Search
- Page Path
- HOME > Search
Review Articles
- Fracture-related infections: a comprehensive review of diagnosis and prevention
- HoeJeong Chung, Hoon-Sang Sohn
- J Musculoskelet Trauma 2025;38(2):86-95. Published online April 25, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00164
-
 Abstract
Abstract
 PDF
PDF - Fracture-related infections are challenging complications in orthopedic trauma that often require prolonged treatment and impose a significant healthcare burden. Accurate diagnosis and effective prevention strategies are essential for minimizing their occurrence. A recent international consensus has established standardized diagnostic criteria based on clinical, microbiological, radiological, and histopathological findings. Prevention is the top priority and involves a thorough preoperative risk assessment, along with glycemic control, nutritional optimization, and management of comorbidities, as well as intraoperative and postoperative measures such as appropriate antibiotic prophylaxis, surgical site antisepsis, and meticulous wound care. A multidisciplinary approach involving orthopedic surgeons, infectious disease specialists, and microbiologists is crucial for successfully reducing the burden of fracture-related infections.
-
Citations
Citations to this article as recorded by- Personalized Approaches to Diagnostic and Therapeutic Strategies in Periprosthetic Fracture-Related Infections (PFRIs): Case Series and Literature Review
Marianna Faggiani, Marco Zugnoni, Matteo Olivero, Salvatore Risitano, Giuseppe Malizia, Silvia Scabini, Marcello Capella, Stefano Artiaco, Simone Sanfilippo, Alessandro Massè
Journal of Personalized Medicine.2025; 15(12): 576. CrossRef - Pathogen-Specific Risk for Iterative Surgical Debridement in Orthopedic Infections: A Prospective Multicohort Analysis
Flamur Zendeli, Anna Jędrusik, Raymond O. Schaefer, David Albrecht, Michael Betz, Felix W. A. Waibel, Tanja Gröber, Nathalie Kühne, Sören Könneker, İlker Uçkay
Journal of Clinical Medicine.2025; 14(24): 8750. CrossRef
- Personalized Approaches to Diagnostic and Therapeutic Strategies in Periprosthetic Fracture-Related Infections (PFRIs): Case Series and Literature Review
- 5,978 View
- 219 Download
- 2 Crossref

- Systematic Diagnosis and Treatment Principles for Acute Fracture-Related Infections
- Jeong-Seok Choi, Jun-Hyeok Kwon, Seong-Hyun Kang, Yun-Ki Ryu, Won-Seok Choi, Jong-Keon Oh, Jae-Woo Cho
- J Korean Fract Soc 2023;36(4):148-161. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.148
-
 Abstract
Abstract
 PDF
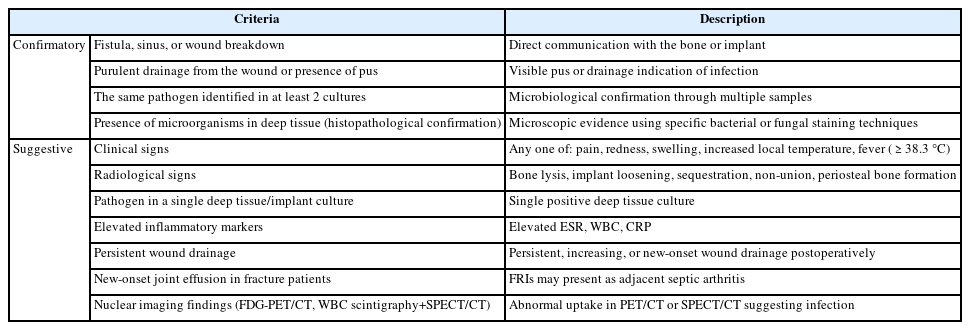
PDF - Acute fracture-related infection (FRI) is a common and serious complication of fracture treatment. The clinical symptoms of the patient and the results of the serological, radiological, and histopathologi-cal examinations can be divided into ‘Confirmatory’ criteria and ‘Suggestive’ criteria, allowing for the diagnosis of FRI. Treatment principles can be broadly categorized into (1) the DAIR (Debridement, Antimicrobial therapy, Implant Retention) method and (2) the staged reconstruction method. The choice of treatment depends on factors such as the time elapsed after infection, stability of the internal fixation device, reduction status, host physiology, and virulence of the pathogens. Thorough surgical debridement and irrigation, ensuring stability at the fracture site, reconstruction of bone defects, and appropriate soft tissue coverage, along with antibiotic therapy, are essential to suppress or eradicate the infection. The restoration of limb function should be promoted through proper soft tissue coverage and bone union at the fracture site.
- 708 View
- 15 Download

Case Report
- Concurrent Posterolateral Corner Injury Associated with a Schatzker Type 2 Tibial Plateau Fracture: A Case Report
- Jae Cheon Sim, Choong Won Jung, Tae Seok Nam
- J Korean Fract Soc 2020;33(1):27-31. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.27
-
 Abstract
Abstract
 PDF
PDF - Isolated posterolateral corner (PLC) injury associated with a Schatzker type 2 fracture is a very rare combination of injuries. A male who was driving a motor vehicle was injured after a collision accident. The plain radiographs and computed tomography scans of the knee showed a Schatzker type 2 fracture of the tibial plateau, mostly in the anterolateral portion of tibial plateau, and an avulsion fragment on the fibular tip. Magnetic resonance imaging showed no injury to cruciate ligaments, medial collateral ligament, or any meniscal injury. We performed an open reduction operation and internal fixation for treating the fracture. Six months later, he complained of instability. At 11 months later after initial operation, we performed the second operation for stabilizing the PLC. We present here a rare case of an isolated PLC injury associated with a Schatzker type 2 fracture. We discuss the mechanism of injury and review similar cases.
- 801 View
- 3 Download

Original Articles
- Ankle Fracture Associated with Tibia Shaft Fractures
- Ji Wan Kim, Hong Joon Choi, Dong Hyun Lee, Young Chang Kim
- J Korean Fract Soc 2014;27(2):136-143. Published online April 30, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.2.136
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the incidence of ankle injury in ipsilateral tibial shaft fractures and to assess the risk factors for ankle injury associated with tibial shaft fractures.
MATERIALS AND METHODS
Sixty patients with tibial shaft fractures were enrolled in this retrospective study. The incidence and characteristics of ankle injury were evaluated, and fracture classification, fracture site, and fracture pattern of the tibial shaft fractures were analyzed for assessment of the risk factors for ankle injury combined with tibial shaft fractures.
RESULTS
Ankle injury occurred in 20 cases (33%). There were four cases of lateral malleolar fracture, four cases of posterior malleolar fracture, two cases of distal tibiofibular ligament avulsion fracture, and 10 cases of complex injury. Fourteen cases (70%) of 20 cases of ankle injury were diagnosed from x-ray films, and the other six cases were recognized in ankle computed tomography (CT). Ankle injury occurred in 45.1% of distal tibial shaft fractures and found in 41.4% of A type, but there was no statistical significance. Ankle injury was observed in 54% of cases of spiral pattern of tibial shaft fracture and the incidence was statistically higher than 19% of cases of non-spiral pattern tibial shaft fracture.
CONCLUSION
Ankle injury was observed in 33% of tibial shaft fractures; however, only 70% could be diagnosed by x-ray. Ankle injury occurred frequently in cases of spiral pattern of tibial shaft fracture, and evaluation of ankle injury with CT is recommended in these cases. -
Citations
Citations to this article as recorded by- Usefulness of Computed Tomography on Distal Tibia Intra-Articular Fracture Associated with Spiral Tibia Shaft Fracture
Seong-Eun Byun, Sang-June Lee, Uk Kim, Young Rak Choi, Soo-Hong Han, Byong-Guk Kim
Journal of the Korean Fracture Society.2016; 29(2): 114. CrossRef
- Usefulness of Computed Tomography on Distal Tibia Intra-Articular Fracture Associated with Spiral Tibia Shaft Fracture
- 697 View
- 5 Download
- 1 Crossref

- Diagnosis and Treatment of the Lateral Condylar Fracture of Humerus Traversing the Capitulum in Children
- Kwang Soo Song, Dong Hwa Woo
- J Korean Soc Fract 2000;13(1):166-171. Published online January 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.1.166
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
: To emphasize the importance of the oblique view of elbow in diagnosis of the lateral condylar fracture traversing the capitulum to propose an appropriate treatment reducing the complication.
MATERIALS AND METHODS
: We analyzed eight cases of lateral condylar fracture traversing the capitulum among the 192 cases of lateral condylar fracture with preoperative complete roentgenogram and medical record from April, 1992 to September, 1998.
RESULTS
: In seven cases, it was possible to diagnose as lateral condylar fracture of humerus in initial anteroposterior and lateral view, but it had a difficulty to decide whether fracture line traversing the capitulum. The oblique view provided accurate fracture line to diagnose. One case was diagnosed fracture line traversing the capitulum in lateral view. There was no considerable complications at 18 months follow up in average, except one case with malunion that was transferred form other hospital after operation.
CONCLUSION
: To make a diagnosis of the lateral condylar fracture traversing capitulum, the oblique view is helpful. We considered that internal fixation is require because the fragment can be displaced progressively.
- 370 View
- 0 Download

- The Clinical Signifiance of Bone Scan in Fracture Diagnosis
- Joon Young Kim, Young An Choi, Byoung Kuk Noh, Bo Seuk Kong
- J Korean Soc Fract 1988;1(1):102-108. Published online November 30, 1988
- DOI: https://doi.org/10.12671/jksf.1988.1.1.102
-
 Abstract
Abstract
 PDF
PDF - Most of fracture is easily diagnosed by simple roentgenological studies. However, certain fracture, especially rib and spine are not well definable in scout film desite the suspicious clinical findings. For these cases, we can confirm the fracture by use of whole body bone scan, CT scan and M.R.I We performed Tc bone scan and found out 27 cases of the definite fracture that were considered contusion at initial roentgenological studies from March 1987 to April 1988. We present the following results: 1. In general, the incidence of positive findings on bone scan is higher by the 7 days after trauma. 2. The bone scan is especially valuable for detection of occult rib and spine fracture. 3. It is necessary to perform the interval bone scan in the case of clinically suspicious fracture even if negative initial bone scan.
-
Citations
Citations to this article as recorded by- The Comparison of Bone Scan and MRI in Osteoporotic Compression Fractures
Jung-Hoon Kim, Jong-In Kim, Bo-Hoon Jang, Jung-Gook Seo, Jin-Hwan Kim
Asian Spine Journal.2010; 4(2): 89. CrossRef
- The Comparison of Bone Scan and MRI in Osteoporotic Compression Fractures
- 508 View
- 0 Download
- 1 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


