Search
- Page Path
- HOME > Search
Review Article
- Innovative applications of artificial intelligence in orthopedics focusing on fracture and trauma treatment: a narrative review
- Chul-Ho Kim, Ji Wan Kim
- J Musculoskelet Trauma 2025;38(4):178-185. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00283
-
 Abstract
Abstract
 PDF
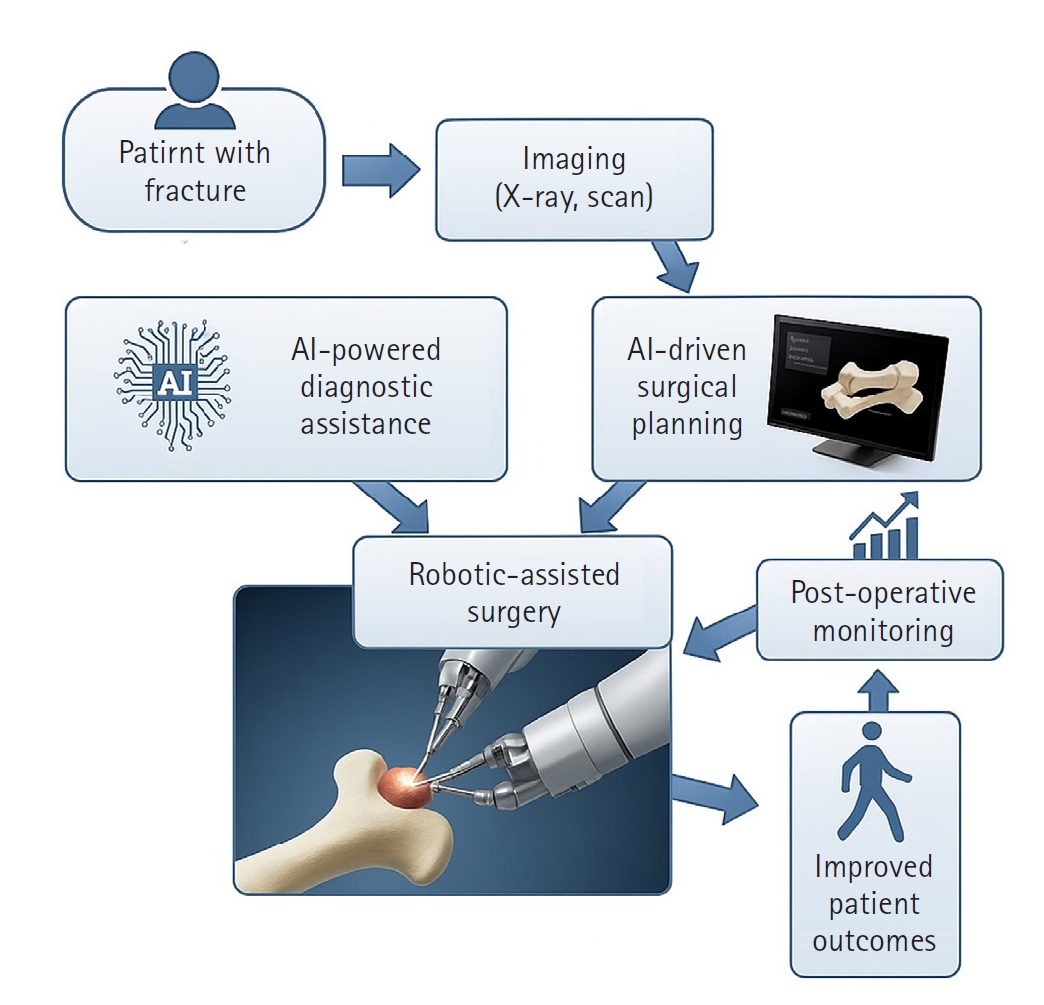
PDF - Artificial intelligence (AI) is bringing about transformative changes in orthopedic surgery, with its potential being particularly prominent in the field of fracture and trauma treatment. This review explores the current applications and future prospects of AI-driven surgical planning and simulation, robot and image-based navigation surgery, and image-assisted diagnostic technologies. Robotic assistance in orthopedic surgery, which was initially applied to improve accuracy in component implantation for knee and hip arthroplasty and to achieve high precision in spinal screw placement, has recently expanded its use to include accurate, minimally invasive reduction of pelvic fractures. In diagnostics, AI aids in the early prediction and classification of ambiguous fractures in various anatomical regions—for example, detecting shoulder or hip fractures, identifying incomplete atypical femur fractures, and classifying femoral neck fractures—through X-ray image analysis. This improves diagnostic accuracy and reduces medical costs. However, significant challenges remain, including high initial costs, steep learning curves, a lack of long-term studies, data bias, and ethical concerns. Continued research, interdisciplinary collaboration, and policy support are crucial for the widespread adoption of these technologies.
- 543 View
- 7 Download

Original Articles
- Risk factors of surgical complications after use of the femoral neck system: a random forest analysis
- Chul-Ho Kim, Hyun-Chul Shon, Han Soul Kim, Ji Wan Kim, Eic Ju Lim
- J Musculoskelet Trauma 2025;38(3):160-167. Published online July 23, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00157
-
 Abstract
Abstract
 PDF
PDF - Background
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
Methods
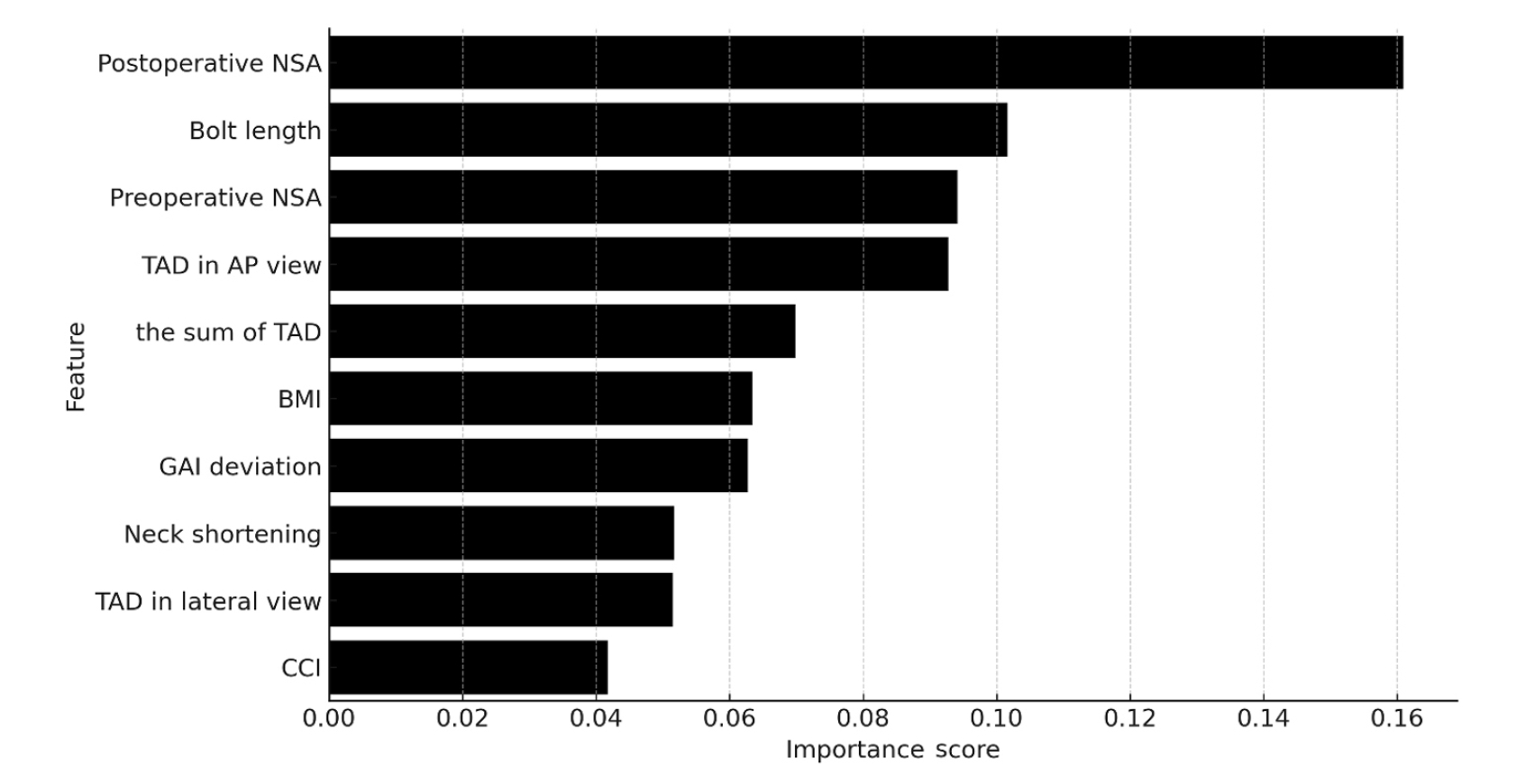
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
Results
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery. Level of Evidence: III.
- 844 View
- 37 Download

- Lateral marginal fractures of the patella and patellofemoral pain
- Jae-Ang Sim, Chul-Ho Kim, Ji Wan Kim
- J Musculoskelet Trauma 2025;38(3):152-159. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00171
-
 Abstract
Abstract
 PDF
PDF - Background
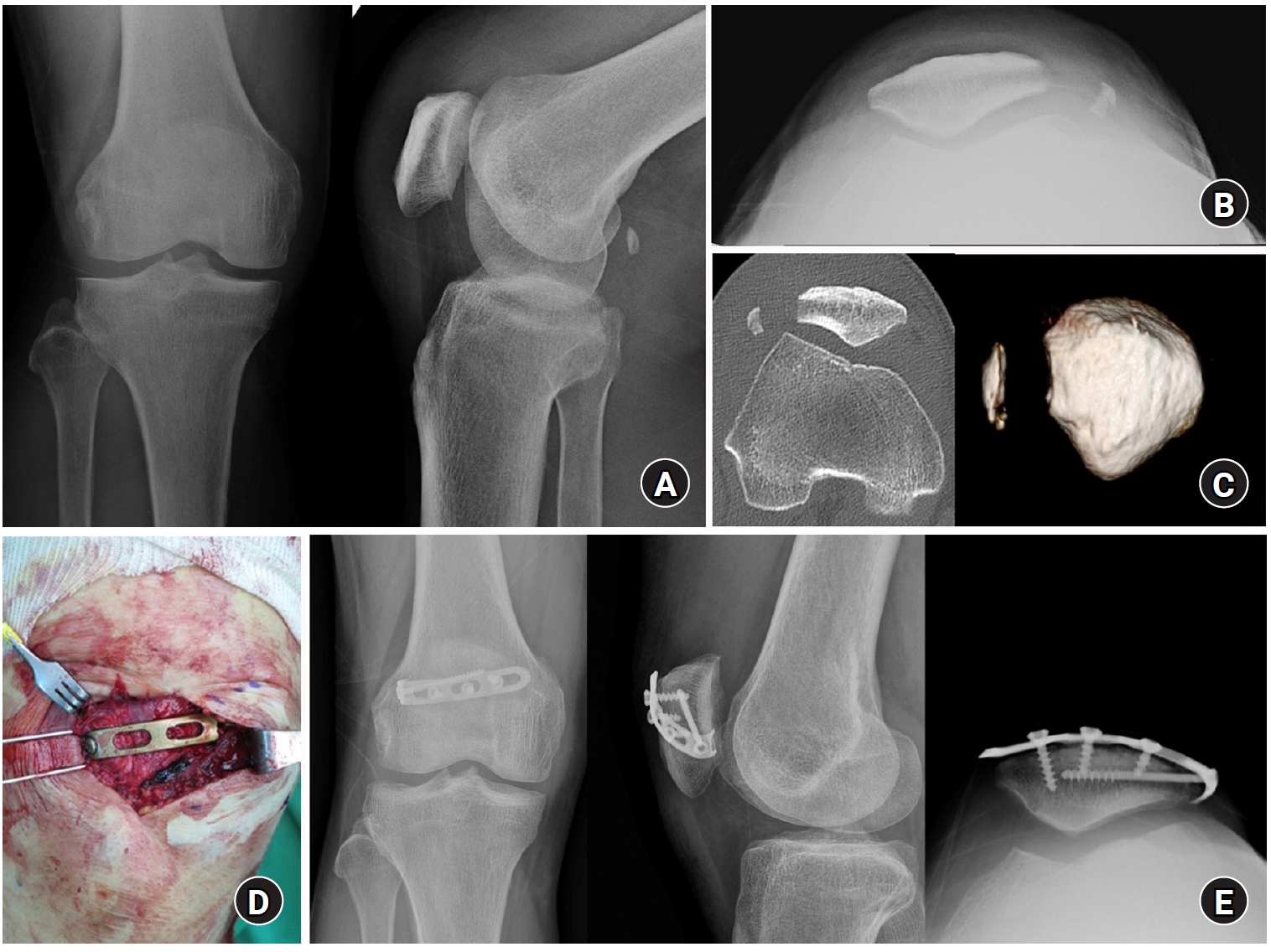
This study investigated the characteristics of lateral marginal fractures of the patella and evaluated the clinical outcomes.
Methods
We retrospectively reviewed all patients with lateral marginal fractures of the patella, defined as a vertical fracture line within 15 mm of the lateral patellar border, from 2008 to 2020. In total, 41 patients were included. Patient characteristics, radiologic findings, and clinical outcomes, including the Lysholm score at 1 year postoperation, were evaluated.
Results
The injury mechanisms were direct in 34 cases and indirect in seven. Furthermore, 85% of patients had a skyline view of the patella at the initial visit, and one medial subluxation of the patella was found. Forty of the 41 patients underwent surgery. Anatomical and nonanatomical (>1-mm displacement or excision) reductions were carried out in 36 cases (88%) and five cases (12%), respectively. The average Lysholm score was 89.1 (range, 67–99). The nonanatomical reduction group had a poorer functional score (79.8 vs. 90.4; P=0.010). Lateral patellar compression syndrome occurred in two patients with nonanatomical reduction.
Conclusions
Lateral marginal fractures of the patella affected patellofemoral stability. Anatomical reduction showed good functional outcomes, while nonanatomical reduction was associated with patellofemoral stability and pain. Therefore, surgeons should perform anatomical reduction with any appropriate fixation method. Level of Evidence: IV
- 884 View
- 21 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 First
First Prev
Prev


