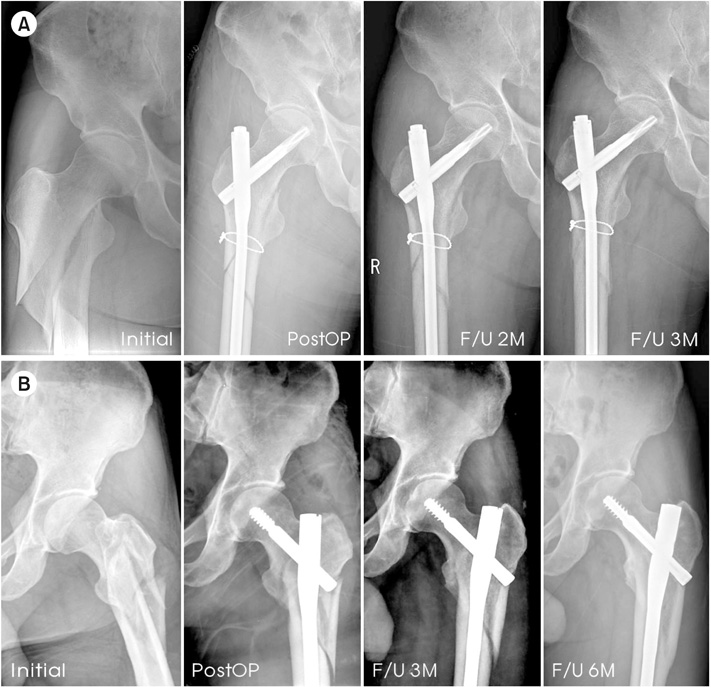
(A) A 48-year-old man with wiring: initial, immediately after surgery, 2-month follow-up (F/U) and 3-month F/U on a simple radiograph. (B) A 59-yearold man without wiring: initial, immediately after surgery, 3-month F/U and 6-month F/U on a simple radiograph. PostOP: postoperative.
Demographic Data
Clinical Results
Figure & Data
REFERENCES
Citations


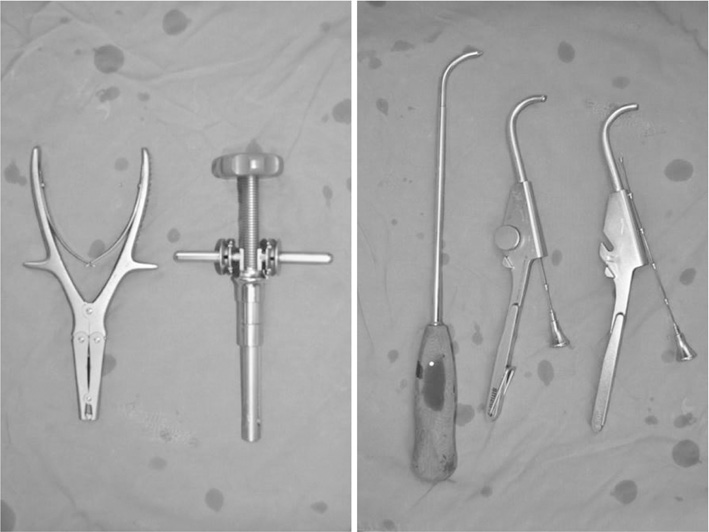
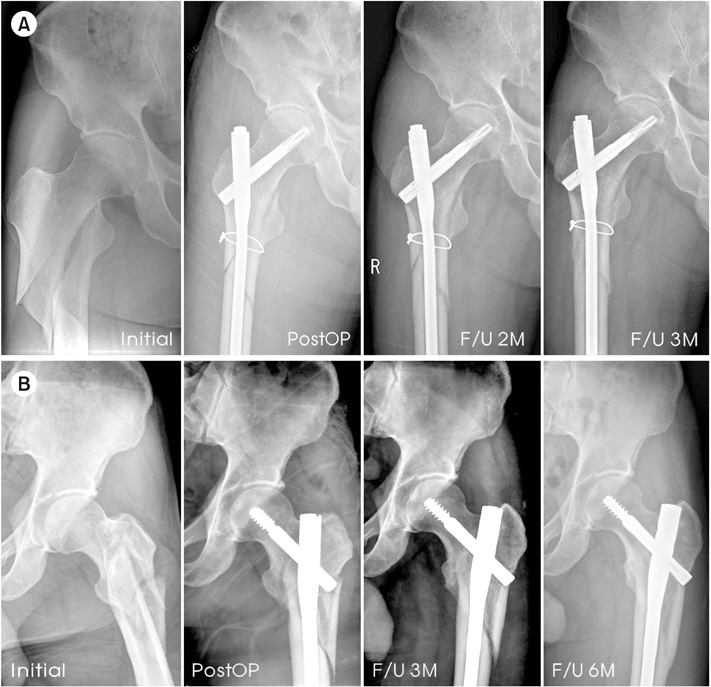
Fig. 1
Fig. 2
Fig. 3
Demographic Data
| Variable | With wiring (17 cases) |
Without wiring (18 cases) |
|---|---|---|
| Device | PFNA II: 10 | PFNA: 10 |
| ITST: 3 | ITST: 3 | |
| CM nail: 4 | Sirus nail: 5 | |
| Sex (male/female) | 14/3 | 15/3 |
| Mean age (yr) | 54 (18–72) | 65 (38–81) |
| BMI (kg/m2) | 22.5 (19.3–26.5) | 21.7 (18.5–24.2) |
| Mean F/U (mo) | 18.2 (13–42) | 45.7 (24–81) |
Values are presented as number only or median (range). PFNA: proximal femoral nail antirotation, ITST: intertrochanteric/subtrochanteric fixation system, CM: cephalomedulary, BMI: body mass index, F/U: follow-up.
Clinical Results
| Variable | With wiring | Without wiring |
|---|---|---|
| Mean operative time (min) | 100 (50–145) | 99.5 (40–150) |
| Hospital day (d) | 24.6 (8–59) | 20.3 (10–46) |
| Blood loss (ml) | 186 (50–300) | 198 (40–400) |
| Change in lower limb function scale | 4.5 (3–9) | 6.2 (4–9) |
| Return to daily life (mo) | 7 (4–12) | 9 (7–15) |
Values are presented as median (range).
Radiological Results
| Variable | With wiring | Without wiring | p-value |
|---|---|---|---|
| Bone attachment time (wk) | 13.3 (9–17) | 17.8 (12.5–28.0) | 0.032 |
| Change in neck-shaft angle (°) | 1.4±2.3 | 1.2±3.1 | >0.05 |
| Postoperative gap (mm) | 0.2 (0–0.5) | 1.7 (0.8–2.5) | >0.05 |
Values are presented as median (range) or mean±standard deviation.
Complications
| Complication | With wiring | Without wiring | Total |
|---|---|---|---|
| Delayed union | 0 | 3 | 3 |
| Nonunion | 0 | 0 | 0 |
| Shortening (>2 cm) | 0 | 0 | 0 |
| Infection | 0 | 0 | 0 |
Values are presented as number only.
Values are presented as number only or median (range). PFNA: proximal femoral nail antirotation, ITST: intertrochanteric/subtrochanteric fixation system, CM: cephalomedulary, BMI: body mass index, F/U: follow-up.
Values are presented as median (range).
Values are presented as median (range) or mean±standard deviation.
Values are presented as number only.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

