Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 24(2); 2011 > Article
-
Review Article
- Thoracic Spine Fractures
- Young-Woo Kim, M.D., Ph.D., Young-Seok Kim, M.D., Jae-Chel Byun, M.D., Yong-Bok Park, M.D.
-
Journal of the Korean Fracture Society 2011;24(2):195-205.
DOI: https://doi.org/10.12671/jkfs.2011.24.2.195
Published online: April 13, 2011
Department of Orthopaedic Surgery, Hangang Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea.
- Address reprint requests to: Young-Woo Kim, M.D., Ph.D. Department of Orthopaedic Surgery, Hangang Sacred Heart Hospital, College of Medicine, Hallym University, Yeongdeungpo-dong 7-ga, Yeongdeungpo-gu, Seoul 150-719, Korea. Tel: 82-2-2639-5650, Fax: 82-2-2639-5654, ywkimmd@hallym.ac.kr
Copyright © 2011 The Korean Fracture Society
- 1,170 Views
- 12 Download
- 1 Crossref
- 1. Andriacchi T, Schultz A, Belytschko T, Galante J. A model for studies of mechanical interactions between the human spine and rib cage. J Biomech, 1974;7:497-507.Article
- 2. Bohlman HH, Kirkpatrick JS, Delamarter RB, Leventhal M. Anterior decompression for late pain and paralysis after fractures of the thoracolumbar spine. Clin Orthop Relat Res, 1994;300:24-29.Article
- 3. Bradford DS, McBride GG. Surgical management of thoracolumbar spine fractures with incomplete neurologic deficits. Clin Orthop Relat Res, 1987;218:201-216.Article
- 4. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976), 1983;8:817-831.Article
- 5. Denis F, Burkus JK. Shear fracture-dislocations of the thoracic and lumbar spine associated with forceful hyperextension (lumberjack paraplegia). Spine (Phila Pa 1976), 1992;17:156-161.Article
- 6. Ferguson RL, Allen BL Jr. A mechanistic classification of thoracolumbar spine fractures. Clin Orthop Relat Res, 1984;189:77-88.Article
- 7. Geisler FH, Dorsey FC, Coleman WP. Recovery of motor function after spinal-cord injury--a randomized, placebo-controlled trial with GM-1 ganglioside. N Engl J Med, 1991;324:1829-1838.Article
- 8. Gertzbein SD. Fractures of the thoracic and lumbar spine, 1992;Baltimore, Williams & Wilkins.
- 9. Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976), 1992;17:528-540.
- 10. McAfee PC, Yuan HA, Fredrickson BE, Lubicky JP. The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg Am, 1983;65:461-473.Article
- 11. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976), 1994;19:1741-1744.Article
- 12. Oda T, Panjabi MM, Kato Y. The effects of pedicle screw adjustments on the anatomical reduction of thoracolumbar burst fractures. Eur Spine J, 2001;10:505-511.ArticlePDF
- 13. Reid DC, Hu R, Davis LA. Floman Y, Farcy JP, Argenson C. The nonsurgical treatment of burst fractures. In: Thoracolumbar spine fractures, 1993;New York, Raven. 215-222.
- 14. Saboe LA, Reid DC, Davis LA, Warren SA, Grace MG. Spine trauma and associated injuries. J Trauma, 1991;31:43-48.Article
- 15. Singh K, Kim D, Vaccaro AR. Herkowitz HN, Garfin SR, Eismont FJ, Bell GR, Balderston RA. Thoracic and lumbar spinal injuries. In: The spine, 2006;5th ed. Philadelphia, Saunders. 1132-1156.
- 16. Vaccaro AR. Combined anterior and posterior surgery for fractures of the thoracolumbar spine. Instr Course Lect, 1999;48:443-449.
- 17. Verlaan JJ, van Helden WH, Oner FC, Verbout AJ, Dhert WJ. Balloon vertebroplasty with calcium phosphate cement augmentation for direct restoration of traumatic thoracolumbar vertebral fractures. Spine (Phila Pa 1976), 2002;27:543-548.Article
- 18. White AA, Panjabi MM. Clinical Biomechanics of the Spine, 1978;Philadelphia, JB Lippincott.
REFERENCES
Fig. 1Schematic drawing of a transverse section of the spinal cord at the thoracic level, showing the anatomic organization of the corticospinal tract and posterior column (L: lumbar, S: sacral, T: thoracic).
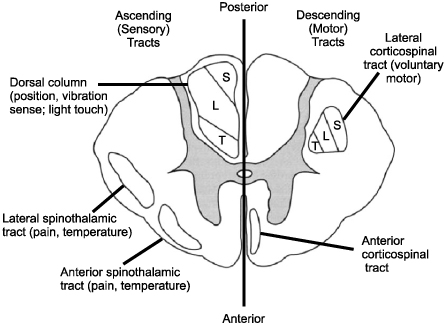
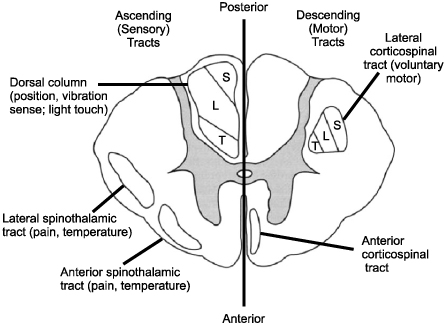
Fig. 2
Types of spinal cord injury (shaded zones) that produce the four main incomplete injury patterns seen clinically.
(A) Central cord syndrome.
(B) Anterior cord syndrome.
(C) Brown-Sequard syndrome.
(D) Posterior cord syndrome.
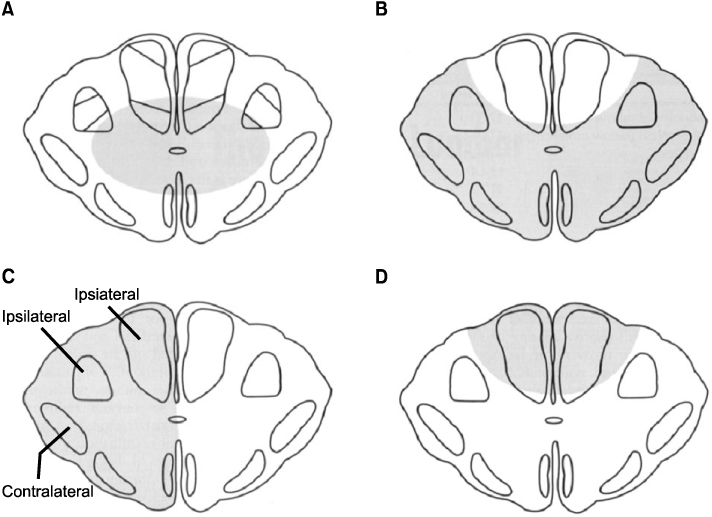
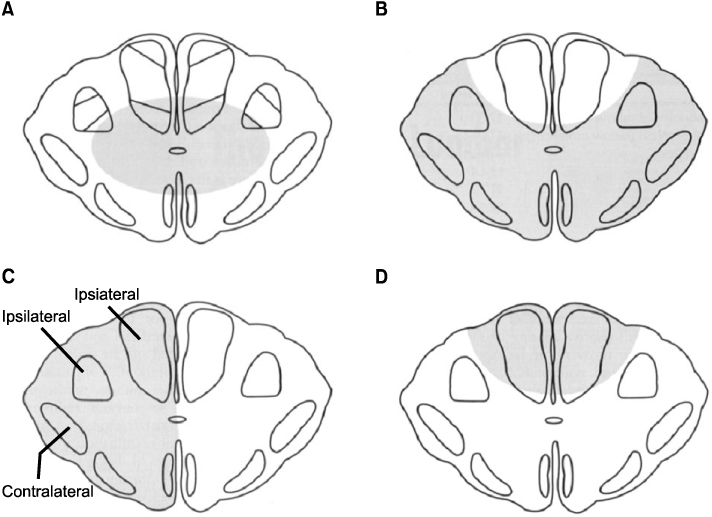
Fig. 3Denis three-column model of spinal stability which involves anterior (anterior 1/2 of vertebra/disc and anterior longitudinal ligament), middle (posterior 1/2 of vertebra/disc and posterior longitudinal ligament), and posterior (posterior elements including the pedicles and facet joints and the remaining ligaments) columns. According to this paradigm, any injury extending into the middle column is largely considered to be unstable.
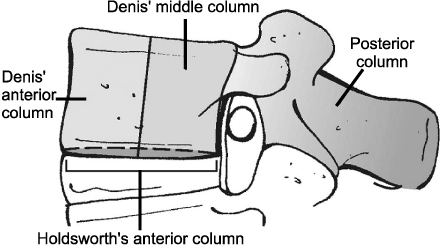
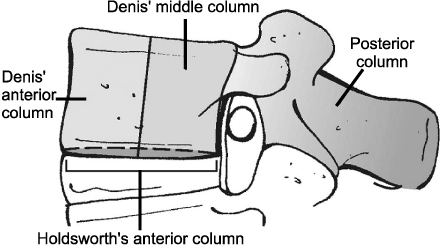
Fig. 4Denis classification of thoracolumbar compression injuries. These fractures may involve both endplates (A, type A), the superior endplate only (B, type B), the inferior endplate only (C, type C), or a buckling of the anterior cortex with both endplates intact (D, type D).
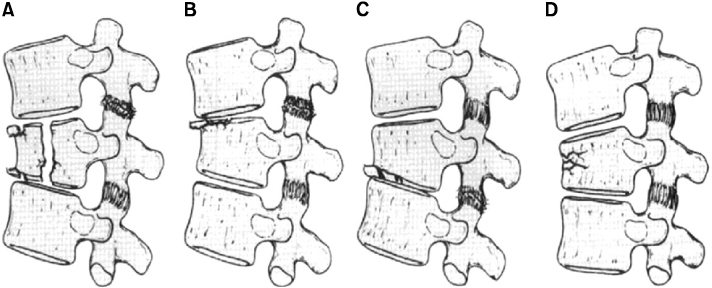
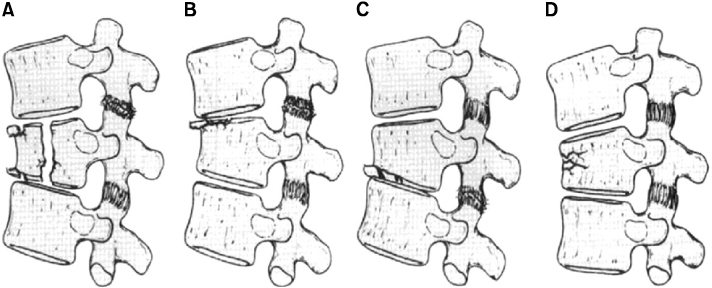
Fig. 5
Denis classification of thoracolumbar burst fractures.
(A~C) Types A, B, and C represent fractures of both endplates, the superior endplate, and the inferior endplate, respectively.
(D) Type D is a combination of a type A burst fracture with rotation, which is best appreciated on an anteroposterior radiograph. The superior or inferior endplate, or both, may be involved with this fracture.
(E) Type E is eccentrically loaded type A fracture.
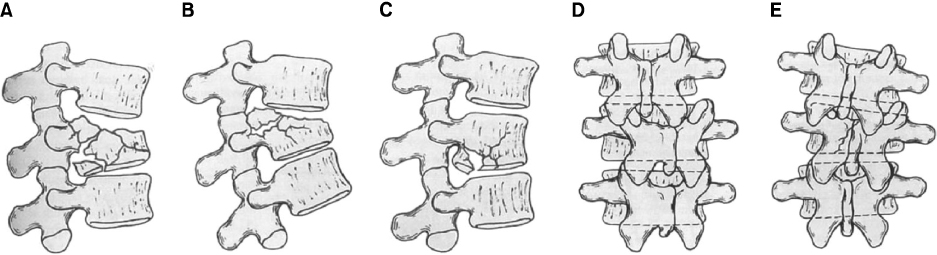
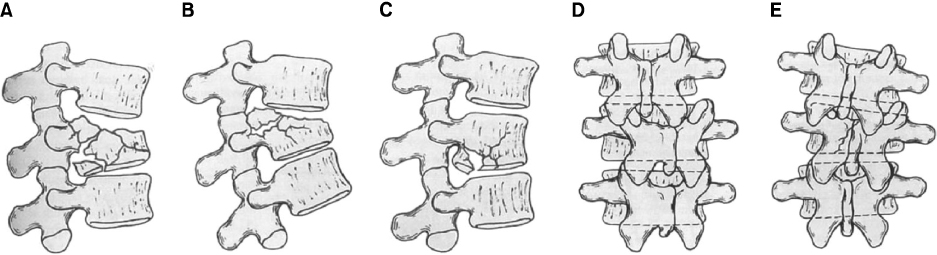
Fig. 6Denis classification of flexion-distraction injuries. These may occur at one level through the bone (A), at one level through the ligaments and disc (B), at two levels, with the middle column injured through the bone (C), or at two levels with the middle column injured through the ligament and disc (D).
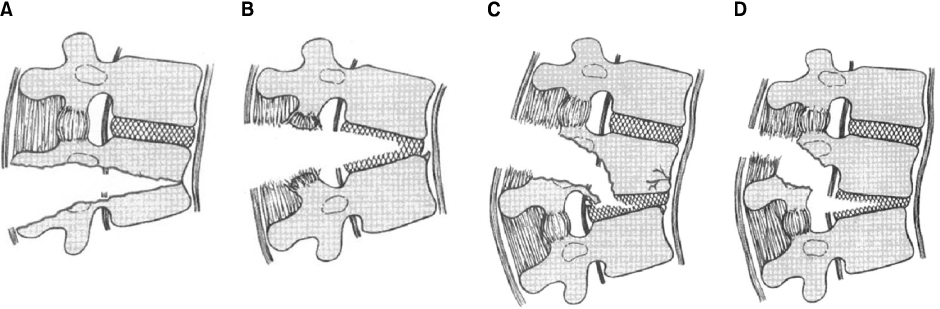
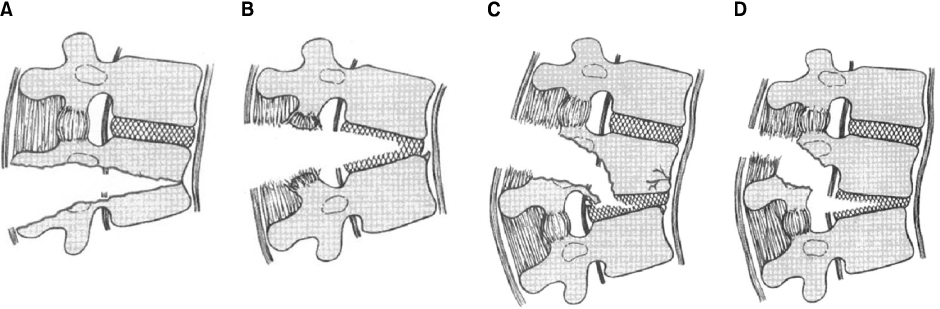
Fig. 7Denis classification of fracture-dislocations. These may occur at one level through the bone (A), at one level through the ligaments and disc (B), or at two levels, with the middle column injuried through the bone or at two levels with the middle column injuried through the ligament and disc (C).


Fig. 8The load sharing classification system for thoracolumbar fractures identifies injuries that may be appropriately treated with short-segment posterior instrumentation constructs by assigning points based on the extent of vertebral body comminution, apposition of the body fragments, and the degree of focal kyphosis.
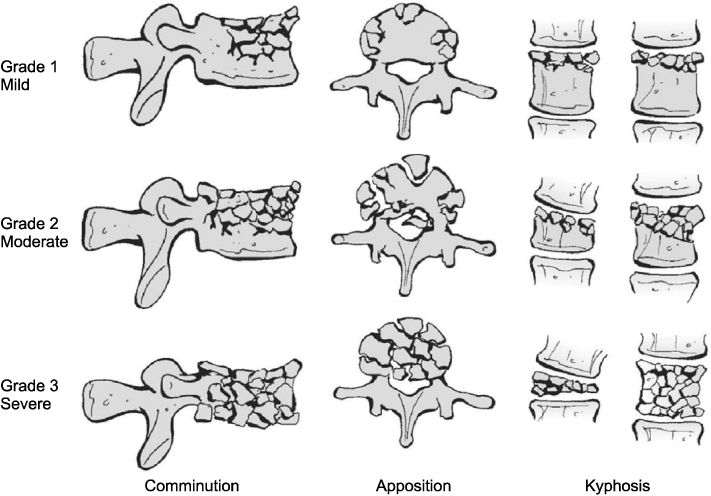
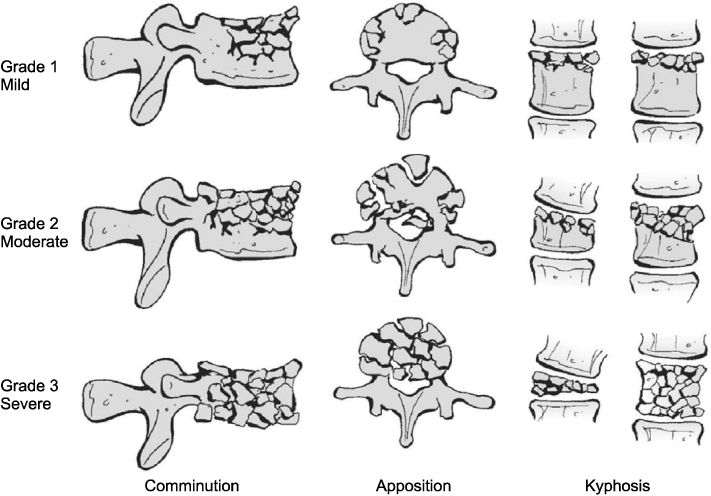
Fig. 9
A 36-year old man got injured by a fall from height, who was diagnosed with complete paraplegia due to the cord injury with unstable bursting fracture at T12 and L1 (A, B).
The preoperative MRI (C), and CT (D) showed the cord compressed by the retropulsed bony fragments. He underwent indirect reduction by ligamentotaxis using segmental pedicle screw instrumentation from T11 to L2 with distraction (E, F).
Postoperative CT (G) and MRI (H) shows the cord decompressed after the operation, but the patient has not recovered from the complete paraplegia.
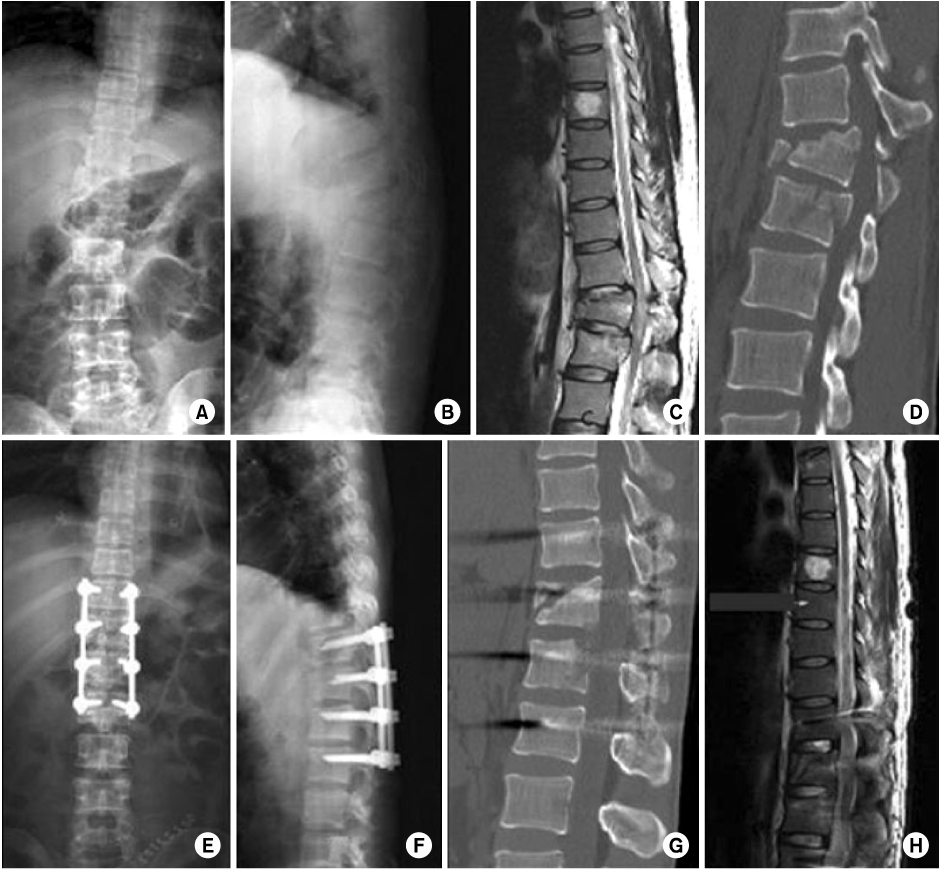
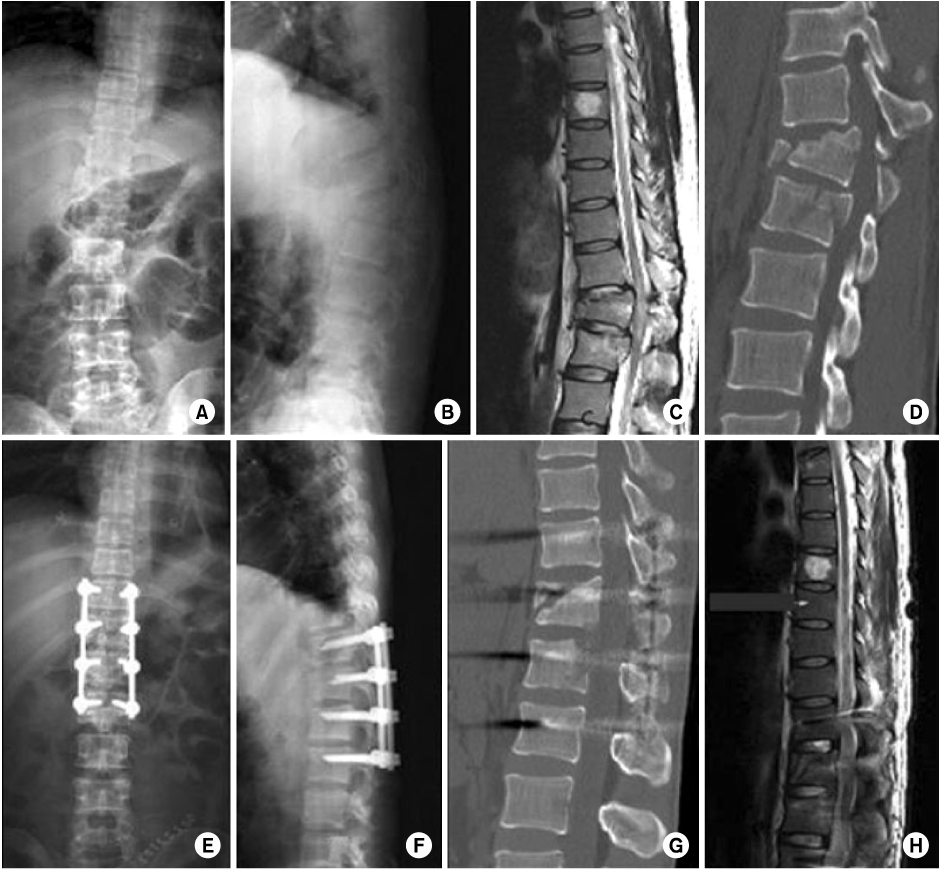
Fig. 10
A 53-year old lady was operated on her back to fix the T12 bursting fracture at other hospital. When she visited our spine center 15 months later from the initial operation, she complained of severe back pain and numbness on her both lower extremities with thoracolumbar kyphosis. She couldn't lie flat on her back due to aggravating back pain and leg numbness. Preoperative x-ray showed thoracolumbar kyphosis and pull out of both L1 pedicle screws (A~C).
In the CT and MRI findings, the spinal cord compressed slightly by the sharp margin of T12 body (D, E).
The spinal cord decompressed by modified PSO and the spinal column realigned normally (F~H).
At 5 months postoperatively, the operation site was fused solidly without loss of correction (I, J).
And the leg symptoms were resolved completely.
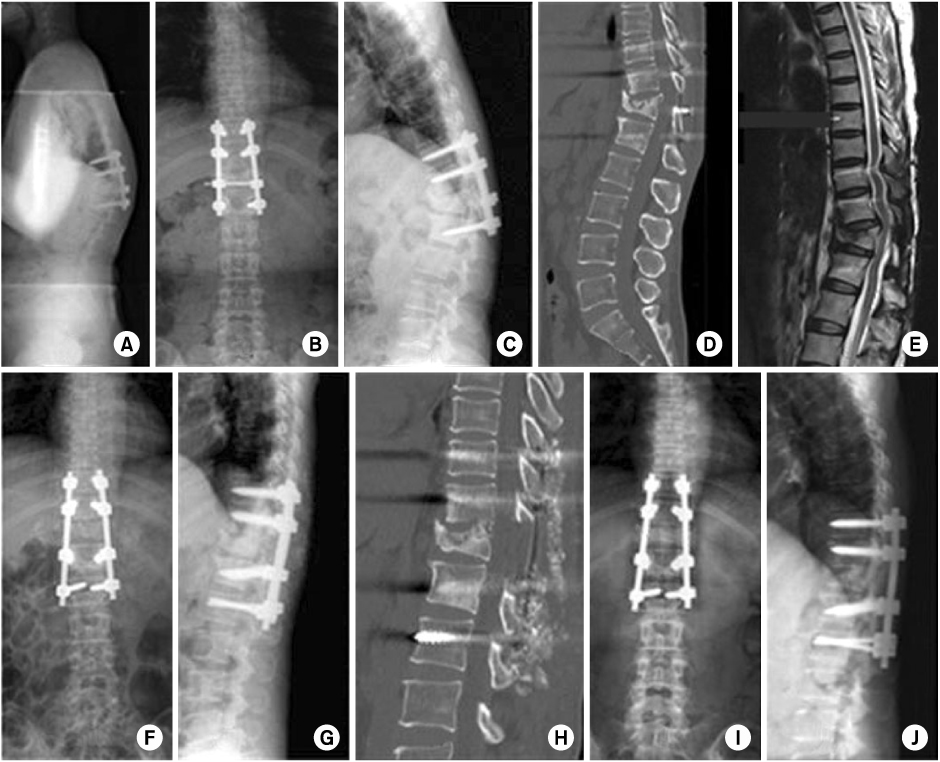
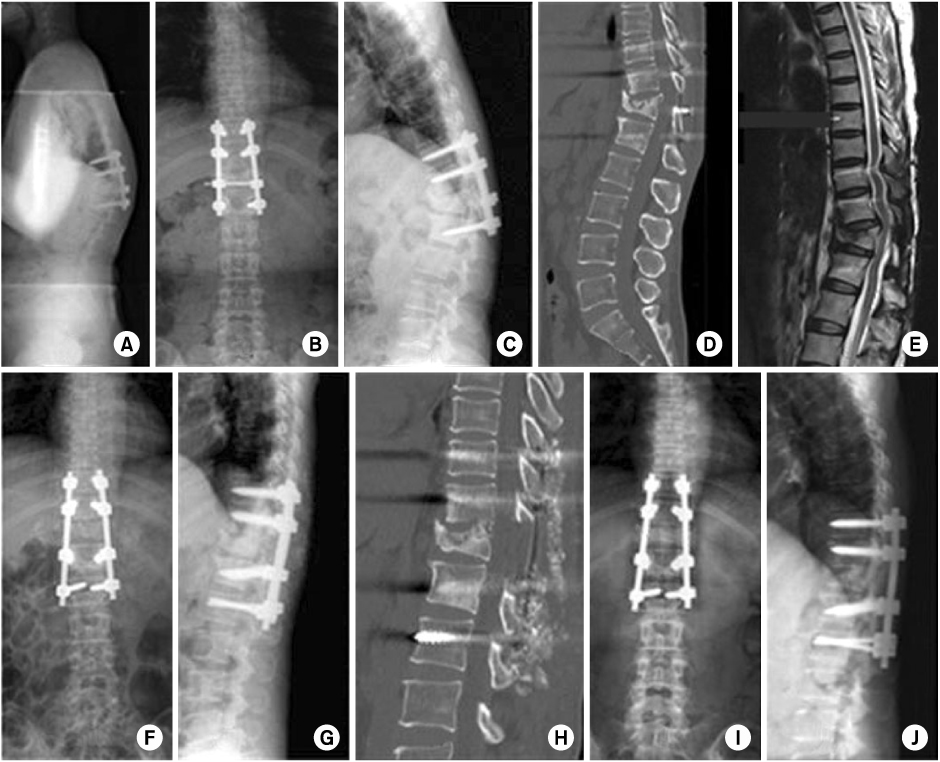
Fig. 11
A 68-year old man sustained a bony chance fracture at T12 by a fall (A, B).
Preoperative CT showed clear fracture line at the T12 body and lamina (C).
The fracture was reduced by cantilever method using USS universal spine system (D, E).
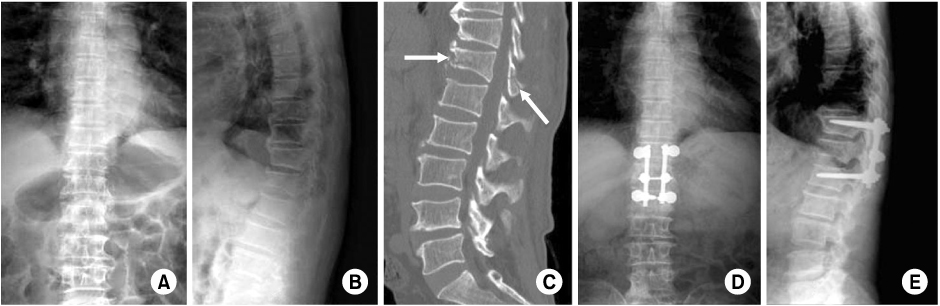
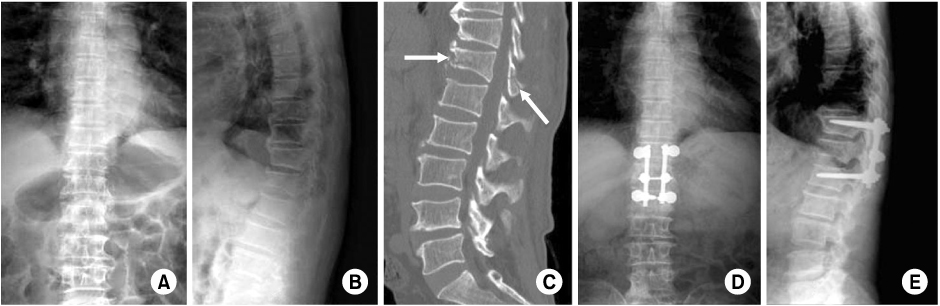
Fig. 12
A flexion-distraction type injury at T12 and L1 and compression fracture of L4 which involving both end plates by a fall from height. The 28-year old man got 60% flame burn on his both lower extremities and the trunk. The spinal operation was delayed for 4 and half months to care the burn wound. The preoperative x-ray shows kyphosis at the thoracolumbar junction with wedging of L1 body (A, B).
Preoperative parasagittal CT shows bilateral facet dislocation of T12 and L1 (C, E).
The patient complained paraparesis at both lower extremities and the CT shows the dislodged posterosuperior coner of L1 body was compressing the spinal cord (D).
The spinal cord decompressed by modified pedicle subtraction osteotomy at L1, and the spinal alignment normalized very nicely. The patient's neurologic symptoms were subsided after the operation (F~H).
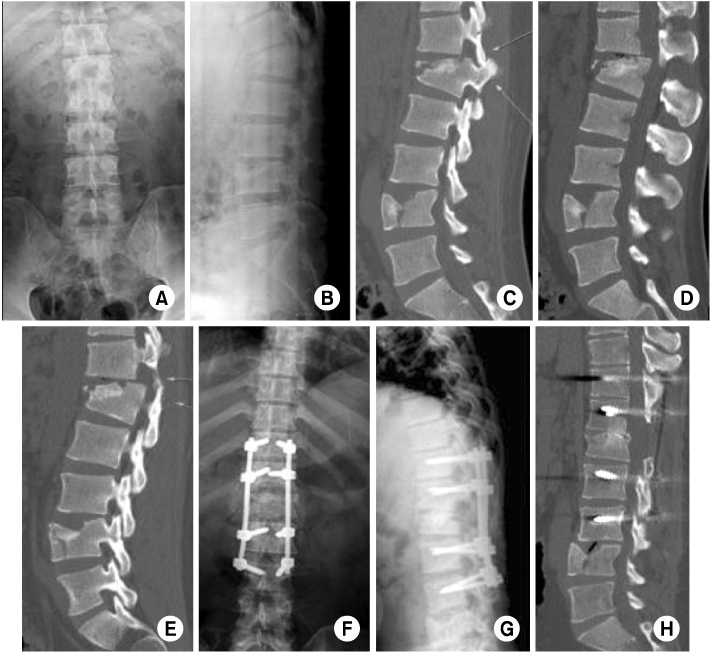
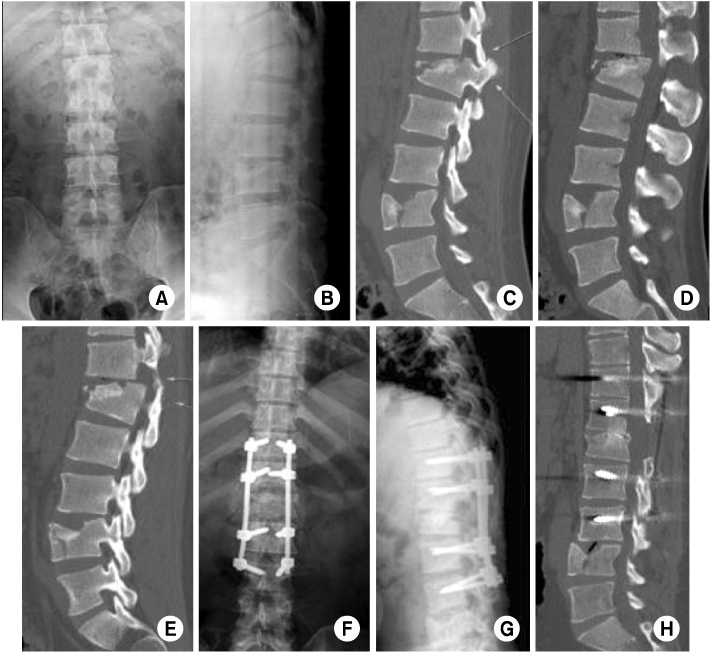
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Unusual midsagittal defects in vertebrae from McKee Island, Alabama (1Ms32)
Brian D. Padgett, Alexis Dzubak
International Journal of Paleopathology.2014; 6: 44. CrossRef
Thoracic Spine Fractures
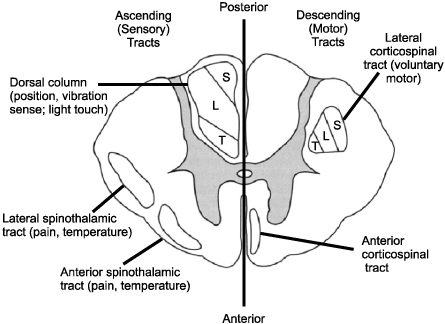
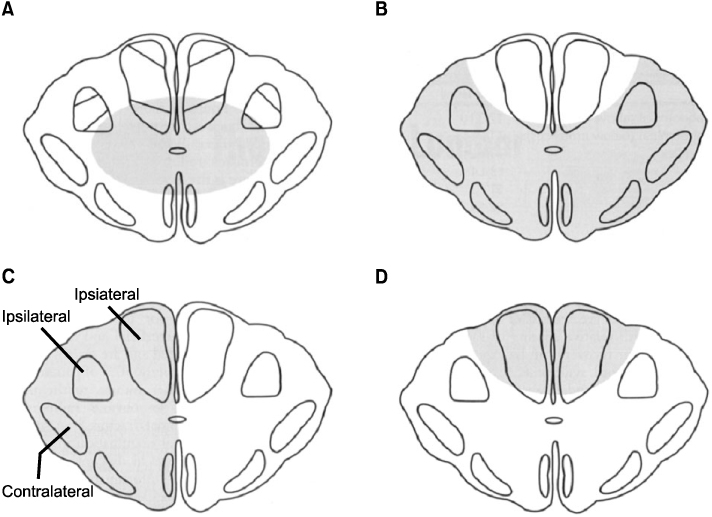
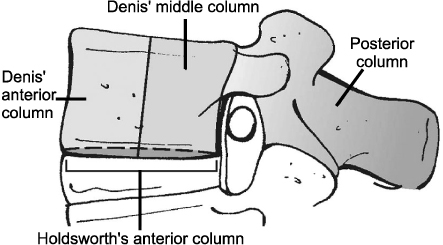

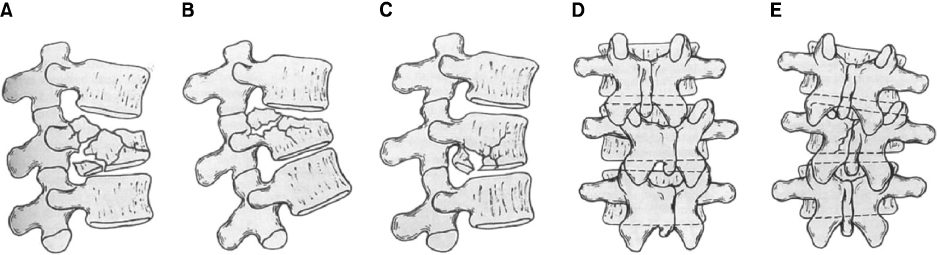
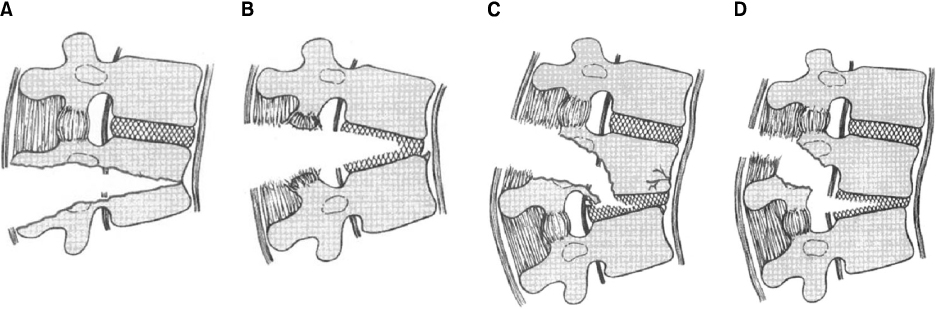
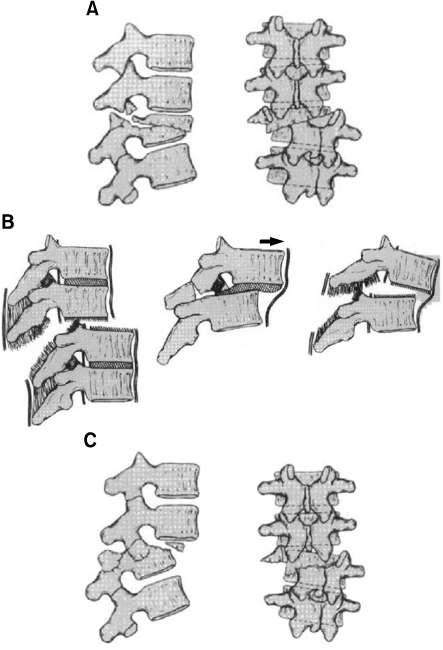
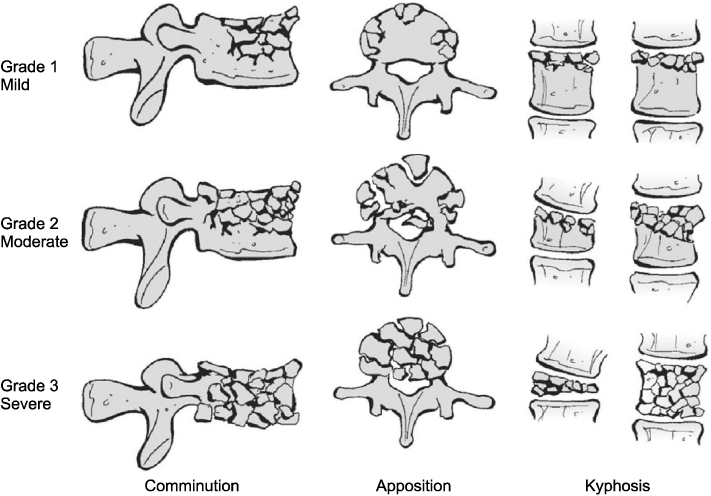
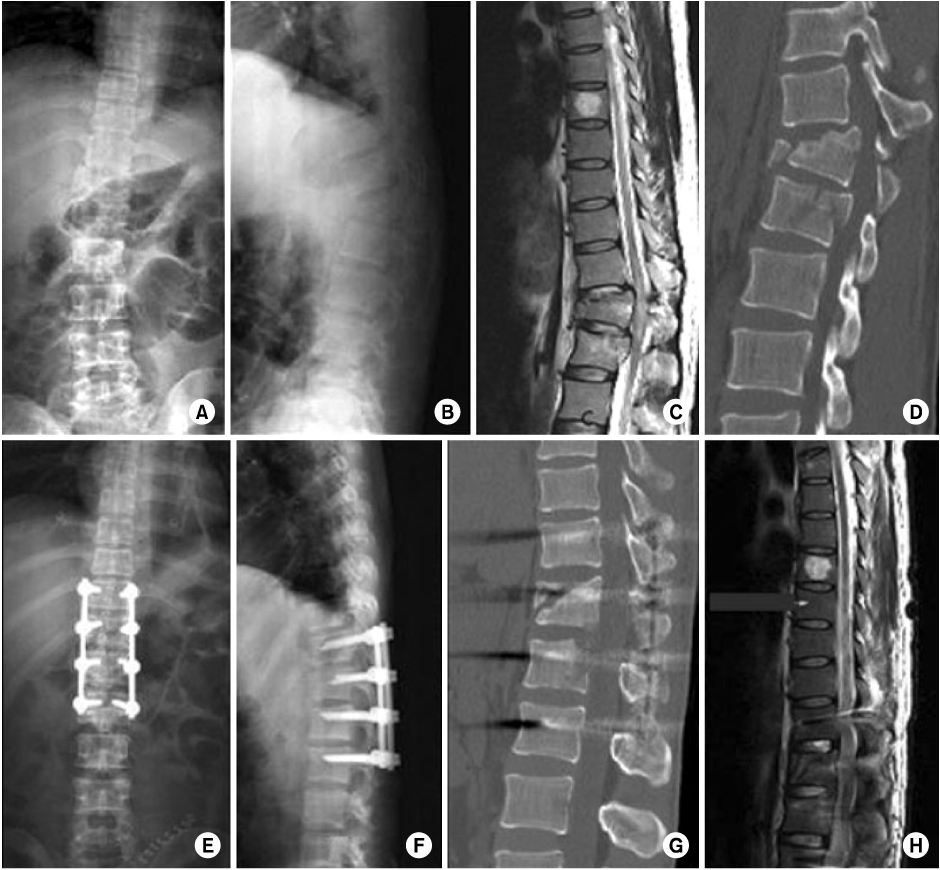
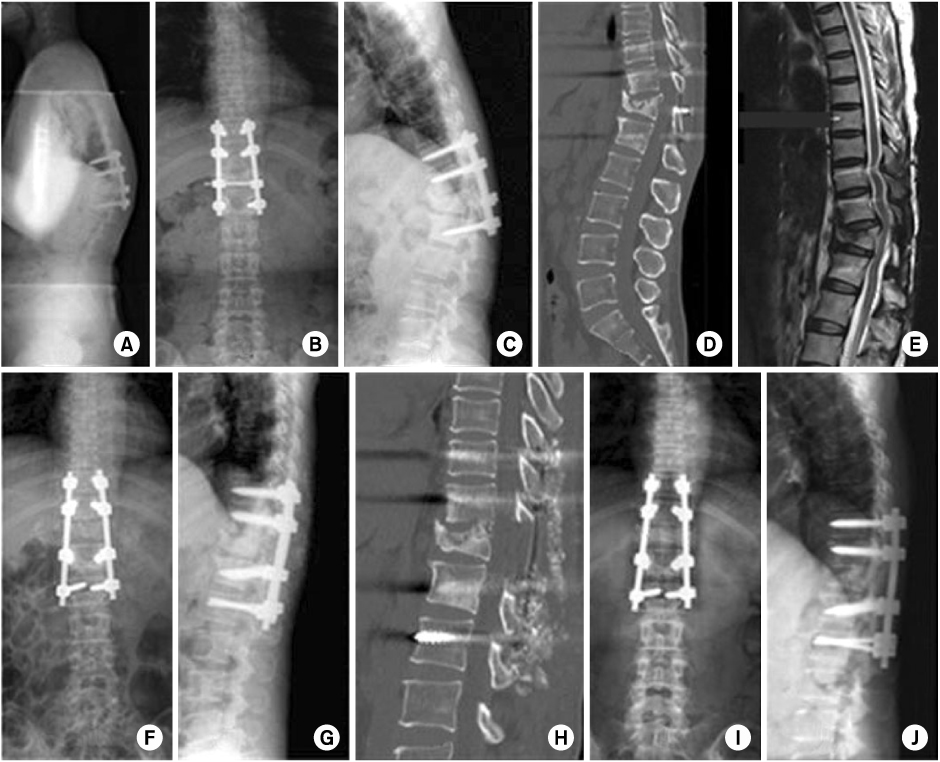
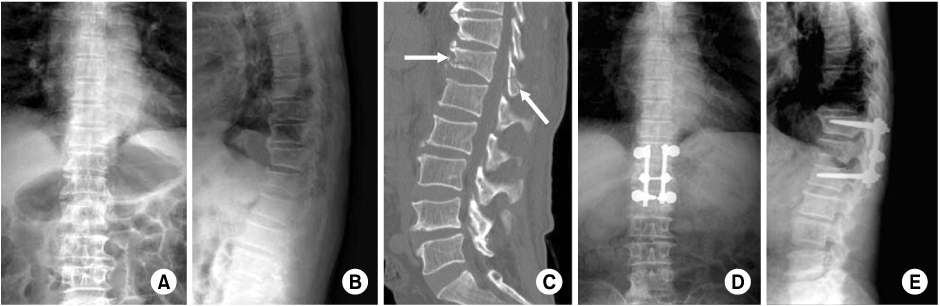
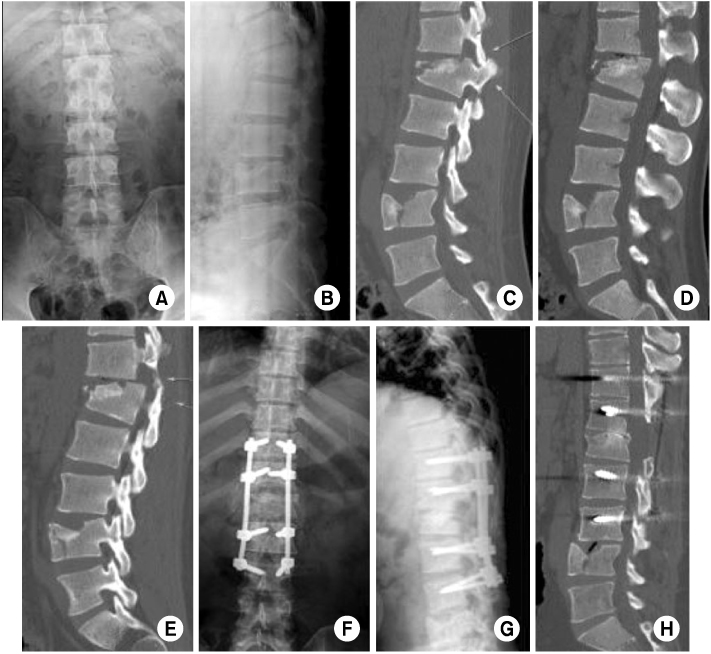
Fig. 1
Schematic drawing of a transverse section of the spinal cord at the thoracic level, showing the anatomic organization of the corticospinal tract and posterior column (L: lumbar, S: sacral, T: thoracic).
Fig. 2
Types of spinal cord injury (shaded zones) that produce the four main incomplete injury patterns seen clinically.
(A) Central cord syndrome.
(B) Anterior cord syndrome.
(C) Brown-Sequard syndrome.
(D) Posterior cord syndrome.
Fig. 3
Denis three-column model of spinal stability which involves anterior (anterior 1/2 of vertebra/disc and anterior longitudinal ligament), middle (posterior 1/2 of vertebra/disc and posterior longitudinal ligament), and posterior (posterior elements including the pedicles and facet joints and the remaining ligaments) columns. According to this paradigm, any injury extending into the middle column is largely considered to be unstable.
Fig. 4
Denis classification of thoracolumbar compression injuries. These fractures may involve both endplates (A, type A), the superior endplate only (B, type B), the inferior endplate only (C, type C), or a buckling of the anterior cortex with both endplates intact (D, type D).
Fig. 5
Denis classification of thoracolumbar burst fractures.
(A~C) Types A, B, and C represent fractures of both endplates, the superior endplate, and the inferior endplate, respectively.
(D) Type D is a combination of a type A burst fracture with rotation, which is best appreciated on an anteroposterior radiograph. The superior or inferior endplate, or both, may be involved with this fracture.
(E) Type E is eccentrically loaded type A fracture.
Fig. 6
Denis classification of flexion-distraction injuries. These may occur at one level through the bone (A), at one level through the ligaments and disc (B), at two levels, with the middle column injured through the bone (C), or at two levels with the middle column injured through the ligament and disc (D).
Fig. 7
Denis classification of fracture-dislocations. These may occur at one level through the bone (A), at one level through the ligaments and disc (B), or at two levels, with the middle column injuried through the bone or at two levels with the middle column injuried through the ligament and disc (C).
Fig. 8
The load sharing classification system for thoracolumbar fractures identifies injuries that may be appropriately treated with short-segment posterior instrumentation constructs by assigning points based on the extent of vertebral body comminution, apposition of the body fragments, and the degree of focal kyphosis.
Fig. 9
A 36-year old man got injured by a fall from height, who was diagnosed with complete paraplegia due to the cord injury with unstable bursting fracture at T12 and L1 (A, B).
The preoperative MRI (C), and CT (D) showed the cord compressed by the retropulsed bony fragments. He underwent indirect reduction by ligamentotaxis using segmental pedicle screw instrumentation from T11 to L2 with distraction (E, F).
Postoperative CT (G) and MRI (H) shows the cord decompressed after the operation, but the patient has not recovered from the complete paraplegia.
Fig. 10
A 53-year old lady was operated on her back to fix the T12 bursting fracture at other hospital. When she visited our spine center 15 months later from the initial operation, she complained of severe back pain and numbness on her both lower extremities with thoracolumbar kyphosis. She couldn't lie flat on her back due to aggravating back pain and leg numbness. Preoperative x-ray showed thoracolumbar kyphosis and pull out of both L1 pedicle screws (A~C).
In the CT and MRI findings, the spinal cord compressed slightly by the sharp margin of T12 body (D, E).
The spinal cord decompressed by modified PSO and the spinal column realigned normally (F~H).
At 5 months postoperatively, the operation site was fused solidly without loss of correction (I, J).
And the leg symptoms were resolved completely.
Fig. 11
A 68-year old man sustained a bony chance fracture at T12 by a fall (A, B).
Preoperative CT showed clear fracture line at the T12 body and lamina (C).
The fracture was reduced by cantilever method using USS universal spine system (D, E).
Fig. 12
A flexion-distraction type injury at T12 and L1 and compression fracture of L4 which involving both end plates by a fall from height. The 28-year old man got 60% flame burn on his both lower extremities and the trunk. The spinal operation was delayed for 4 and half months to care the burn wound. The preoperative x-ray shows kyphosis at the thoracolumbar junction with wedging of L1 body (A, B).
Preoperative parasagittal CT shows bilateral facet dislocation of T12 and L1 (C, E).
The patient complained paraparesis at both lower extremities and the CT shows the dislodged posterosuperior coner of L1 body was compressing the spinal cord (D).
The spinal cord decompressed by modified pedicle subtraction osteotomy at L1, and the spinal alignment normalized very nicely. The patient's neurologic symptoms were subsided after the operation (F~H).
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
Fig. 9
Fig. 10
Fig. 11
Fig. 12
Thoracic Spine Fractures
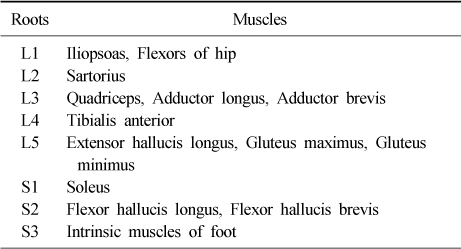
Nerve innervation of leg muscles
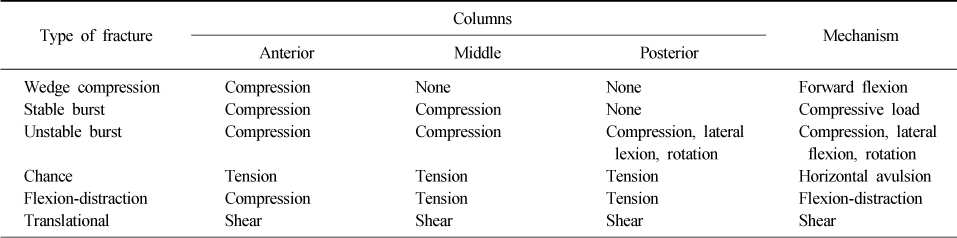
The McAfee classification system
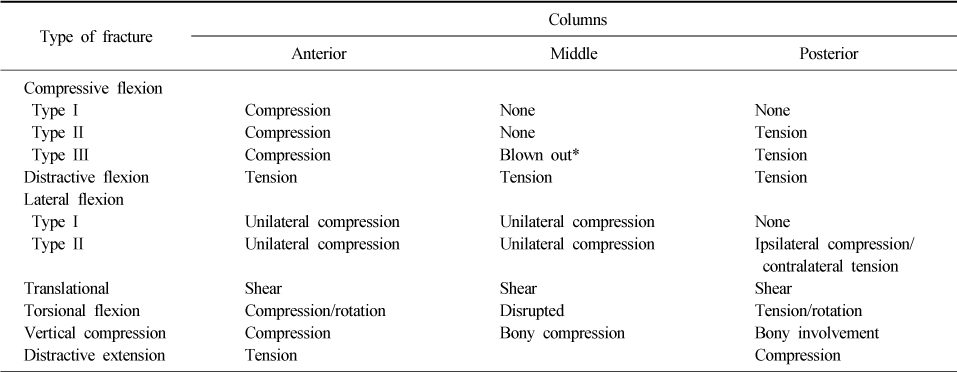
The Ferguson and Allen classification system for spinal fractures
*Blown out: Evidence of middle column bone rotated into the neural canal between pedicles.
Table 1
Nerve innervation of leg muscles
Table 2
The McAfee classification system
Table 3
The Ferguson and Allen classification system for spinal fractures
*Blown out: Evidence of middle column bone rotated into the neural canal between pedicles.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

