Search
- Page Path
- HOME > Search
Review Articles
- Fracture-related infections: a comprehensive review of diagnosis and prevention
- HoeJeong Chung, Hoon-Sang Sohn
- J Musculoskelet Trauma 2025;38(2):86-95. Published online April 25, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00164
-
 Abstract
Abstract
 PDF
PDF - Fracture-related infections are challenging complications in orthopedic trauma that often require prolonged treatment and impose a significant healthcare burden. Accurate diagnosis and effective prevention strategies are essential for minimizing their occurrence. A recent international consensus has established standardized diagnostic criteria based on clinical, microbiological, radiological, and histopathological findings. Prevention is the top priority and involves a thorough preoperative risk assessment, along with glycemic control, nutritional optimization, and management of comorbidities, as well as intraoperative and postoperative measures such as appropriate antibiotic prophylaxis, surgical site antisepsis, and meticulous wound care. A multidisciplinary approach involving orthopedic surgeons, infectious disease specialists, and microbiologists is crucial for successfully reducing the burden of fracture-related infections.
-
Citations
Citations to this article as recorded by- Personalized Approaches to Diagnostic and Therapeutic Strategies in Periprosthetic Fracture-Related Infections (PFRIs): Case Series and Literature Review
Marianna Faggiani, Marco Zugnoni, Matteo Olivero, Salvatore Risitano, Giuseppe Malizia, Silvia Scabini, Marcello Capella, Stefano Artiaco, Simone Sanfilippo, Alessandro Massè
Journal of Personalized Medicine.2025; 15(12): 576. CrossRef - Pathogen-Specific Risk for Iterative Surgical Debridement in Orthopedic Infections: A Prospective Multicohort Analysis
Flamur Zendeli, Anna Jędrusik, Raymond O. Schaefer, David Albrecht, Michael Betz, Felix W. A. Waibel, Tanja Gröber, Nathalie Kühne, Sören Könneker, İlker Uçkay
Journal of Clinical Medicine.2025; 14(24): 8750. CrossRef
- Personalized Approaches to Diagnostic and Therapeutic Strategies in Periprosthetic Fracture-Related Infections (PFRIs): Case Series and Literature Review
- 5,972 View
- 219 Download
- 2 Crossref

- Systematic Diagnosis and Treatment Principles for Acute Fracture-Related Infections
- Jeong-Seok Choi, Jun-Hyeok Kwon, Seong-Hyun Kang, Yun-Ki Ryu, Won-Seok Choi, Jong-Keon Oh, Jae-Woo Cho
- J Korean Fract Soc 2023;36(4):148-161. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.148
-
 Abstract
Abstract
 PDF
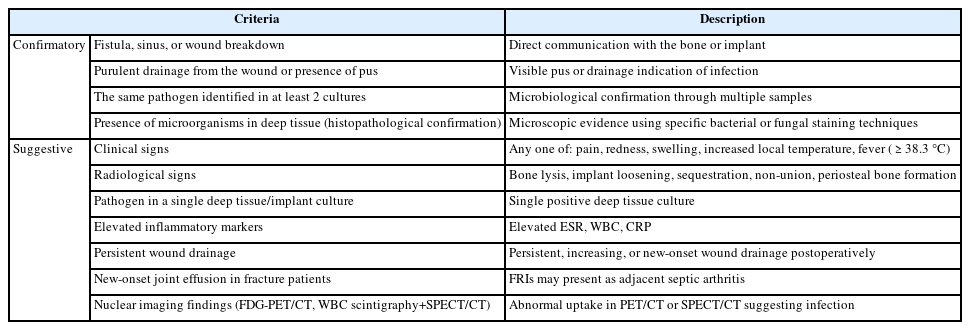
PDF - Acute fracture-related infection (FRI) is a common and serious complication of fracture treatment. The clinical symptoms of the patient and the results of the serological, radiological, and histopathologi-cal examinations can be divided into ‘Confirmatory’ criteria and ‘Suggestive’ criteria, allowing for the diagnosis of FRI. Treatment principles can be broadly categorized into (1) the DAIR (Debridement, Antimicrobial therapy, Implant Retention) method and (2) the staged reconstruction method. The choice of treatment depends on factors such as the time elapsed after infection, stability of the internal fixation device, reduction status, host physiology, and virulence of the pathogens. Thorough surgical debridement and irrigation, ensuring stability at the fracture site, reconstruction of bone defects, and appropriate soft tissue coverage, along with antibiotic therapy, are essential to suppress or eradicate the infection. The restoration of limb function should be promoted through proper soft tissue coverage and bone union at the fracture site.
- 708 View
- 15 Download

- Fracture-Related Complications: What You Can Do to Prevent Infection
- HoeJeong Chung, Jin Woo Lee, Sang-Ho Lee, Hoon-Sang Sohn
- J Korean Fract Soc 2023;36(4):139-147. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.139
-
 Abstract
Abstract
 PDF
PDF - Fracture-related infections (FRI) can occur when bacteria enter the wound during a traumatic injury. All efforts should be made to prevent FRI-associated complications due to the complexity of treatment at the time of onset and poor treatment outcomes. The risk factors for FRIs vary and several preoperative, perioperative, and postoperative measures can be implemented to prevent infections. Preoperative measures include blood sugar control, nutritional support, discontinuation of steroids and immunosuppressants, treatment of accompanying pre-existing infections, and decolonization of pathogens, specifically Staphylococcus aureus. The perioperative and postoperative measures include the use of prophylactic antibiotics, proper surgical site preparation (hair removal, preoperative washing, skin antisepsis), suitable surgical environment (operating room ventilation system, behavioral interventions in the operating room), correct surgical techniques (debridement, irrigation, wound closure, and negative pressure wound therapy). All medical staff should pay careful attention and ensure the implementation of the correct preventive measures.
- 688 View
- 26 Download

Original Article
- Usefulness of Sonication in Implant-Related Infection
- Jae Hyeon Seo, Mi Na Kim, Ji Wan Kim
- J Korean Fract Soc 2020;33(2):81-86. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.81
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study determined whether the sonication of explants could improve the detection of bacteria and influence the optimal antibiotics treatment.
Materials and Methods
This retrospective study included the patients who underwent implant removal surgery followed by sonication culture as well as tissue culture in order to diagnose implant-related infection. A total of 37 consecutive patients with 41 cases were included. The patients’ demographic data, use of preoperative antibiotics, type of implants, change of antibiotics following the culture results, and recurrence of infection were all reviewed.
Results
Among 41 cases, 20 cases met the diagnostic requirements for implant-related infection as defined by musculoskeletal infection society criteria, while the other 21 cases had explant sonication to exclude indolent infection or residual infection. The latter showed negative results on the both explant cultures and tissue cultures. Among the 20 cases that met the requirements for implant-related infection, 19 cases (95.0%) were identified by any cultures. Of the 19 cases with positive culture results, 2 cases (10.5%) showed positive results only on sonication cultures, and one case (5.3%) showed positive results only on tissue culture. In 1 case of culture negative implant-related infection, a drain sinus was present preoperatively, but the cultures were negative according to both methods. The culture results made postoperative antibiotics change in 12 cases among the 19 culture (+) cases. Antibiotics changes were based on the tissue culture in 2 cases, 2 cases were based on the sonication culture, and the remaining 8 cases were based on both cultures.
Conclusion
The sonication culture improved the diagnosis of implant-related infection combined with conventional tissue culture and helped to determine administering the proper antibiotics. -
Citations
Citations to this article as recorded by- Systematic Diagnosis and Treatment Principles for Acute Fracture-Related Infections
Jeong-Seok Choi, Jun-Hyeok Kwon, Seong-Hyun Kang, Yun-Ki Ryu, Won-Seok Choi, Jong-Keon Oh, Jae-Woo Cho
Journal of the Korean Fracture Society.2023; 36(4): 148. CrossRef
- Systematic Diagnosis and Treatment Principles for Acute Fracture-Related Infections
- 755 View
- 1 Download
- 1 Crossref

Review Article
- Treatment Strategy of Infected Nonunion
- Hyoung Keun Oh
- J Korean Fract Soc 2017;30(1):52-62. Published online January 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.1.52
-
 Abstract
Abstract
 PDF
PDF - The management of infected nonunion is based on a detailed evaluation of patients, the involved bone and soft tissues, stability of fixation, and type of bacterial pathogens. Preoperative surgical planning and strategies for each step is mandatory for the successful treatment of infected nonunion. The radical debridement of infected tissues, including the unstable implant, is one of the most important procedures. Adequate soft tissue coverage should be considered for the appropriate management of infection; a reconstructive procedure and stable skeletal stabilization by internal or external fixation is also necessary later. A restoration of bone defects and bony union can be accomplished with bone grafting, distraction osteogenesis, vascularized fibular grafting, and induced membrane technique.
-
Citations
Citations to this article as recorded by- Systematic Diagnosis and Treatment Principles for Acute Fracture-Related Infections
Jeong-Seok Choi, Jun-Hyeok Kwon, Seong-Hyun Kang, Yun-Ki Ryu, Won-Seok Choi, Jong-Keon Oh, Jae-Woo Cho
Journal of the Korean Fracture Society.2023; 36(4): 148. CrossRef - The Antibiotic Cement Coated Nail and Masquelet Technique for the Treatment of Infected Nonunion of Tibia with Bone Defect and Varus Deformity: A Case Report
Min Gu Jang, Jae Hwang Song, Dae Yeung Kim, Woo Jin Shin
Journal of the Korean Fracture Society.2022; 35(1): 26. CrossRef
- Systematic Diagnosis and Treatment Principles for Acute Fracture-Related Infections
- 1,399 View
- 23 Download
- 2 Crossref

Original Articles
- The Incidence of Infection in Interlocking Intramedullary Nailing after Skeletal Traction of Distal Femur
- Hyuk Woo Nam, Seung Woo Suh, Hae Reong Song, Jun Gyu Moon, Jun Ho Wang, Chan Eung Park, Jae Hyuk Yang
- J Korean Fract Soc 2005;18(1):12-16. Published online January 31, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.1.12
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The insertion site of K-wire for skeletal traction is proximal part of tibia or distal part of femur. However, people prefer proximal tibia over distal femur due to lower risk of infection rate when change to interlocking IM nailing is needed. We evaluated the infection rate of interlocking IM nailing.
MATERIALS AND METHODS
Fourty-seven patients were included in this study who underwent interlocking IM nailing due to femur shaft fracture. Traction was applied at the distal femur in 19 cases and proximal tibia in 10 cases before interlocking IM nailing. No skeletal traction was applied to the remaining 18 cases. Thirty-eight patients were male and 9 were female. The average age at the time of surgery was 36.7 years old (range, 15~17 years). The average traction period was 9.5 days (range, 3~33 days) and the average followed-up period was 17.2 months.
RESULTS
In the distal femoral traction group, 8 cases of superficial pin tract infection developed, but no case of deep infection such as osteomyelitis occurred. In the proximal tibia traction group, 2 cases of superficial pin tract infection developed, but no case of deep infection occurred. In the group that received no skeletal traction before interlocking IM nailing, no case of infection developed.
CONCLUSION
In femur shaft fracture, the distal femoral skeletal traction followed by interlocking IM nailing of femur, compared to proximal tibia skeletal traction, did not increase the risk of deep infection such as osteomyelitis. -
Citations
Citations to this article as recorded by- Rectus femoris muscle atrophy and recovery caused by preoperative pretibial traction in femoral shaft fractures-comparison between traction period
D.-G. Shim, T.-Y. Kwon, K.-B. Lee
Orthopaedics & Traumatology: Surgery & Research.2017; 103(5): 691. CrossRef
- Rectus femoris muscle atrophy and recovery caused by preoperative pretibial traction in femoral shaft fractures-comparison between traction period
- 585 View
- 4 Download
- 1 Crossref

- Differential diagnosis and its treatment of gas forming infections
- Soo Bong Hahn, Ho Jung Kang, Jin Park
- J Korean Soc Fract 2002;15(4):607-613. Published online October 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.4.607
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To establish the guidelines for the differential diagnosis and proper initial treatment of the gas forming infections through the review of literature and our clinical experiences.
MATERIALS AND METHODS
The radiological findings, clinical course, gram stain, bacterial culture, predisposing factors and treatment of four cases of gas forming infections from January 1994 to August 2001, were retrospectively analyzed.
RESULTS
Three cases diagnosed presumptively as gas gangrene were improved through amputation or disarticulation and intravenous antibiotics. One case diagnosed presumptively as non-clostridial infection was expired due to sepsis in spite of incision, drainage and intravenous antibiotics. In the bacterial culture, two cases were non-clostridial infection, one case was not able to diagnose and one case was clostridial myonecrosis(gas gangrene) CONCLUSION: The gas forming infections are rare but life-threatening. When the proper initial treatment is delayed, the fatal complications may result. So, the presumptive diagnosis through gram stain, clinical course, radiological findings should be made as soon as possible, and according to which, the appropriate initial treatment, such as, surgical debridement, amputation, intravenous antibiotics must be started. The following treatments should be corrected by definitive diagnosis through the bacterial culture. -
Citations
Citations to this article as recorded by- Salmonella gas-forming pyomyositis in an immunocompetent patient: a case report and review
Jee Young Lee, Gyu Min Kong
Journal of International Medical Research.2025;[Epub] CrossRef - Type I, II Acute Necrotizing Fasciitis of the Low Extremity
Sang-Jun Song, In Seok Lee, Ju Hwan Chung
The Journal of the Korean Orthopaedic Association.2007; 42(5): 636. CrossRef
- Salmonella gas-forming pyomyositis in an immunocompetent patient: a case report and review
- 502 View
- 0 Download
- 2 Crossref

- Operative Treatment of Open Tibial Fracture
- Kyung Jin Song, Sun Woong Jang
- J Korean Soc Fract 2002;15(1):45-51. Published online January 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.1.45
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of the present study was to clarify the contributing factors, such as the method of fracture stabilization, type of internal fixation and the deep infection rate(DIR) in the treatment of open tibial fractures. MATERIAL AND METHODS: We made a retrospective study of these 87 open tibial fractures treated with various fixation method. Patients were divided into immediate internal fixation(IIF) group, delayed internal fixation(DIF) group and external fixation(EF) groups. Fixation methods, deep infection rate related with fixation devices and time to bone union were compared and anaylzed according to the Gustilo`s classification.
RESULTS
The mean time to union in open type I, II, IIIa, IIIb, and IIIc was 5.7 months, 8.6 months, 7.1 months, 9.7 months, and 18.0 month respectively. The mean time to union in group IIF, DIF1, DIF2 and EF was 7.2 months, 8.1 months 5.5 months, and 10.7 months and 13.1 months. The mean time to union of group using a interlocking IM nailing, plate and screws, and external fixator was 6.3 month, 6.9 months, and 10.6 months. SUMMARY: We concluded that there is an advantage of immediate internal fixation over external fixation in the prevention of infection and promotion of fracture healing in the treatment of open tibia fractures. Immediate internal fixation could be recommended for type I, II, IIIa and some cases of IIIb open tibia fracture.
- 367 View
- 1 Download

- Management for Postoperative Infection of Fractures
- Eui Hwan Ahn, In Whan Chung, Jeong Hwan Oh, Seong Tae Lee, Duk Hwan Kho
- J Korean Soc Fract 1999;12(2):402-410. Published online April 30, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.2.402
-
 Abstract
Abstract
 PDF
PDF - It is often difficult to eradicate infection and achieve bony union in postoperative infection after fracture fixation. Authors treated 14 such cases from February 1992 to February 1998, and followed up for 6 to 35 months. The purpose of this study is to review the clinical features of the postoperative infection and assess the treatment modality which influence the time required for attaining bony union and healing of infection. The results were as follows : 1. Primary fixation were left in place in 5 cases of stable fixation, and new external fixation and/or another fixations were required in 8 cases of unstable fixation. 2. Time required for achieving union was 4.7 months for stable primary fixation and 12.8 months for unstable primary fixation. 3. Time required for healing in infection was 3.5 months for stable primary fixation and 14.4 months for unstable primary fixation. 4. Bony union was delayed as the number of surgical procedures were increased. 5. Antibiotic cement beads were inserted for 5 cases into bony defect and dead space after curettage and sequestrectomy, and pus discharge was stopped after 8.8 weeks in average.
-
Citations
Citations to this article as recorded by- A Review of Domestic and International Clinical Research Trends on Pharmacopuncture Treatment for Fractures
Hea Sun Chun
Journal of Physiology & Pathology in Korean Medicine.2023; 37(6): 185. CrossRef
- A Review of Domestic and International Clinical Research Trends on Pharmacopuncture Treatment for Fractures
- 462 View
- 0 Download
- 1 Crossref

- Internal Bone Transport for Treatment of Infected Non-union of Long Bone
- Han Suk Ko, Byung Jik Kim, Young Lim, Jeong Gook Seo, Jin Ku Kim, Dong Hun Lee
- J Korean Soc Fract 1998;11(3):623-628. Published online July 31, 1998
- DOI: https://doi.org/10.12671/jksf.1998.11.3.623
-
 Abstract
Abstract
 PDF
PDF - Infected nonunion of long bone frequently accompanies with bone loss, because of the outcome of initial trauma or iatrogenic result from sequestra resection. In this study, infected and ununited long bone fracture was treated with internal bone transport technique which was first discribed by G.A. Ilizarov. There were eleven tibial and two femural nonunion. The mean number of admission was 2.8 times; mean number of operation was 8 times; mean duration of average healing index was 1.95 month/cm. All infections were cured and all nonunions were united. Functional result was excellent in 5 cases (of 13 cases), good in 5, fair in 2, and 1 had poor result. Many complication had been observed. All had infection of pin site and pain at least one time, 5 had stiff knee, 9 had stiff ankle, early consolidation(1), delay consolidation(3), tibiofibular synostosis(5), nerve injury(1), refracture after union(1), angular deformity over 5 degree(7), rotational deformity over 10 degree(2).
- 308 View
- 2 Download

- Postoperative Infection in the Closed Fractures of the Long Bone
- Hyoun Oh Cho, Kyoung Duck Kwak, Sung Do Cho, Bab Jae Lee, Il Jong Yang
- J Korean Soc Fract 1997;10(4):866-871. Published online October 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.4.866
-
 Abstract
Abstract
 PDF
PDF - Operative treatment for closed fractures of the long bone has many advantages including early restoration of function by stable fixation, but has untoward problems including postoperative infection. The authors reviewed 19 cases of postoperative infection for closed long bone fracture during the period from January, 1990 to December, 1995 and analyzed about clinical, radiologic, pathologic findings and found causes of infection. Most cases were associated with multiple fractures of major bones or injuries to the vital organs and delayed over 48 hours after injury to operation. Operation time was prolonged due to the simultaneous operations for multiple fractures and associated open fractures at the same time. Staphylococcus aureus was the most frequent offending organism. Irregular resorption of plate-bone interface with resultant gap between the plate and bone, on the radiographic follow up, may indicate postoperative infection.
- 298 View
- 0 Download

- The Treatment of Infected Fracture of Long Bones
- Hak Yeong Jeong, Seung Wook Yang, Young Cheol Shin, Jae Woong Shim
- J Korean Soc Fract 1995;8(3):678-687. Published online July 31, 1995
- DOI: https://doi.org/10.12671/jksf.1995.8.3.678
-
 Abstract
Abstract
 PDF
PDF - The increase in incidence and severity of open injury to bone and surrounding soft tisseues from vehicular and industrial accidents, and the aggressive surgical approach of open reduction and internal fixation of closed fractures contribute to a definite rise in acute wound infection in fracture management. The main objectives are twofold in the treatment of infected fractures, the first to diagnose infection early and the second to treat it effectively and to prevent it from spreading into bone. To solve these problems, we used some principles of treatment, those are meticulous debridement of infected tissue, management of soft tissue and bony defect and maintenance of fracture stability. From Jan. 1988 to Dec. 1993, we treated 23 infected fractures of long bone and the result were as follows. 1. The infected fractures were femur in 9 and tibia in 14 cases. 2. There were 14 open fractures and 9 closed fractures. 3. In closed fracture, the first infection sign was developed average 7.8 days after open reduction, and average 9 days after trauma in open fracture. 4. The most common causative organism was staphylococcus aureus. 5. Infection was controlled from 3 months to a year and 8 months. 6. The number of soft tissue and bone debridement was one to four times. 7. Bony union was achieved from 6 months to 2 years in tibia and 6 months to 2 years and 1 month in femur.
- 273 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


