-
Comparative results of the femoral neck system versus the dynamic hip screw for stable femoral neck fractures in older adults in Korea: a retrospective cohort study
-
Byung-Chan Choi, Byung-Woo Min, Kyung-Jae Lee, Jun-Sik Hong
-
J Musculoskelet Trauma 2025;38(4):203-211. Published online October 24, 2025
-
DOI: https://doi.org/10.12671/jmt.2025.00276
-
-
 Abstract Abstract
 PDF PDF
- Background
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
Methods
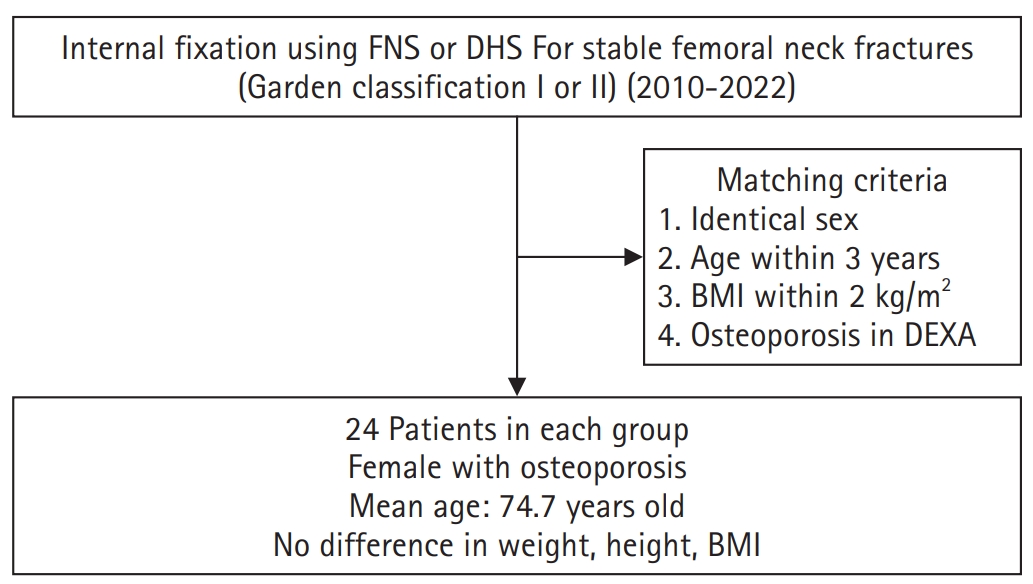
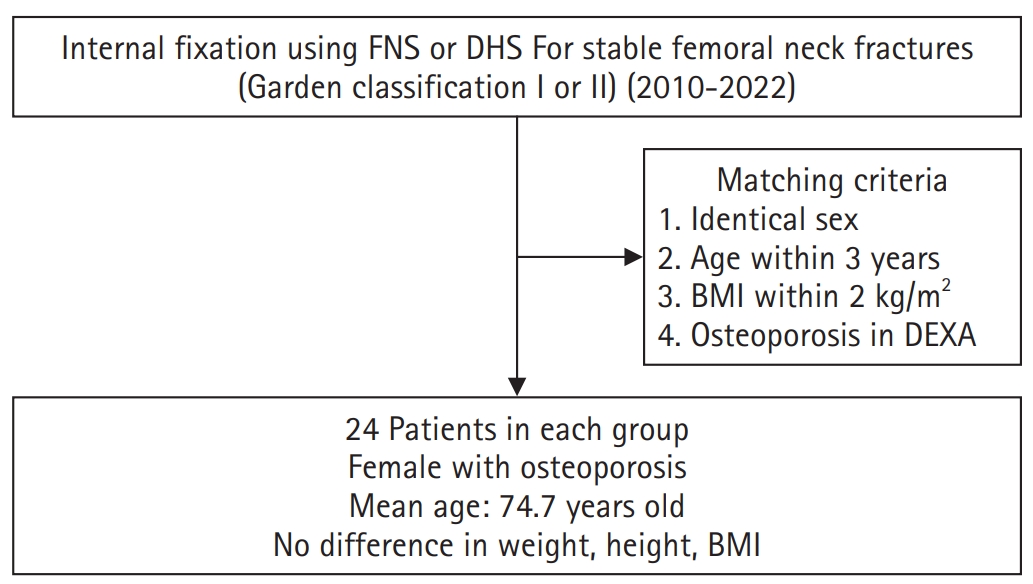
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results.
Level of evidence: IV.
|