Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 29(2); 2016 > Article
-
Original Article
- A Comparative Study of TRIGENâ„¢ INTERTAN Nail (InterTAN) and Proximal Femoral Nail Antirotation 2 (PFNA2) in the Patients with Intertrochanteric Fractures
- Jae-Hoon Jang, M.D., Jeung Il Kim, M.D., Ph.D., Um Ji Kim, M.D., Nam Hoon Moon, M.D.
-
Journal of the Korean Fracture Society 2016;29(2):128-136.
DOI: https://doi.org/10.12671/jkfs.2016.29.2.128
Published online: April 19, 2016
Department of Orthopaedic Surgery, Pusan National University School of Medicine, Busan, Korea.
- Address reprint requests to: Nam Hoon Moon, M.D. Department of Orthopaedic Surgery, Pusan National University Hospital, 179 Gudeok-ro, Seo-gu, Busan 49241, Korea. Tel: 82-51-240-7248, Fax: 82-51-240-8395, namhoonmoon@gmail.com
Copyright © 2016 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 682 Views
- 3 Download
- 1 Crossref
Abstract
-
Purpose
- The primary purpose of this study was to demonstrate that the TRIGEN™ INTERTAN nail (InterTAN) could show better clinical outcome compared to the proximal femoral nail antirotation 2 (PFNA2) for treatment of intertrochanteric fracture in the elderly.
-
Materials and Methods
- Between March 2009 and December 2013, 164 patients with intertrochanteric fractures who met our inclusion and exclusion criteria were enrolled in this study. Evaluation variables, including operation time, blood loss during the operation, incidence of perioperative complications, clinical results at the last follow-up, and radiographic findings were assessed for comparison of the 2 implants.
-
Results
- Intraoperative lateral wall fracture was significantly higher in the PFNA2 group (p<0.05) and tip apex distance was significantly higher in the InterTAN group (p<0.05). Sliding of the proximal fragment at the last follow-up was significantly higher in the PFNA2 group. However, there was no significant difference in union rate, time to union, postoperative complications, and clinical outcomes at the last follow-up between the 2 groups.
-
Conclusion
- Based on these data, clinical outcomes at the last follow-up were equivalent between InterTAN and PFNA2.
- 1. Liu M, Yang Z, Pei F, Huang F, Chen S, Xiang Z. A meta-analysis of the Gamma nail and dynamic hip screw in treating peritrochanteric fractures. Int Orthop, 2010;34:323-328.PDF
- 2. Ricci WM, Spiguel A, McAndrew C, Gardner M. What's new in orthopaedic trauma. J Bone Joint Surg Am, 2013;95:1333-1342.
- 3. Simmermacher RK, Bosch AM, Van der Werken C. The AO/ASIF-proximal femoral nail (PFN): a new device for the treatment of unstable proximal femoral fractures. Injury, 1999;30:327-332.
- 4. Sadic S, Custovic S, Jasarevic M, et al. Proximal femoral nail antirotation in treatment of fractures of proximal femur. Med Arh, 2014;68:173-177.
- 5. Zhang S, Zhang K, Jia Y, Yu B, Feng W. InterTan nail versus proximal femoral nail Antirotation-Asia in the treatment of unstable trochanteric fractures. Orthopedics, 2013;36:e288-e294.
- 6. Ruecker AH, Rupprecht M, Gruber M, et al. The treatment of intertrochanteric fractures: results using an intramedullary nail with integrated cephalocervical screws and linear compression. J Orthop Trauma, 2009;23:22-30.
- 7. Huang Y, Zhang C, Luo Y. A comparative biomechanical study of proximal femoral nail (InterTAN) and proximal femoral nail antirotation for intertrochanteric fractures. Int Orthop, 2013;37:2465-2473.PDF
- 8. Kim JW, Kim TY, Ha YC, Lee YK, Koo KH. Outcome of intertrochanteric fractures treated by intramedullary nail with two integrated lag screws: a study in Asian population. Indian J Orthop, 2015;49:436-441.
- 9. Chinzei N, Hiranaka T, Niikura T, et al. Accurate and easy measurement of sliding distance of intramedullary nail in trochanteric fracture. Clin Orthop Surg, 2015;7:152-157.
- 10. Corrales LA, Morshed S, Bhandari M, Miclau T 3rd. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am, 2008;90:1862-1868.
- 11. Simmermacher RK, Ljungqvist J, Bail H, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury, 2008;39:932-939.
- 12. Li J, Cheng L, Jing J. The Asia proximal femoral nail antirotation versus the standard proximal femoral antirotation nail for unstable intertrochanteric fractures in elderly Chinese patients. Orthop Traumatol Surg Res, 2015;101:143-146.
- 13. Lee SY, Niikura T, Iwakura T, Sakai Y, Kuroda R, Kurosaka M. Complete traumatic backout of the blade of proximal femoral nail antirotation: a case report. Orthop Traumatol Surg Res, 2014;100:441-443.
- 14. Tao YL, Ma Z, Chang SM. Does PFNA II avoid lateral cortex impingement for unstable peritrochanteric fractures? Clin Orthop Relat Res, 2013;471:1393-1394.
- 15. Macheras GA, Koutsostathis SD, Galanakos S, Kateros K, Papadakis SA. Does PFNA II avoid lateral cortex impingement for unstable peritrochanteric fractures? Clin Orthop Relat Res, 2012;470:3067-3076.
- 16. Li J, Xu XZ, You T, Li H, Jing JH. Early results of the proximal femoral nail antirotation-Asia for intertrochanteric fractures in elderly Chinese patients. Saudi Med J, 2014;35:385-390.
- 17. Wu D, Ren G, Peng C, Zheng X, Mao F, Zhang Y. InterTan nail versus Gamma3 nail for intramedullary nailing of unstable trochanteric fractures. Diagn Pathol, 2014;9:191.
- 18. Matre K, Vinje T, Havelin LI, et al. TRIGEN INTERTAN intramedullary nail versus sliding hip screw: a prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up. J Bone Joint Surg Am, 2013;95:200-208.
REFERENCES
(A) Preoperative hip anteroposterior (AP) radiograph of a 65-year-old male patient showing an intertrochanteric fracture (AO2-2) of the left proximal femur. (B) Postoperative radiograph showing Inter-TAN fixation of the intertrochanteric fracture. (C) At the last follow-up, union was achieved. (D) Preoperative hip AP radiograph of a 72-yearold male patient showing an intertrochanteric fracture (AO2-3) of the right proximal femur. (E) Postoperative radiograph showing proximal femoral nail antirotation 2 fixation of the intertrochanteric fracture. (F) At the last follow-up, union was achieved.

(A) Intraoperative fluoroscopy of a 78-year-old female patient showing an anatomical reduction of an intertrochanteric fracture (AO1-2) of the right proximal femur before insertion of a helical blade. (B) Fluoroscopy showing an intraoperative lateral wall fracture (black arrow) during insertion of a helical blade.

Preoperative Demographic Data of Patients
Postoperative Outcome after Surgery
Complications after Surgery
Figure & Data
REFERENCES
Citations

- Unstable Intertrochanteric Fracture: Do We Know Everything? A Review
Balaji Zacharia, Harshitha Hayavadana Udupa
SN Comprehensive Clinical Medicine.2022;[Epub] CrossRef

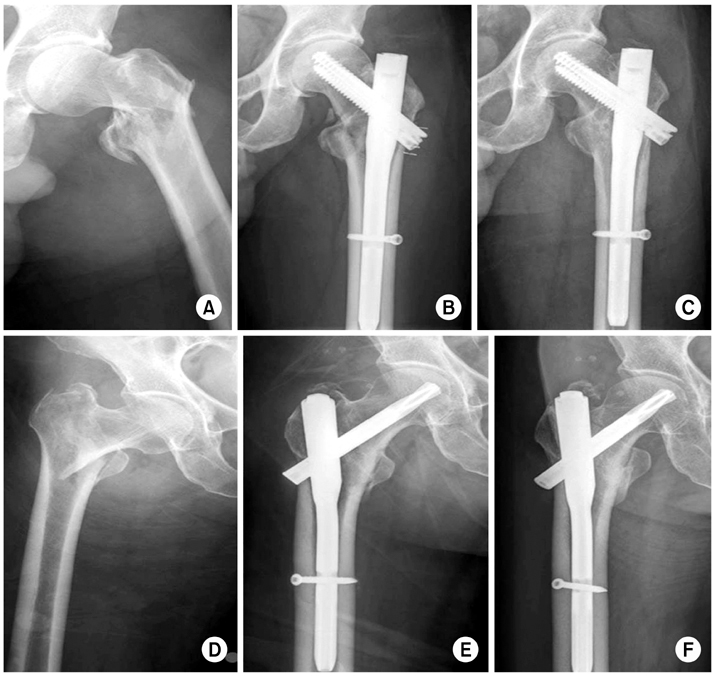
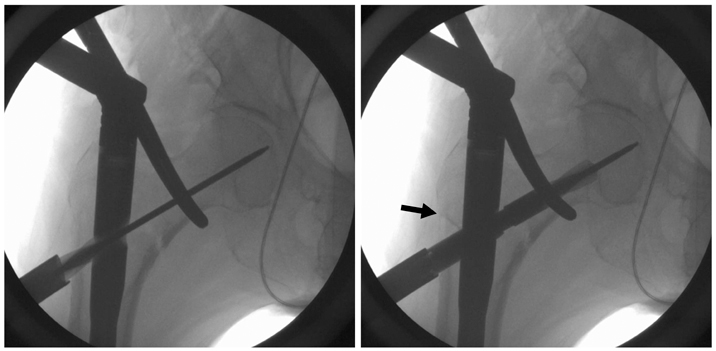
Fig. 1
Fig. 2
Fig. 3
Preoperative Demographic Data of Patients
| Characteristic | Group 1* | Group 2† | p-value |
|---|---|---|---|
| Total patients | 72 | 92 | |
| Age at surgery (yr) | 74.3±9.0 (65-95) | 74.5±9.6 (65-96) | 0.897 |
| Gender (male) | 25 (34.7) | 29 (31.5) | 0.738 |
| Affected hip (right) | 32 (44.4) | 42 (45.7) | 1.000 |
| Anesthesia (general) | 33 (45.8) | 43 (46.7) | 1.000 |
| Follow-up (mo) | 11.0±4.8 (6-36) | 12.1±7.2 (6-36) | 0.256 |
| AO type | 0.214 | ||
| A11, 12, 13 | 25 (34.7) | 37 (40.2) | |
| A21, 22, 23 | 37 (51.4) | 49 (53.3) | |
| A31, 32, 33 | 10 (13.9) | 6 (6.5) | |
| ASA | 0.915 | ||
| Class 1 | 18 (25.0) | 21 (22.8) | |
| Class 2 | 32 (44.4) | 43 (46.7) | |
| Class 3 | 22 (30.6) | 28 (30.4) | |
| Class 4 | 0 (0) | 0 (0) | |
| Mobility score before injury | 6.1±1.9 (1-9) | 6.2±1.9 (1-9) | 0.742 |
Values are presented as number only, mean±standard deviation (range), or number (%). *A group underwent InterTAN nail. †A group underwent proximal femoral nail antirotation 2. ASA: American Society of Anesthesiologists.
Postoperative Outcome after Surgery
| Variable | Group 1* (n=72) | Group 2† (n=92) | p-value |
|---|---|---|---|
| Operative time (min) | 56.2±14.4 (50-120) | 54.3±13.7 (50-120) | 0.388 |
| Blood loss (ml) | 263.9±161.7 (50-700) | 283.2±189.7 (50-700) | 0.493 |
| Postoperative drainage | 120.1 (30-550) | 110.3 (50-300) | 0.078 |
| Postoperative reduction | |||
| Anatomical | 50 (69.4) | 62 (67.4) | 0.234 |
| Acceptable | 20 (27.8) | 30 (32.6) | |
| Poor | 2 (2.8) | 0 (0) | |
| Implant position | |||
| Optimal | 60 (83.3) | 81 (88.0) | 0.498 |
| Suboptimal | 12 (16.7) | 11 (12.0) | |
| TAD (mm) | 21.7±3.3 (15-30) | 20.7±2.3 (15-30) | 0.020 |
| TAD >25 mm | 13 (18.1) | 5 (5.4) | 0.012 |
| Sliding of proximal femur (mm) | 4.1±2.3 (1.0-12.6) | 6.4±4.0 (1.2-20.2) | <0.001 |
| Bony union | 71 (98.6) | 91 (98.9) | >0.999 |
| Time to union (mo) | 5.0±2.01 (3-12) | 5.3±2.1 (3-12) | 0.379 |
Values are presented as mean±standard deviation (range), median (range), or number (%). *A group underwent InterTAN nail. †A group underwent proximal femoral nail antirotation 2. TAD: Tip apex distance.
Complications after Surgery
| Complication | Group 1* (n=72) | Group 2† (n=92) | p-value |
|---|---|---|---|
| Intraoperative complication | |||
| Lateral wall fracture | 2 (2.8) | 13 (14.1) | 0.014 |
| Fish-mouth opening | 4 (5.6) | 5 (5.4) | >0.999 |
| Postoperative complication | |||
| Hematoma formation | 2 (2.8) | 1 (1.1) | 0.582 |
| Superficial infection | 2 (2.8) | 2 (2.2) | >0.999 |
| Excessive lateral protrusion | 2 (2.8) | 11 (12.0) | 0.040 |
| Deep infection | 1 (1.4) | 1 (1.1) | >0.999 |
| General complication | |||
| Pneumonia | 8 (11.1) | 11 (12.0) | 0.867 |
| Myocardial infarction | 1 (1.4) | 0 (0) | 0.439 |
| Cerebral infarction | 1 (1.4) | 1 (1.1) | >0.999 |
| Pulmonary embolism | 1 (1.4) | 0 (0) | 0.439 |
| Deep vein thrombosis | 5 (6.9) | 10 (10.9) | 0.428 |
| Severe hemoptysis | 1 (1.4) | 0 (0) | 0.439 |
| Ulcer bleeding | 1 (1.4) | 0 (0) | 0.439 |
Values are presented as number (%). *A group underwent InterTAN nail. †A group underwent proximal femoral nail antirotation 2.
Functional Outcome at Last Follow-Up
| Variable | Group 1* (n=72) | Group 2† (n=92) | p-value |
|---|---|---|---|
| Harris hip score | 72.1±11.4 (38-96) | 70.2±9.9 (40-95) | 0.263 |
| Mobility score | 4.4±1.4 (1-8) | 4.5±1.4 (2-7) | 0.504 |
| Change in mobility score‡ | 1.5±1.0 (0-3) | 1.4±0.9 (0-5) | 0.359 |
Values are presented as mean±standard deviation (range). *A group underwent InterTAN nail. †A group underwent proximal femoral nail antirotation 2. ‡Mobility score before injury–mobility score at last follow-up.
Values are presented as number only, mean±standard deviation (range), or number (%). *A group underwent InterTAN nail. †A group underwent proximal femoral nail antirotation 2. ASA: American Society of Anesthesiologists.
Values are presented as mean±standard deviation (range), median (range), or number (%). *A group underwent InterTAN nail. †A group underwent proximal femoral nail antirotation 2. TAD: Tip apex distance.
Values are presented as number (%). *A group underwent InterTAN nail. †A group underwent proximal femoral nail antirotation 2.
Values are presented as mean±standard deviation (range). *A group underwent InterTAN nail. †A group underwent proximal femoral nail antirotation 2. ‡Mobility score before injury–mobility score at last follow-up.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

