Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 20(2); 2007 > Article
-
Review Article
- Treatment of Infected Nonunion
- Sang-Ho Ha, M.D.
-
Journal of the Korean Fracture Society 2007;20(2):206-214.
DOI: https://doi.org/10.12671/jkfs.2007.20.2.206
Published online: June 14, 2016
Department of Orthopedic Surgery, Chosun University Hospital, 588, Seosuk-dong, Dong-gu, Gwangju 501-717, Korea.
- Address reprint requests to: Sang-Ho Ha, M.D. Department of Orthopedic Surgery, Chosun University Hospital, 588, Seosuk-dong, Dong-gu, Gwangju 501-717, Korea. Tel:82-62-220-3147, Fax: 82-62-226-3379, shha@chosun.ac.kr
Copyright © The Korean Fracture Society. All rights reserved
- 614 Views
- 1 Download
- 1 Crossref
- 1. Babhulkar S, Pande K, Babhulkar S. Nonunion of the diaphysis of long bone. Clin Orthop Relat Res, 2005;431:50-56.
- 2. Brinker MR, O'Connor DP. Exchange nailing of ununited fractures. J Bone Joint Surg Am, 2007;89:177-188.Article
- 3. Browner BD, Jupiter JB, Levine AM, Trafton PG. Skeletal trauma. 3rd ed. Philadelphia: Saunders; 2003. p. 532-535.
- 4. Cabanela ME. Open cancellous bone grafting of infected bone defects. Orthop Clin North Am, 1984;15:427-440.Article
- 5. Chen CE, KO JY, Pan CC. Results of vancomycin-impregnated cancellous bone grafting for infected tibial nonunion. Arch Orthop Trauma Surg, 2005;125:369-375.ArticlePDF
- 6. Cho SH, Jeong ST, Park HB, Hwang SC, Ha YC, Hwang IH. Two-stage reconstruction of infected nonunion of long bones using antibiotics- impregnated cement beads. J Korean Fract Soc, 2004;17:395-400.Article
- 7. Green SA, Dlabal TA. The open bone graft for septic nonunion. Clin Orthop Relat Res, 1983;180:117-124.Article
- 8. Green SA, Jackson JM, Wall DM, Marinow H, Ishkanian J. Management of segmental defects by the llizarov intercalary bone transport method. Clin Orthop Relat Res, 1992;280:136-142.
- 9. Han DY, Lee HM, Lee SB. A clinical analysis of the treatment of infected non-union in the fractures of long bones. J Korean Orthop Assoc, 1990;25:389-397.ArticlePDF
- 10. Han SK, Choi NY, Park SJ, Lee SK, Jang G, Lee IJ. Antibiotic cement-coated unreamed nailing for treatment of infected nonunion of long bone. J Korean Orthop Assoc, 2000;35:699-703.ArticlePDF
- 11. Holtom PD, Patzakis MJ. Newer methods of antimicrobial delivery for bone and joint infections. Instr Course Lect, 2003;52:745-749.
- 12. Jain AK, Sinha S. Infected nonunion of the long bones. Clin Orthop Relat Res, 2005;431:57-65.Article
- 13. Klemm KW. Antibiotic bead chains. Clin Orthop Relat Res, 1993;295:63-76.Article
- 14. Krishnan A, Pamecha C, Patwa JJ. Modified llizarov technique for infected nonunion of the femur: the principle of distraction-compression osteogenesis. J Orthop Surg (Hong Kong), 2006;14:265-272.ArticlePDF
- 15. Mader JT, Landon GC, Calhoun J. Antimicrobial treatment of osteomyelitis. Clin Orthop Relat Res, 1993;295:87-95.Article
- 16. Marsh JL, Prokuski L, Biermann S. Chronic infected tibial nonunion with bone loss: conventaional techniques versus bone transport. Clin Orthop Relat Res, 1994;(301):139-146.
- 17. May JW Jr, Jupiter JB, Weiland AJ, Byrd HS. Current concepts review: clinical classification of post-traumatic tibial osteomyelitis. J Bone Joint Surg Am, 1989;71:1422-1428.
- 18. Meyer S, Weiland AJ, Willenegger H. The treatment of infected non-union of fractures of long bones. Study of sixty-four cases with a five to twenty-one-year follow-up. J Bone Joint Surg Am, 1975;57:836-842.Article
- 19. Miller ME, Ada JR, Webb LX. Treatment of infected no nunion and delayed union of tibia fractures with locking intramedullary nails. Clin Orthop Relat Res, 1989;(245):233-238.
- 20. Park MS, Lee KO. The treatment of infected non-union of fractures of long bones. J Korean Orthop Assoc, 1985;20:689-699.ArticlePDF
- 21. Park SJ, Shim JS, Shin SK. Treatment for intractable infected nonunion of lower extremity in elderly people using external fixator. J Korean Fract Soc, 2004;17:177-183.Article
- 22. Patzakis MJ, Scilaris TA, Chon J, Holtom P, Sherman R. Results of bone grafting for infected tibial nonunion. Clin Orthop Relat Res, 1995;315:192-198.Article
- 23. Ruedi TP, Murphy WM. AO principles of fracture management. 1st ed. New York: Theime; 2000. p. 785-800.
- 24. Toh CL, Jupiter JB. The infected nonunion of the tibia. Clin Orthop Relat Res, 1995;(315):176-191.
- 25. Ueng SW, Wei FC, Shin CH. Management of femoral diaphyseal infected nonunion with antibiotic beads local therapy, external skeletal fixation, and staged bone grafting. J Trauma, 1999;46:97-103.Article
- 26. Wahlig H, Dingeldein E, Bergmann R, Reuss K. The release of gentamicin from polymethylmethacrylate beads. An experimental and pharmacokinetic study. J Bone Joint Surg Br, 1978;60-B:270-275.ArticlePDF
- 27. Weiland AJ. Current concepts review: vascularized free bone transplants. J Bone Joint Surg Am, 1981;63:166-169.
REFERENCES
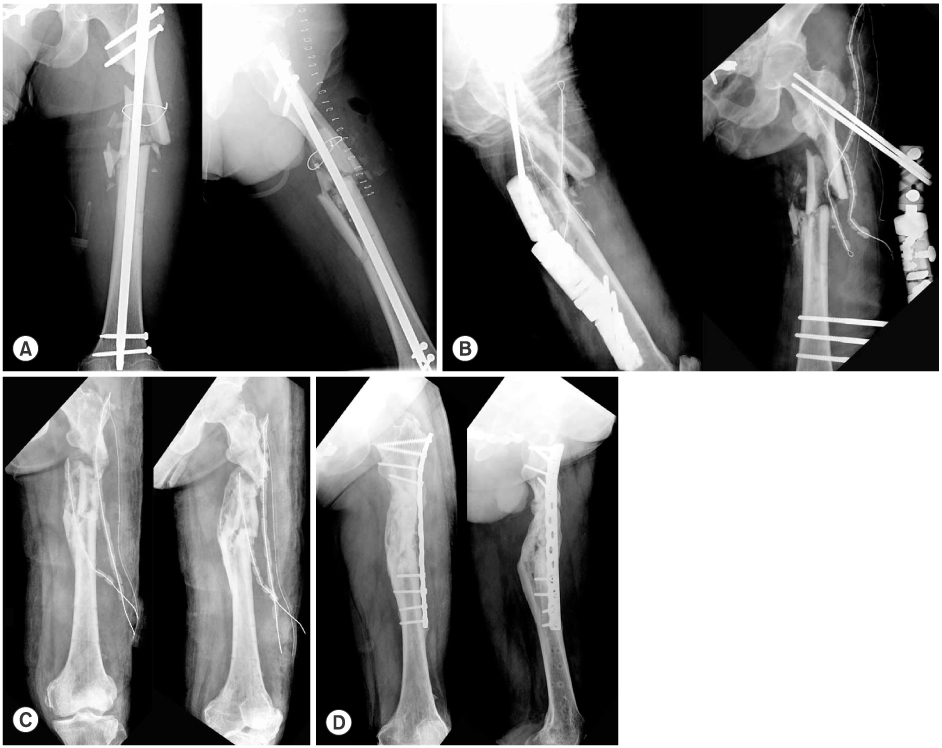
Fig. 1
(B) Implant removal and debridement of the infected nonunion site was done with stabilization using external fixator.
(C) Last follow up radiograph shows complete bone union with good alignment.
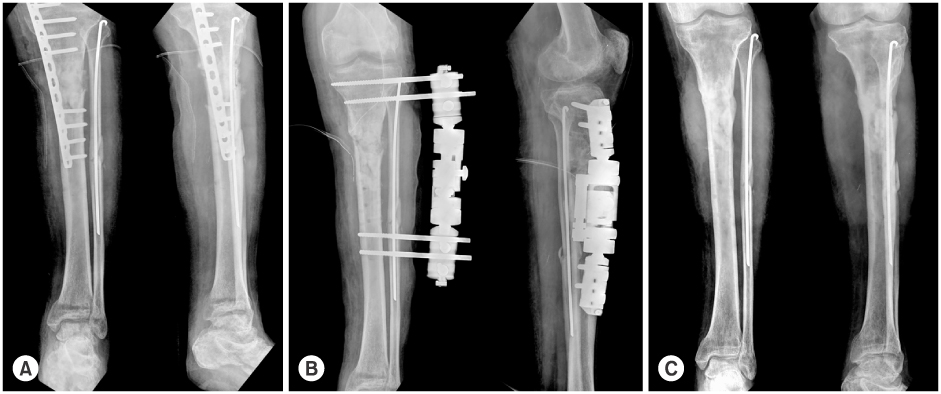
(A) The radiograph shows tibia proximal shaft fracture with LCP applied. The patient showed pus discharge from the fracture site and loosening of the implants.
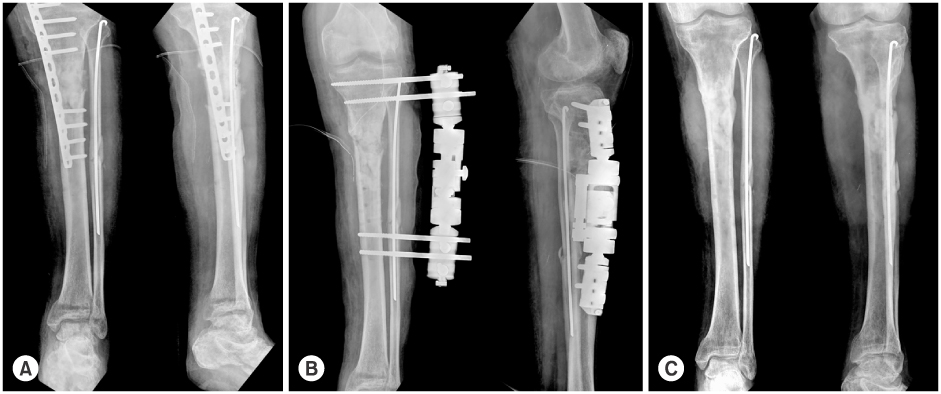
Fig. 2
(B) Sequestrectomy and debridement was done with external fixator applied.
(C) The external fixator was changed to intramedullary nail with strut bone graft. Radiograph shows partial bone union with good alignment.
(A) Debridement and antibiotic mixed cement bead insertion was done but infection was not controlled.
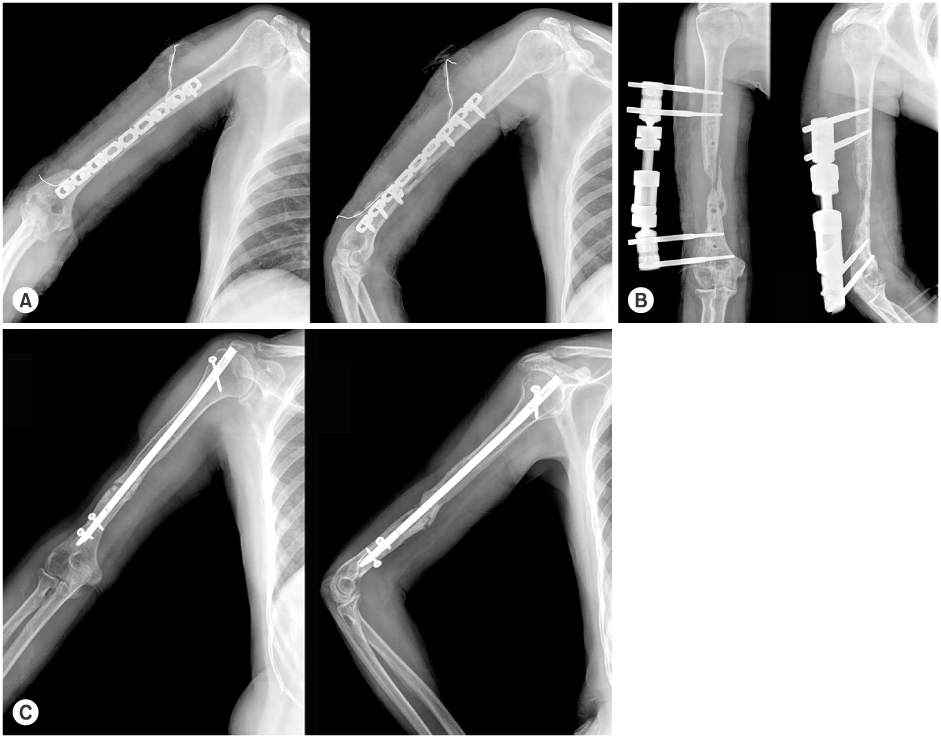
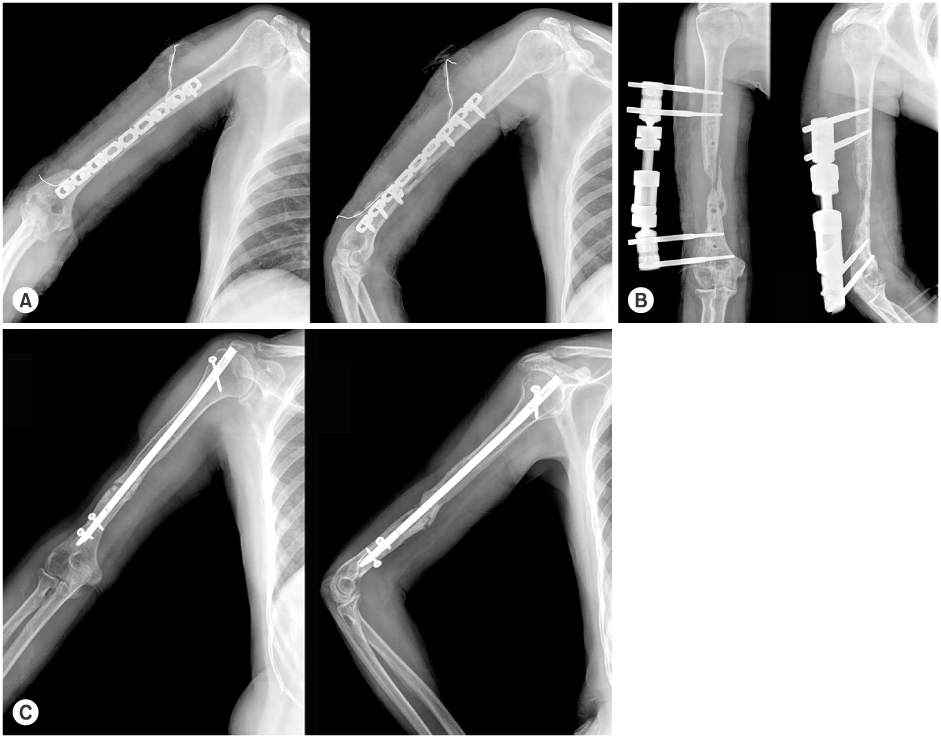
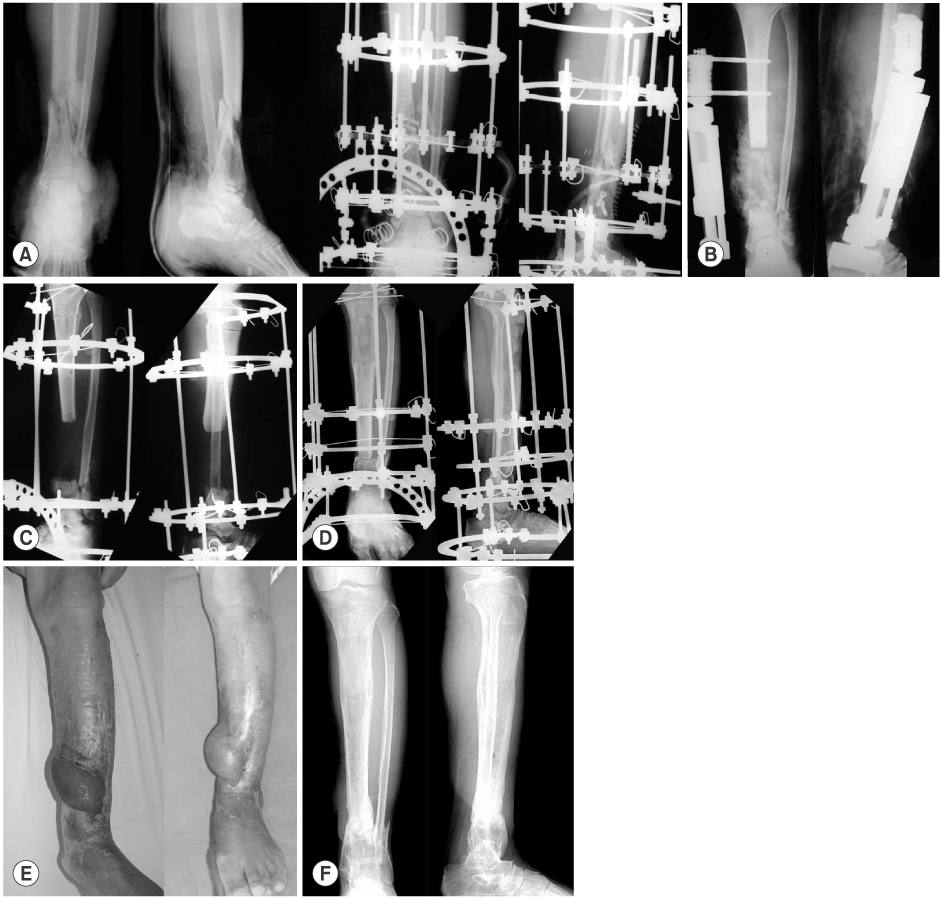
Fig. 3
(B) Removal of implant and debridement was performed, and external fixator and antibiotic mixed cement bead was inserted to control infection.
(C) External fixator was removed, and debridement & reinsertion of antibiotic mixed cement bead was inserted for infection control.
(D) Last follow up radiograph shows complete bone union with plate fixation and cancellous bone graft.
(A) The radiograph shows femur proximal shaft comminuted fracture fixated with open intramedullary nailing. The patient showed pus discharge from the fracture site.
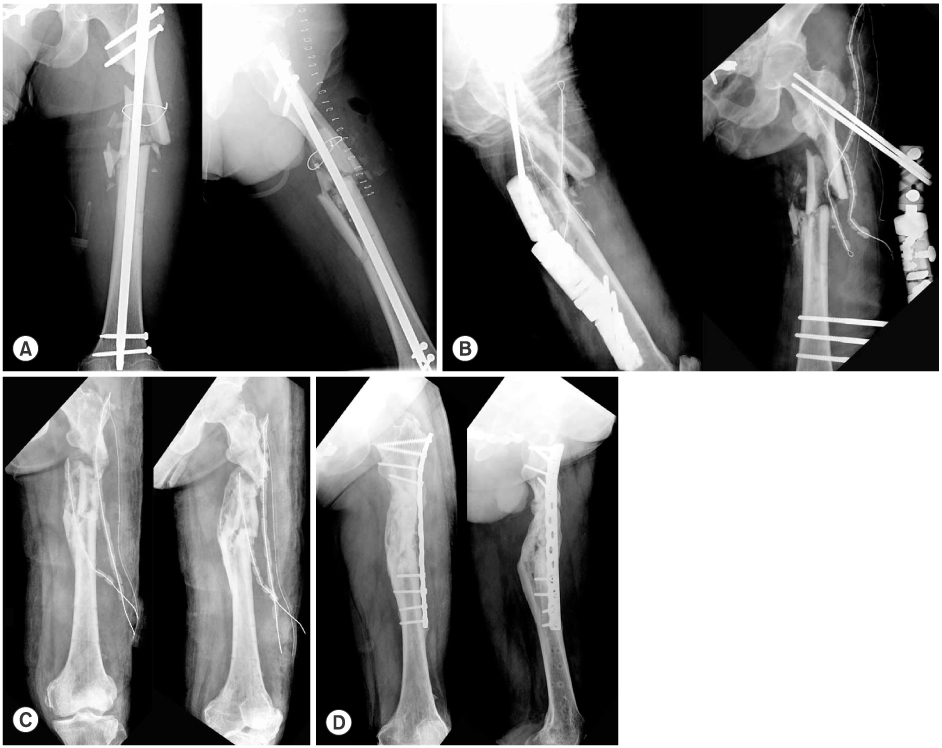
Fig. 4
(B) Internal fixator was removed and antibiotic mixed cement spacer was inserted to fill the bony defect of infected nonunion site with steinman pin and antibiotic mixed cement bead in proximal femur.
(C) After spacer removal and strut bone graft, the radiograph show complete union with posterior angulation of distal femur.

(A) The picture of 28 year-old-male 6months following initial operation shows nonunion of distal femur. The patient had pus discharge from the fracture site.

Fig. 5
(B) At 2 months following initial operation, pus discharge and fracture site displacement was observed. Sequestered bone was resected and cement bead was inserted to control infection.
(C) After infection was controlled, Ilizarov fixator was applied for the lengthening of tibia.
(D) Radiograph shows complete bone union with good alignment of tibia with ankle joint in fusion state.

(A) Radiograph of a 45-year-old male shows right pilon fracture with lateral malleolar fracture (open III-b) treated with Ilizarov fixator.

Fig. 6
(B) At 2 months following operation, pus discharge and displacement of fracture site was observed. Nonviable bone was resected with antibiotic mixed cement bead insertion for infection control and external fixator for stabilization.
(C) After the infection control, Ilizarov external fixation and corticotomy was done for the lengthening of tibia.
(D) Tibia lengthening of 15 cm was achieved after 7 months.
(E) Skin defect was covered with rotational hemisoleus muscle flap and split thickness skin graft.
(F) Last follow up radiograph shows complete bone union with good alignment.
(A) Radiographs shows 47-year-old male with left pilon fracture and distal tibio-fbular fracture with initial treatment using Ilizarov fixator.
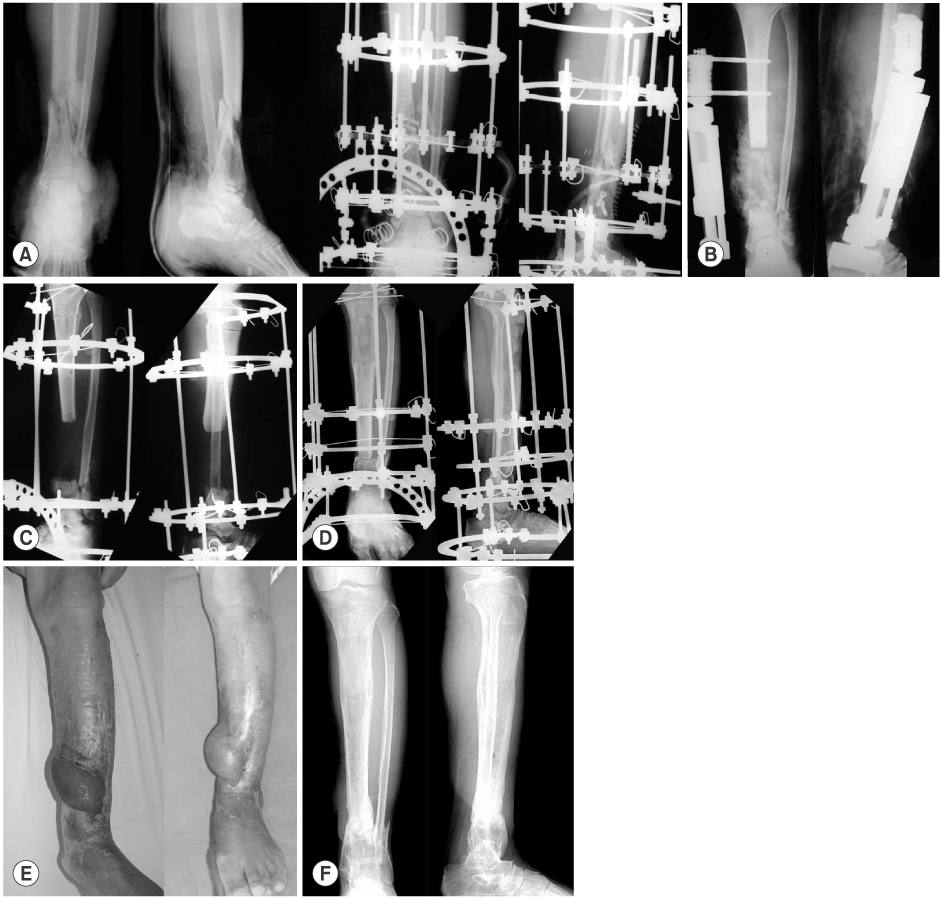
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Treatment Strategy of Infected Nonunion
Hyoung-Keun Oh
Journal of the Korean Fracture Society.2017; 30(1): 52. CrossRef
Treatment of Infected Nonunion
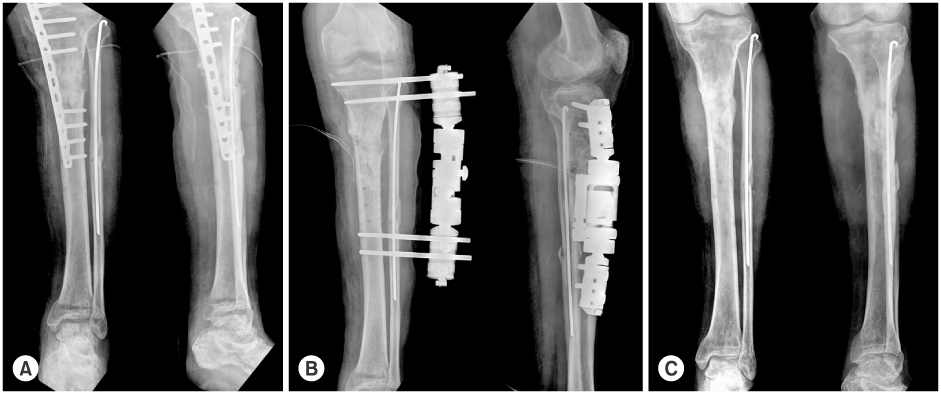
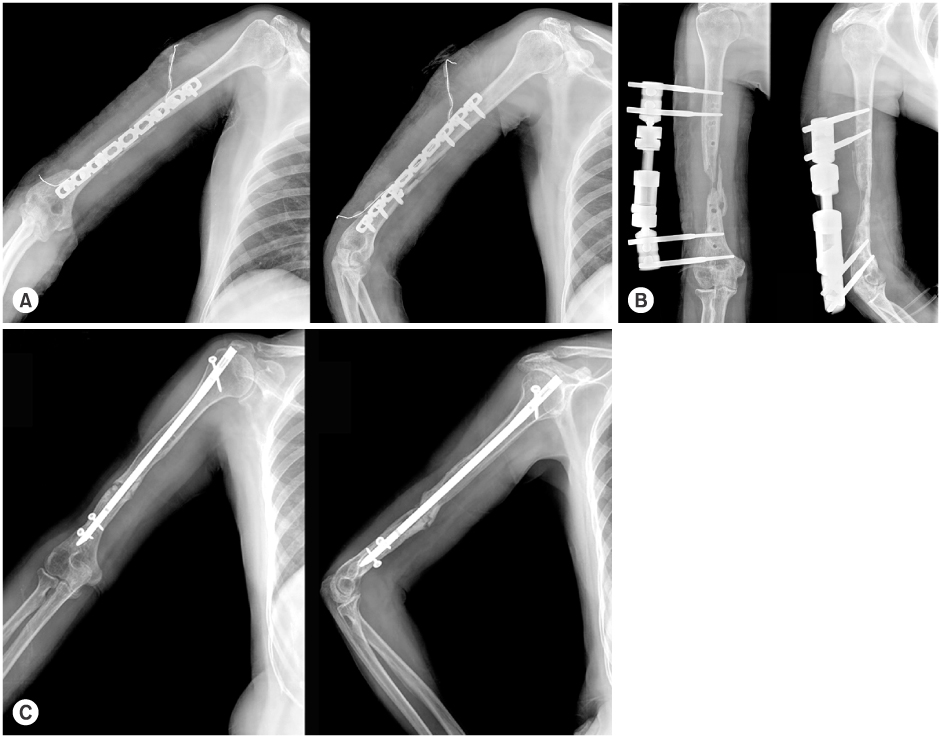
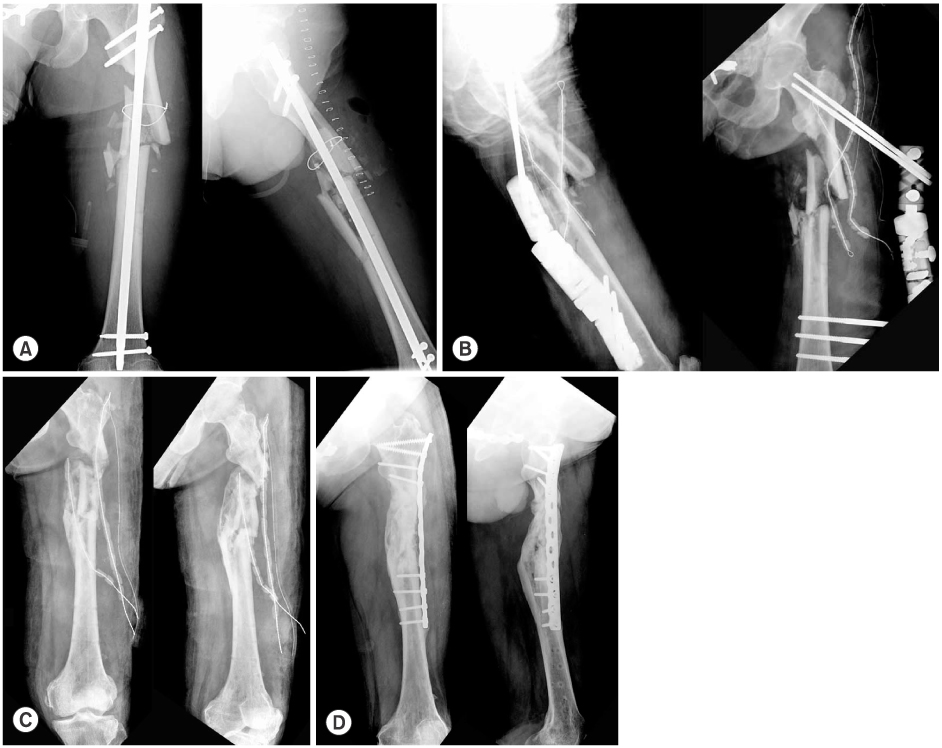
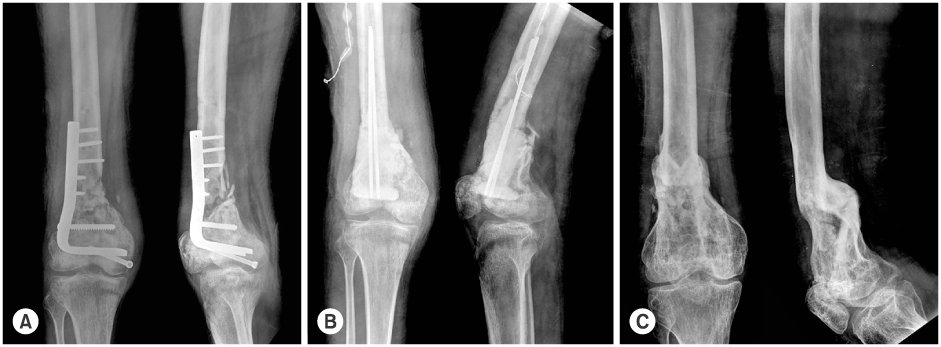

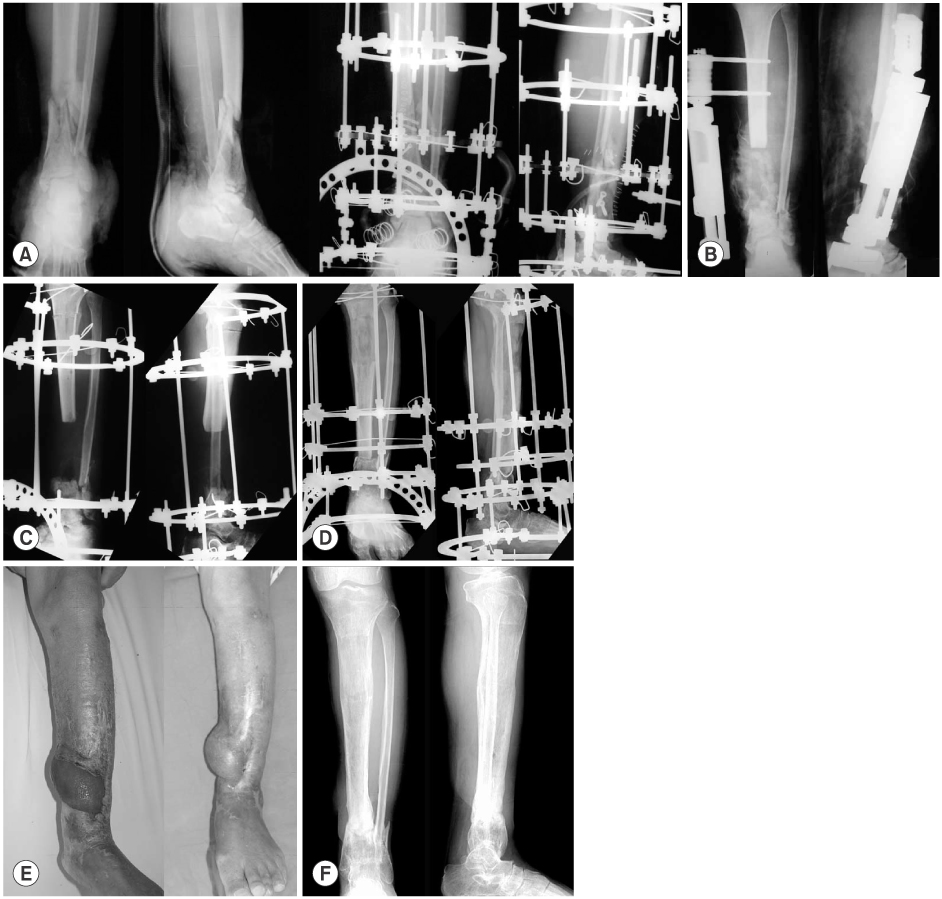
Fig. 1
(A) The radiograph shows tibia proximal shaft fracture with LCP applied. The patient showed pus discharge from the fracture site and loosening of the implants.
(B) Implant removal and debridement of the infected nonunion site was done with stabilization using external fixator.
(C) Last follow up radiograph shows complete bone union with good alignment.
Fig. 2
(A) Debridement and antibiotic mixed cement bead insertion was done but infection was not controlled.
(B) Sequestrectomy and debridement was done with external fixator applied.
(C) The external fixator was changed to intramedullary nail with strut bone graft. Radiograph shows partial bone union with good alignment.
Fig. 3
(A) The radiograph shows femur proximal shaft comminuted fracture fixated with open intramedullary nailing. The patient showed pus discharge from the fracture site.
(B) Removal of implant and debridement was performed, and external fixator and antibiotic mixed cement bead was inserted to control infection.
(C) External fixator was removed, and debridement & reinsertion of antibiotic mixed cement bead was inserted for infection control.
(D) Last follow up radiograph shows complete bone union with plate fixation and cancellous bone graft.
Fig. 4
(A) The picture of 28 year-old-male 6months following initial operation shows nonunion of distal femur. The patient had pus discharge from the fracture site.
(B) Internal fixator was removed and antibiotic mixed cement spacer was inserted to fill the bony defect of infected nonunion site with steinman pin and antibiotic mixed cement bead in proximal femur.
(C) After spacer removal and strut bone graft, the radiograph show complete union with posterior angulation of distal femur.
Fig. 5
(A) Radiograph of a 45-year-old male shows right pilon fracture with lateral malleolar fracture (open III-b) treated with Ilizarov fixator.
(B) At 2 months following initial operation, pus discharge and fracture site displacement was observed. Sequestered bone was resected and cement bead was inserted to control infection.
(C) After infection was controlled, Ilizarov fixator was applied for the lengthening of tibia.
(D) Radiograph shows complete bone union with good alignment of tibia with ankle joint in fusion state.
Fig. 6
(A) Radiographs shows 47-year-old male with left pilon fracture and distal tibio-fbular fracture with initial treatment using Ilizarov fixator.
(B) At 2 months following operation, pus discharge and displacement of fracture site was observed. Nonviable bone was resected with antibiotic mixed cement bead insertion for infection control and external fixator for stabilization.
(C) After the infection control, Ilizarov external fixation and corticotomy was done for the lengthening of tibia.
(D) Tibia lengthening of 15 cm was achieved after 7 months.
(E) Skin defect was covered with rotational hemisoleus muscle flap and split thickness skin graft.
(F) Last follow up radiograph shows complete bone union with good alignment.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Treatment of Infected Nonunion

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

