Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 27(4); 2014 > Article
-
Review Article
- Non-Operative Treatment of Nonunion
- Oog Jin Shon, M.D., Man-Ho Lee, M.D., Hyo Sae Ahn, M.D.
-
Journal of the Korean Fracture Society 2014;27(4):338-347.
DOI: https://doi.org/10.12671/jkfs.2014.27.4.338
Published online: October 20, 2014
Department of Orthopedic Surgery, Yeungnam University College of Medicine, Daegu, Korea.
- Address reprint requests to: Oog Jin Shon, M.D. Department of Orthopedic Surgery, Yeungnam University Medical Center, 170 Hyeonchung-ro, Nam-gu, Daegu 705-703, Korea. Tel: 82-53-620-3640, Fax: 82-53-628-4020, maestro-jin@hanmail.net
Copyright © 2014 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,163 Views
- 9 Download
- 2 Crossref
- 1. Axelrad TW, Kakar S, Einhorn TA. New technologies for the enhancement of skeletal repair. Injury, 2007;38:Suppl 1. S49-S62.Article
- 2. Hayda RA, Brighton CT, Esterhai JL Jr. Pathophysiology of delayed healing. Clin Orthop Relat Res, 1998;355 Suppl. S31-S40.ArticlePubMed
- 3. Ellegaard M, Jørgensen NR, Schwarz P. Parathyroid hormone and bone healing. Calcif Tissue Int, 2010;87:1-13.ArticlePubMedPDF
- 4. Brinker MR, O'Connor DP, Monla YT, Earthman TP. Metabolic and endocrine abnormalities in patients with nonunions. J Orthop Trauma, 2007;21:557-570.ArticlePubMed
- 5. Doepfner W. Consequences of calcium and-or phosphorus deficient diets on various parameters of callus formation and on growth rate in young rats. Br J Pharmacol, 1970;39:188P-189P.ArticlePubMedPMC
- 6. Einhorn TA, Bonnarens F, Burstein AH. The contributions of dietary protein and mineral to the healing of experimental fractures. A biomechanical study. J Bone Joint Surg Am, 1986;68:1389-1395.ArticlePubMed
- 7. Koskinen EV, Ryoppy SA, Lindholm TS. Bone formation by induction under the influence of growth hormone and cortisone. Isr J Med Sci, 1971;7:378-380.ArticlePubMed
- 8. Nichols JT, Toto PD, Choukas NC. The proliferative capacity and DNA synthesis of osteoblasts during fracture repair in normal and hypophysectomized rats. Oral Surg Oral Med Oral Pathol, 1968;25:418-426.ArticlePubMed
- 9. Krakauer JC, McKenna MJ, Buderer NF, Rao DS, Whitehouse FW, Parfitt AM. Bone loss and bone turnover in diabetes. Diabetes, 1995;44:775-782.ArticlePubMed
- 10. Adams CI, Keating JF, Court-Brown CM. Cigarette smoking and open tibial fractures. Injury, 2001;32:61-65.ArticlePubMed
- 11. Porter SE, Hanley EN Jr. The musculoskeletal effects of smoking. J Am Acad Orthop Surg, 2001;9:9-17.ArticlePubMed
- 12. Babhulkar S, Pande K, Babhulkar S. Nonunion of the diaphysis of long bones. Clin Orthop Relat Res, 2005;(431):50-56.Article
- 13. Brighton CT, Pollack SR. Treatment of recalcitrant non-union with a capacitively coupled electrical field. A preliminary report. J Bone Joint Surg Am, 1985;67:577-585.ArticlePubMed
- 14. Diniz P, Shomura K, Soejima K, Ito G. Effects of pulsed electromagnetic field (PEMF) stimulation on bone tissue like formation are dependent on the maturation stages of the osteoblasts. Bioelectromagnetics, 2002;23:398-405.ArticlePubMed
- 15. Hannouche D, Petite H, Sedel L. Current trends in the enhancement of fracture healing. J Bone Joint Surg Br, 2001;83:157-164.ArticlePubMedPDF
- 16. Ciombor DM, Aaron RK. The role of electrical stimulation in bone repair. Foot Ankle Clin, 2005;10:579-593.ArticlePubMed
- 17. Megas P. Classification of non-union. Injury, 2005;36:Suppl 4. S30-S37.ArticlePubMed
- 18. Nelson FR, Brighton CT, Ryaby J, et al. Use of physical forces in bone healing. J Am Acad Orthop Surg, 2003;11:344-354.ArticlePubMed
- 19. Heckman JD, Ryaby JP, McCabe J, Frey JJ, Kilcoyne RF. Acceleration of tibial fracture-healing by non-invasive, low-intensity pulsed ultrasound. J Bone Joint Surg Am, 1994;76:26-34.ArticlePubMed
- 20. Kristiansen TK, Ryaby JP, McCabe J, Frey JJ, Roe LR. Accelerated healing of distal radial fractures with the use of specific, low-intensity ultrasound. A multicenter, prospective, randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am, 1997;79:961-973.ArticlePubMed
- 21. Hadjiargyrou M, McLeod K, Ryaby JP, Rubin C. Enhancement of fracture healing by low intensity ultrasound. Clin Orthop Relat Res, 1998;355 Suppl. S216-S229.ArticlePubMed
- 22. Ito M, Azuma Y, Ohta T, Komoriya K. Effects of ultrasound and 1,25-dihydroxyvitamin D3 on growth factor secretion in co-cultures of osteoblasts and endothelial cells. Ultrasound Med Biol, 2000;26:161-166.ArticlePubMed
- 23. Parvizi J, Wu CC, Lewallen DG, Greenleaf JF, Bolander ME. Low-intensity ultrasound stimulates proteoglycan synthesis in rat chondrocytes by increasing aggrecan gene expression. J Orthop Res, 1999;17:488-494.ArticlePubMed
- 24. Gebauer D, Correll J. Pulsed low-intensity ultrasound: a new salvage procedure for delayed unions and nonunions after leg lengthening in children. J Pediatr Orthop, 2005;25:750-754.ArticlePubMed
- 25. Nolte PA, van der Krans A, Patka P, Janssen IM, Ryaby JP, Albers GH. Low-intensity pulsed ultrasound in the treatment of nonunions. J Trauma, 2001;51:693-702.ArticlePubMed
- 26. Tamma R, dell'Endice S, Notarnicola A, et al. Extracorporeal shock waves stimulate osteoblast activities. Ultrasound Med Biol, 2009;35:2093-2100.ArticlePubMed
- 27. Zelle BA, Gollwitzer H, Zlowodzki M, Bühren V. Extracorporeal shock wave therapy: current evidence. J Orthop Trauma, 2010;24:Suppl 1. S66-S70.ArticlePubMed
- 28. Skripitz R, Andreassen TT, Aspenberg P. Strong effect of PTH (1-34) on regenerating bone: a time sequence study in rats. Acta Orthop Scand, 2000;71:619-624.ArticlePubMed
- 29. Skripitz R, Aspenberg P. Implant fixation enhanced by intermittent treatment with parathyroid hormone. J Bone Joint Surg Br, 2001;83:437-440.ArticlePubMed
- 30. Kakar S, Einhorn TA, Vora S, et al. Enhanced chondrogenesis and Wnt signaling in PTH-treated fractures. J Bone Miner Res, 2007;22:1903-1912.ArticlePubMedPDF
- 31. Kaback LA, Soung do Y, Naik A, et al. Teriparatide (1-34 human PTH) regulation of osterix during fracture repair. J Cell Biochem, 2008;105:219-226.ArticlePubMedPMC
- 32. Sampath TK, DeSimone DP, Reddi AH. Extracellular bone matrix-derived growth factor. Exp Cell Res, 1982;142:460-464.ArticlePubMed
- 33. Sampath TK, Reddi AH. Homology of bone-inductive proteins from human, monkey, bovine, and rat extracellular matrix. Proc Natl Acad Sci U S A, 1983;80:6591-6595.ArticlePubMedPMC
- 34. Asahina I, Sampath TK, Nishimura I, Hauschka PV. Human osteogenic protein-1 induces both chondroblastic and osteoblastic differentiation of osteoprogenitor cells derived from newborn rat calvaria. J Cell Biol, 1993;123:921-933.ArticlePubMedPMCPDF
- 35. Reddi AH. Role of morphogenetic proteins in skeletal tissue engineering and regeneration. Nat Biotechnol, 1998;16:247-252.ArticlePubMedPDF
- 36. Cook SD, Wolfe MW, Salkeld SL, Rueger DC. Effect of recombinant human osteogenic protein-1 on healing of segmental defects in non-human primates. J Bone Joint Surg Am, 1995;77:734-750.ArticlePubMed
- 37. Louwerse RT, Heyligers IC, Klein-Nulend J, et al. Use of recombinant human osteogenic protein-1 for the repair of subchondral defects in articular cartilage in goats. J Biomed Mater Res, 2000;49:506-516.ArticlePubMed
- 38. Mermer MJ, Gupta MC, Wheeler DL, et al. Efficacy of osteogenic protein-1 in a challenging multilevel fusion model. Spine (Phila Pa 1976), 2004;29:249-256.ArticlePubMed
- 39. Mizumoto Y, Moseley T, Drews M, Cooper VN 3rd, Reddi AH. Acceleration of regenerate ossification during distraction osteogenesis with recombinant human bone morphogenetic protein-7. J Bone Joint Surg Am, 2003;85:Suppl 3. 124-130.Article
- 40. Geesink RG, Hoefnagels NH, Bulstra SK. Osteogenic activity of OP-1 bone morphogenetic protein (BMP-7) in a human fibular defect. J Bone Joint Surg Br, 1999;81:710-718.ArticlePubMed
- 41. Friedlaender GE, Perry CR, Cole JD, et al. Osteogenic protein-1 (bone morphogenetic protein-7) in the treatment of tibial nonunions. J Bone Joint Surg Am, 2001;83:Suppl 1. S151-S158.ArticlePubMed
- 42. Pecina M, Giltaij LR, Vukicevic S. Orthopaedic applications of osteogenic protein-1 (BMP-7). Int Orthop, 2001;25:203-208.ArticlePubMedPMCPDF
- 43. Yokota H, Tanaka SM. Osteogenic potentials with joint-loading modality. J Bone Miner Metab, 2005;23:302-308.ArticlePubMedPDF
- 44. Wu CC. The effect of dynamization on slowing the healing of femur shaft fractures after interlocking nailing. J Trauma, 1997;43:263-267.ArticlePubMed
- 45. Wu CC, Chen WJ. Healing of 56 segmental femoral shaft fractures after locked nailing. Poor results of dynamization. Acta Orthop Scand, 1997;68:537-540.ArticlePubMed
- 46. Pihlajamäki HK, Salminen ST, Böstman OM. The treatment of nonunions following intramedullary nailing of femoral shaft fractures. J Orthop Trauma, 2002;16:394-402.ArticlePubMed
- 47. Goujon E. Recherches experimentales sur les propriétes du tissu osseux. J L Anat, 1869;6:399-412.Article
- 48. Salama R, Weissman SL. The clinical use of combined xenografts of bone and autologous red marrow. A preliminary report. J Bone Joint Surg Br, 1978;60:111-115.ArticlePubMedPDF
- 49. Lindholm TS, Urist MR. A quantitative analysis of new bone formation by induction in compositive grafts of bone marrow and bone matrix. Clin Orthop Relat Res, 1980;(150):288-300.Article
- 50. Burwell RG. The function of bone marrow in the incorporation of a bone graft. Clin Orthop Relat Res, 1985;(200):125-141.Article
- 51. Hernigou P, Poignard A, Manicom O, Mathieu G, Rouard H. The use of percutaneous autologous bone marrow transplantation in nonunion and avascular necrosis of bone. J Bone Joint Surg Br, 2005;87:896-902.ArticlePubMedPDF
- 52. Kurz LT, Garfin SR, Booth RE Jr. Harvesting autogenous iliac bone grafts. A review of complications and techniques. Spine (Phila Pa 1976), 1989;14:1324-1331.ArticlePubMed
- 53. Seiler JG 3rd, Johnson J. Iliac crest autogenous bone grafting: donor site complications. J South Orthop Assoc, 2000;9:91-97.ArticlePubMed
- 54. Bolano L, Kopta JA. The immunology of bone and cartilage transplantation. Orthopedics, 1991;14:987-996.ArticlePubMed
- 55. Horowitz MC, Friedlaender GE. Immunologic aspects of bone transplantation. A rationale for future studies. Orthop Clin North Am, 1987;18:227-233.ArticlePubMed
- 56. Schmidmaier G, Herrmann S, Green J, et al. Quantitative assessment of growth factors in reaming aspirate, iliac crest, and platelet preparation. Bone, 2006;39:1156-1163.ArticlePubMed
REFERENCES
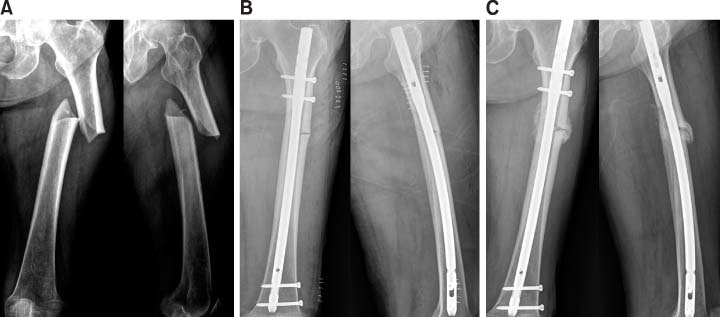
Fig. 5
(A) A 64-year-old man with a right tibio-fibular shaft fracture. (B) OR/IF with tibia nail was performed. (C) Five months after the operation, nonunion had developed (arrow). (D) Dynamization was performed. (E) Eight months after the operation (arrow). (F) Computed tomography (CT) image at 13 months after the operation, nonunion was still seen. (G) After use of EXOGEN® for three months, union had progressed on the CT image. (H) Twenty months after the first operation, union was achieved.
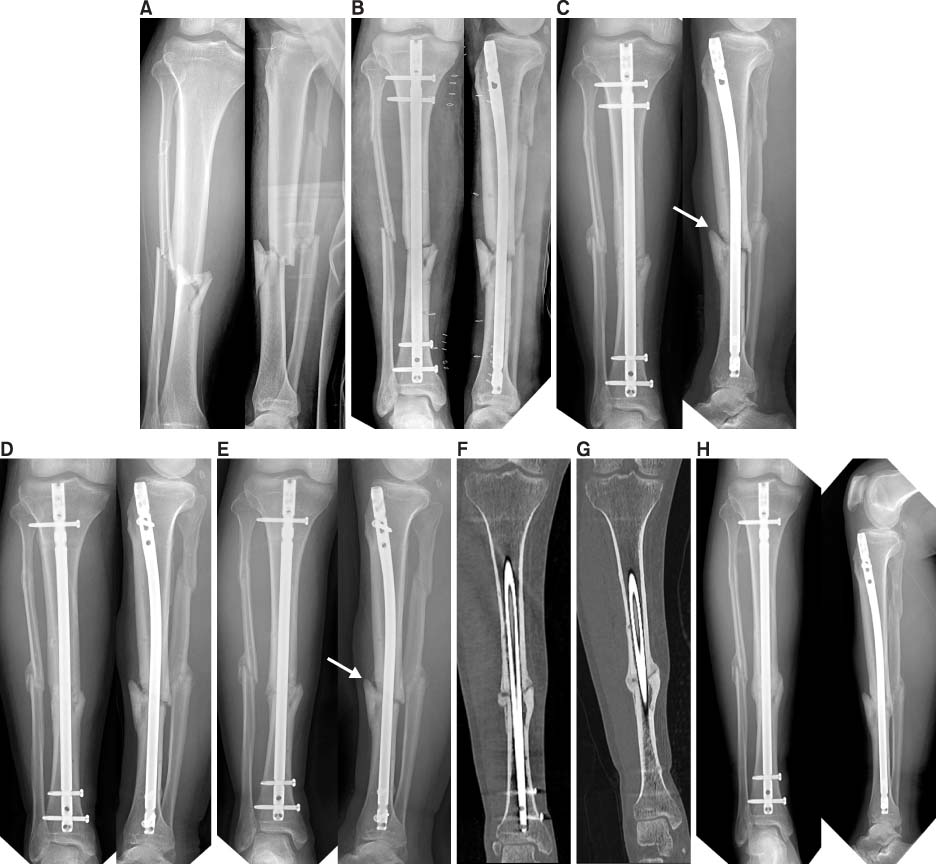
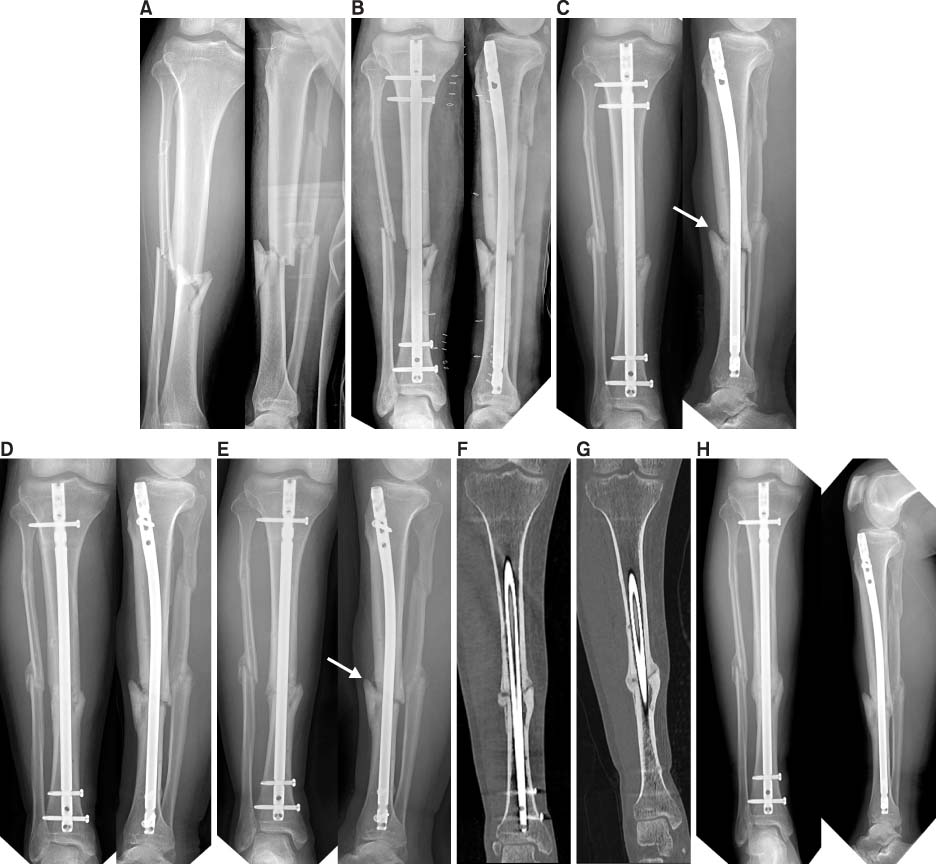
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- A Novel Triad of Bio-Inspired Design, Digital Fabrication, and Bio-Derived Materials for Personalised Bone Repair
Greta Dei Rossi, Laura Maria Vergani, Federica Buccino
Materials.2024; 17(21): 5305. CrossRef - The Clinical Effects of Complex Korean Medicine Treatment in Patient with Delayed Union of the 4th Toe Distal Phalanx Fracture
Kyungtae Park, Hee-Ra Shin, Sung-Hu An, Seung-Ryong Yeom, Young-Dal Kwon
Journal of Korean Medicine Rehabilitation.2019; 29(4): 143. CrossRef
Non-Operative Treatment of Nonunion
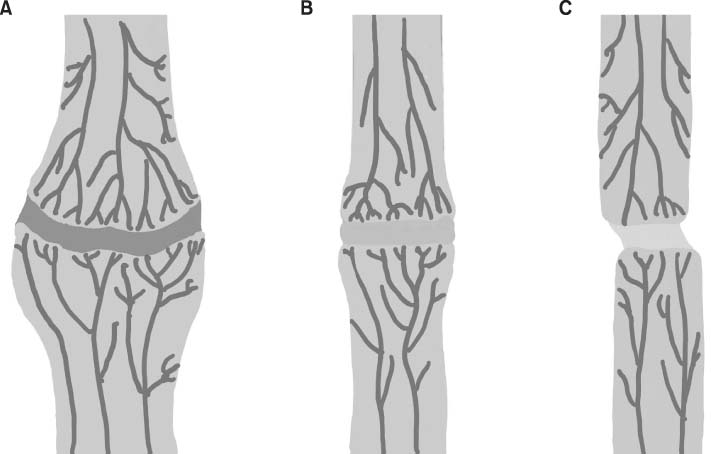
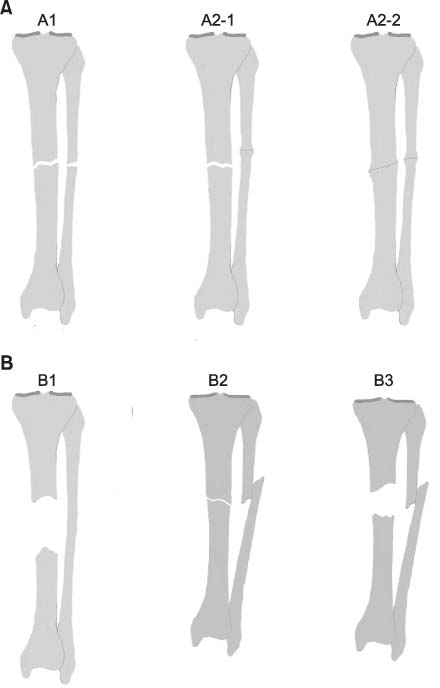

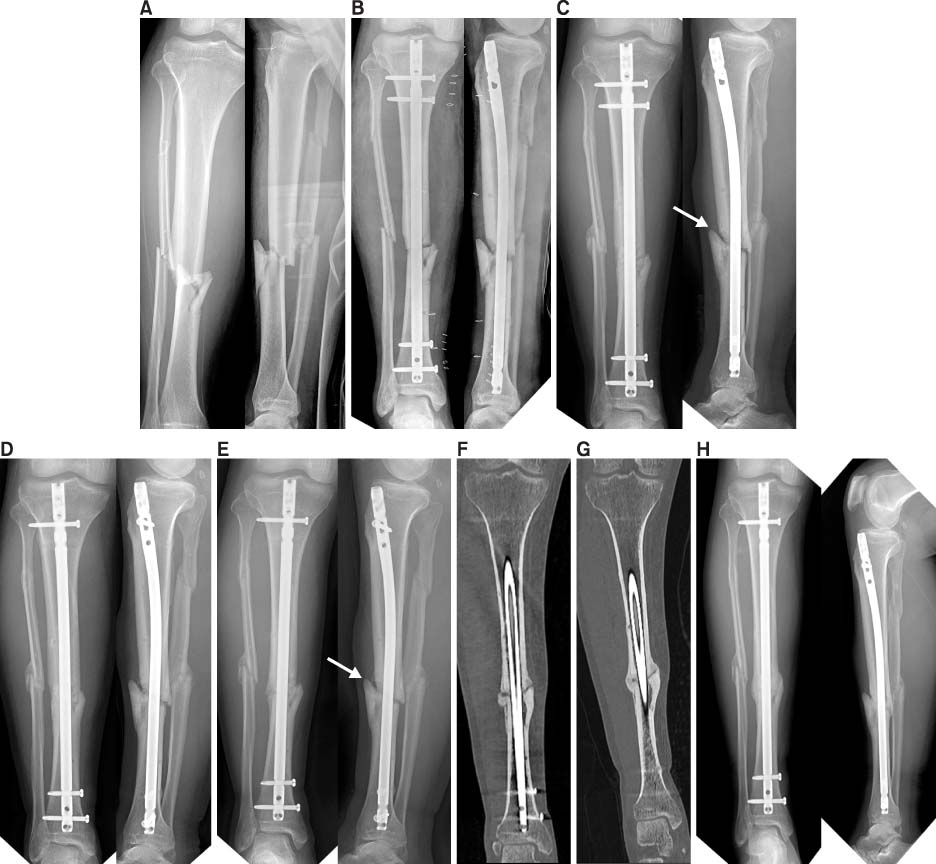

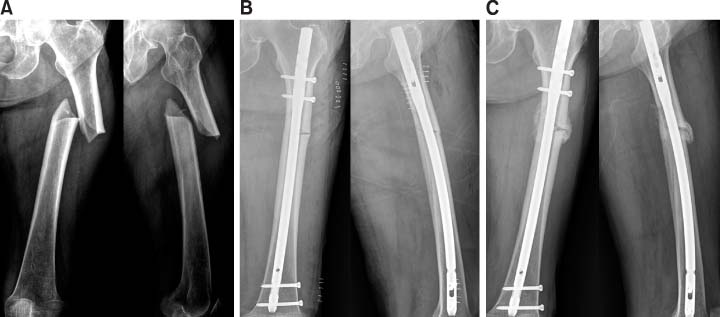
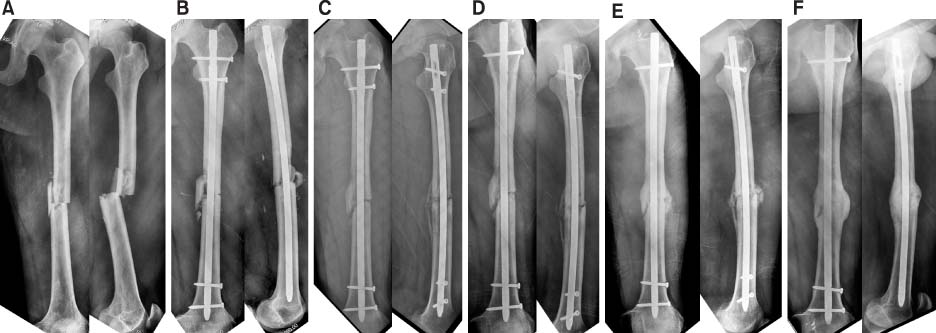
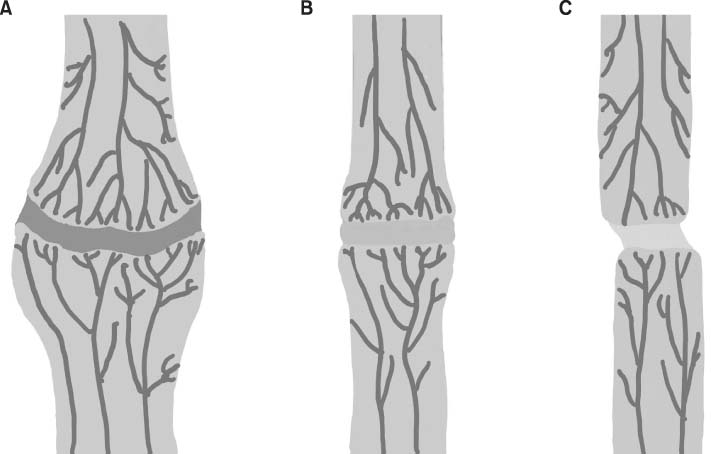
Fig. 1
Hypervascular nonunions. (A) Elephant foot. (B) Horse hoof. (C) Oligotrophic.
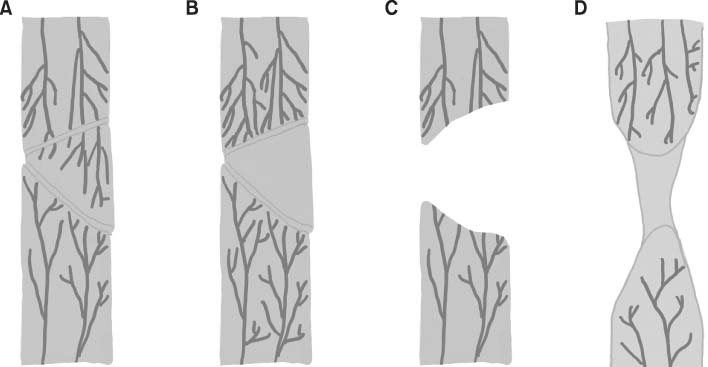
Fig. 2
Avascular nonunions. (A) Torsion wedge. (B) Comminuted. (C) Defect. (D) Atrophic.
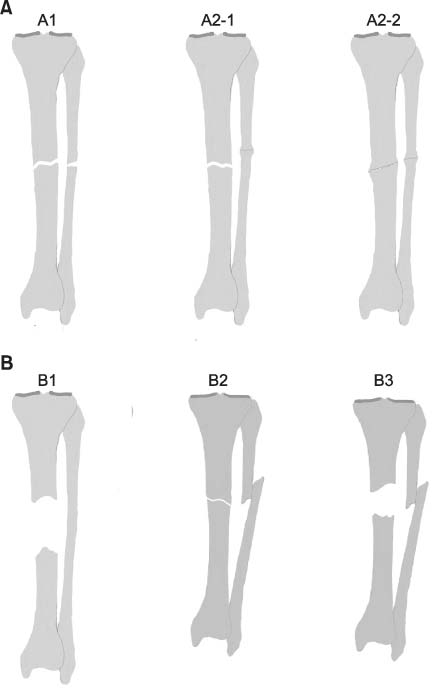
Fig. 3
Classification of nonunions by Paley et al. (A) Type A nonunion. (B) Type B nonunion.
Fig. 4
EXOGEN® Smith & Nephew, Inc. USA.
Fig. 5
(A) A 64-year-old man with a right tibio-fibular shaft fracture. (B) OR/IF with tibia nail was performed. (C) Five months after the operation, nonunion had developed (arrow). (D) Dynamization was performed. (E) Eight months after the operation (arrow). (F) Computed tomography (CT) image at 13 months after the operation, nonunion was still seen. (G) After use of EXOGEN® for three months, union had progressed on the CT image. (H) Twenty months after the first operation, union was achieved.
Fig. 6
FORTEO® Lilly USA.
Fig. 7
(A) An 84-year-old woman with a left femur shaft insufficiency fracture. (B) OR/IF with femoral nail was performed. (C) With use of FORTEO®, union had progressed at two months after the operation.
Fig. 8
(A) A 25-year-old man with a left femur shaft fracture. (B) OR/IF with femoral nail was performed. (C) Seven months after the operation, nonunion was seen. (D) Dynamization was performed. (E) Two months after dynamization, callus formation was seen. (F) Finally, union was achieved.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
Non-Operative Treatment of Nonunion

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS



 Cite
Cite

