Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 23(2); 2010 > Article
-
Original Article
- Surgical Treatment of Pathologic Humeral Fracture
- Ho Jung Kang, M.D., Byoung Yoon Hwang, M.D., Jae Jeong Lee, M.D., Kyu Ho Shin, M.D., Soo Bong Hahn, M.D., Sung Jae Kim, M.D.
-
Journal of the Korean Fracture Society 2010;23(2):187-193.
DOI: https://doi.org/10.12671/jkfs.2010.23.2.187
Published online: April 30, 2010
Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea.
- Address reprint requests to: Byoung Yoon Hwang, M.D. Department of Orthopaedic Surgery, Yonsei University College of Medicine, 250, Seongsan-ro, Seodaemun-gu, Seoul 120-752, Korea. Tel: 82-2-2228-5679, Fax: 82-2-361-1139, sogood95@yuhs.ac
• Received: August 24, 2009 • Revised: December 15, 2009 • Accepted: January 12, 2010
Copyright © 2010 The Korean Fracture Society
- 522 Views
- 3 Download
- 2 Crossref
Abstract
-
Purpose
- To evaluate and analyze the radiographic and clinical outcomes after the surgical treatments of pathologic humeral fractures.
-
Materials and Methods
- From October 1993 to September 2007, a retrospective investigation was conducted with a total of 13 patients who underwent operations for pathologic humeral fractures. The methods of surgical treatment were as follows-four cases of open reduction and internal fixation; eight cases of closed reduction and internal fixation with intramedullary nailing; and one of radical excision and hemiarthroplasty.
-
Results
- Of nine patients with metastatic bone lesions, three were diagnosed with primary cancer after the incidence of pathologic humeral fracture. The mean period between the diagnosis of primary cancer and pathologic fracture in the latter six cases was 36.7 (2~144) months and the mean survival period after the surgical treatments was 22.8 (12~35) weeks in all patients with bone metastasis. Fracture unions were noted in all four cases of primary humeral bone lesion but none in metastatic cases. Pain relief and functional recovery were noted in eleven patients of this study.
-
Conclusion
- Satisfactory clinical outcomes with sustained pain relief and functional recovery were observed after the surgical treatments of pathologic humeral fracture. Benign bone lesions require more active and early treatments in order to facilitate the functional recovery of upper extremities and fracture union. With pathologic humeral fractures originated from metastasis, palliative treatments were preferred to fracture union method for planning long-term pain relief and functional recovery.
- 1. Bae SW, Kim WJ, Song BY, Choi NH, Lee JH. Postoperative functional assessments in adult humerus shaft fractures comparison among plates and screws, intramedullary nail and external fixatior. J Korean Soc Fract, 2001;14:228-235.Article
- 2. Brage ME, Simon MA. Evaluation, prognosis, and medical treatment considerations of metastatic bone tumors. Orthopedics, 1992;15:589-596.Article
- 3. Carlin BI, Andriole GL. The natural history, skeletal complications, and management of bone metastases in patients with prostate carcinoma. Cancer, 2000;88:12 Suppl. 2989-2994.Article
- 4. Chao EYS, Sim FH, Shives TC, Pritchard DJ. Kim AH. Management of pathological fracture. In: Diagnosis and management of metastatic bone disease. A multidisciplinary approach, 1988;New York, Raven Press. 283-290.
- 5. Chin HC, Frassica FJ, Hein TJ, et al. Metastatic diaphyseal fractures of the shaft of the humerus. The structural strength evaluation of a new method of treatment with a segmental defect prosthesis. Clin Orthop Relat Res, 1989;(248):231-239.
- 6. Damron TA, Sim FH, Shives TC, An KN, Rock MG, Pritchard DJ. Intercalary spacers in the treatment of segmentally destructive diaphyseal humeral lesions in disseminated malignancies. Clin Orthop Relat Res, 1996;(324):233-243.Article
- 7. Dijkstra S, Stapert J, Boxma H, Wiggers T. Treatment of pathological fractures of the humeral shaft due to bone metastases: a comparison of intramedullary locking nail and plate osteosynthesis with adjunctive bone cement. Eur J Surg Oncol, 1996;22:621-626.Article
- 8. Dijstra S, Wiggers T, van Geel BN, Boxma H. Impending and actual pathological fractures in patients with bone metastases of the long bones. A retrospective study of 233 surgically treated fractures. Eur J Surg, 1994;160:535-542.
- 9. Flemming JE, Beals RK. Pathologic fracture of the humerus. Clin Orthop Relat Res, 1986;(203):258-260.Article
- 10. Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res, 2003;415 Suppl. S212-S218.Article
- 11. Friedl W. Indication, management and results of surgical therapy for pathological fractures in patients with bone metastases. Eur J Surg Oncol, 1990;16:380-396.
- 12. Galasko CSB. Skeletal metastases, 1986;London, Butterworth.
- 13. Habermann ET, Lopez RA. Metastatic disease of bone and treatment of pathological fractures. Orthop Clin North Am, 1989;20:469-486.
- 14. Harrington KD, Sim FH, Enis JE, Johnston JO, Dick HM, Gristina AG. Methylmethacrylate as an adjunct in internal fixation of pathologic fractures. Experience with three hundred and seventyfive cases. J Bone Joint Surg Am, 1976;58:1047-1055.
- 15. Jacobson AF, Shapiro CL, Van den Abbeele AD, Kaplan WD. Prognostic significance of the number of bone scan abnormalities at the time of initial bone metastatic recurrence in breast carcinoma. Cancer, 2001;91:17-24.Article
- 16. Janjan N. Bone metastases: approaches to management. Semin Oncol, 2001;28:4 Suppl 11. 28-34.Article
- 17. Kim JI, Yoo CI, Suh JT, Suh KT, Kim HT, Moon NH. Surgical treatment and prognostic factor for metastatic bone tumor. J Korean Orthop Assoc, 2008;43:438-444.Article
- 18. Kollender Y, Bickels J, Price WM. Metastatic renal cell carcinoma of bone: indications and technique of surgical intervention. J Urol, 2000;164:1505-1508.Article
- 19. Lancaster JM, Koman LA, Gristina AG, et al. Pathologic fractures of the humerus. South Med J, 1988;81:52-55.Article
- 20. Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res, 1989;(249):256-264.Article
- 21. Park SR, Lee TJ, Kim RS, Moon KH, You DS. Result of interlocking intramedullary nailing for humeral shaft fracture evaluation of post-operative shoulder function. J Korean Fract Soc, 2007;20:166-171.Article
- 22. Patel B, DeGroot H 3rd. Evaluation of the risk of pathologic fractures secondary to metastatic bone disease. Orthopedics, 2001;24:612-617.Article
- 23. Redmond BJ, Biermann JS, Blasier RB. Interlocking intramedullary nailing of pathological fractures of the shaft of the humerus. J Bone Joint Surg Am, 1996;78:891-896.Article
- 24. Sim FH, Frassica FJ, Chao EY. Orthopaedic management using new devices and prostheses. Clin Orthop Relat Res, 1995;312:160-172.
- 25. Sim FH, Prichard DJ. Metastatic disease in the upper extremity. Clin Orthop Relat Res, 1982;(169):83-94.Article
- 26. Townsend PW, Rosenthal HG, Smalley SR, Cozad SC, Hassanein RE. Impact of postoperative radiation therapy and other perioperative factors on outcome after orthopedic stabilization of impending or pathologic fractures due to metastatic disease. J Clin Oncol, 1994;12:2345-2350.
- 27. Vail TP, Harrelson JM. Treatment of pathologic fractures of the humerus. Clin Orthop Relat Res, 1991;(268):197-202.
- 28. van der Hulst RR, van den Wildenberg FA, Vroemen JP, Greve JW. Intramedullary nailing of (impending) pathologic fractures. J Trauma, 1994;36:211-215.Article
REFERENCES
Fig. 1
(A) A 51-year-old female had proximal humeral fracture from a slip down injury. Possible diagnosis was simple bone cyst, enchondroma, giant cell tumor or aneurismal bone cyst.
(B) She was treated with closed reduction and intramedullary nailing.
(C) After the surgical treatment, biopsy of fracture site was confirmed as giant cell tumor. One week after the primary operation, curettage and autoiliac bone graft were performed (Black arrow is an autologous iliac bone block).
(D) The bone union was gained at 13 months after operation.
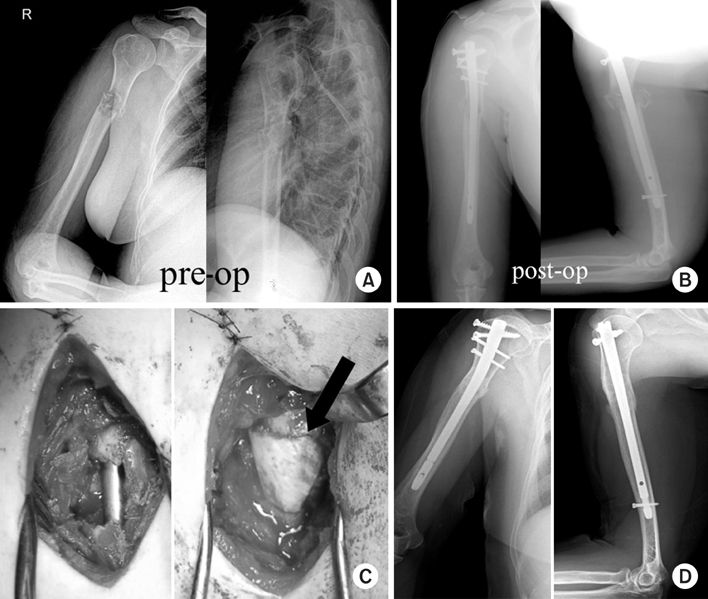
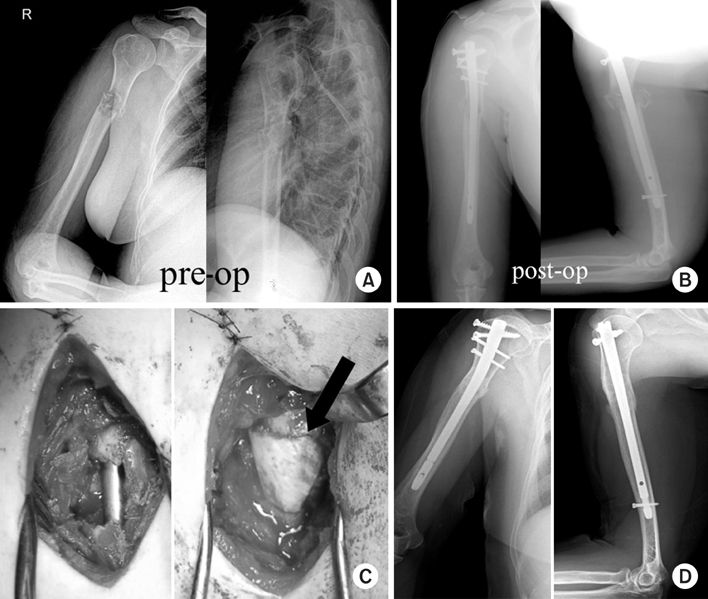
Fig. 2
(A) A 55-year-old male, with humerus shaft fracture from car accident 3 years ago, initially had an internal fixation, but a follow-up bone graft was carried out due to the continuous mal-union.
(B) After his third operation with preoperative evaluation of lung mass, biopsy of fracture site was confirmed as pathologic fracture originated from lung cancer (White arrow is a lung mass).
(C) At 5 months after closed reduction and IM nailing with bone graft, we found persistent non-union of humeral shaft. He died at 26 weeks after operation.
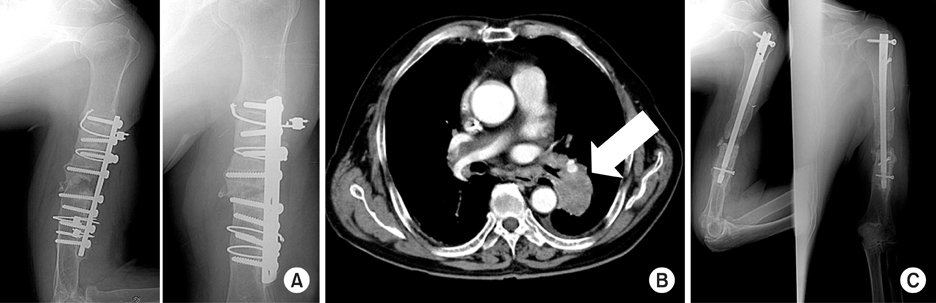
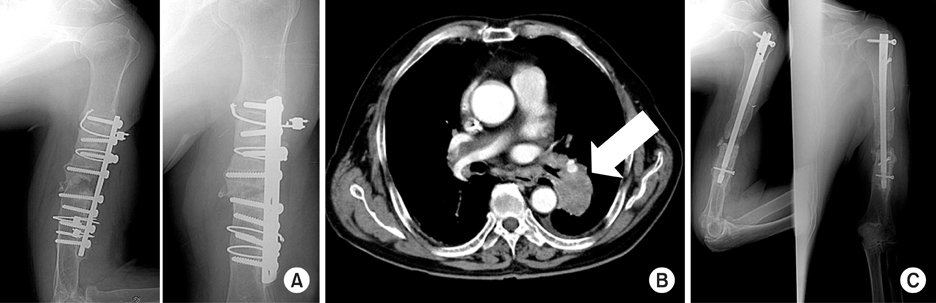
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- The application of a dual-lead locking screw could enhance the reduction and fixation stability of the proximal humerus fractures: a biomechanical evaluation
Eunju Lee, Hyeon Jang Jeong, Yeon Soo Lee, Joo Han Oh
Frontiers in Surgery.2024;[Epub] CrossRef - Therapeutic Approach to Humeral Pathologic Fracture Caused by Benign Bone Tumor
Jeung Il Kim, Um Ji Kim, Nam Hoon Moon, Hui Taek Kim, Tae Young Ahn, In Sook Lee, You Seon Song, Kyung Un Choi
Journal of the Korean Orthopaedic Association.2016; 51(6): 509. CrossRef
Surgical Treatment of Pathologic Humeral Fracture
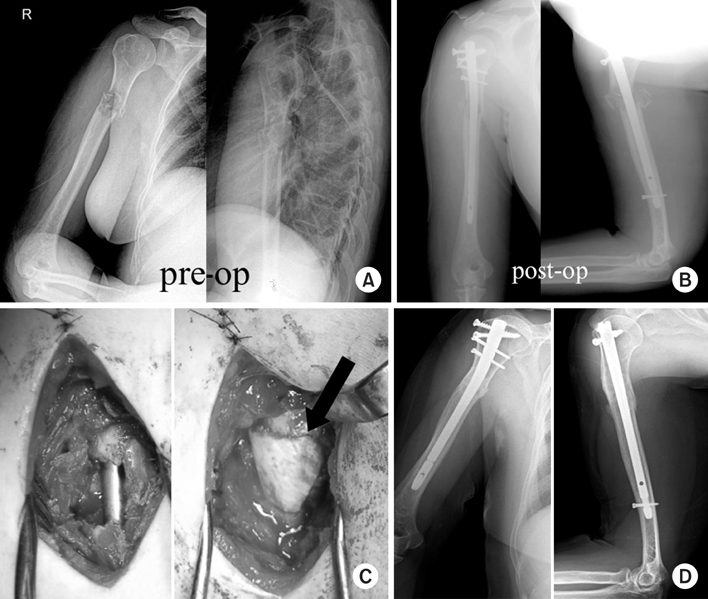
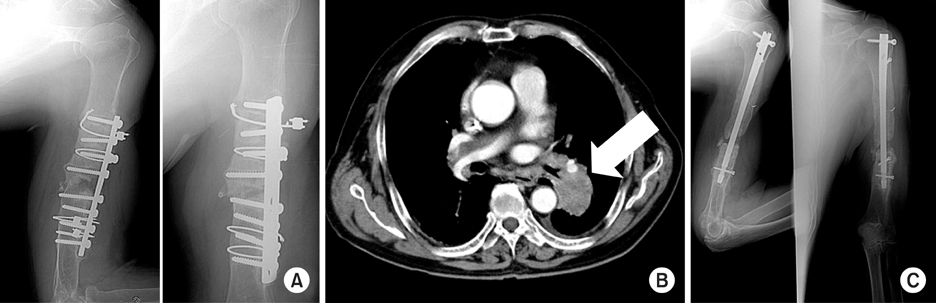
Fig. 1
(A) A 51-year-old female had proximal humeral fracture from a slip down injury. Possible diagnosis was simple bone cyst, enchondroma, giant cell tumor or aneurismal bone cyst.
(B) She was treated with closed reduction and intramedullary nailing.
(C) After the surgical treatment, biopsy of fracture site was confirmed as giant cell tumor. One week after the primary operation, curettage and autoiliac bone graft were performed (Black arrow is an autologous iliac bone block).
(D) The bone union was gained at 13 months after operation.
Fig. 2
(A) A 55-year-old male, with humerus shaft fracture from car accident 3 years ago, initially had an internal fixation, but a follow-up bone graft was carried out due to the continuous mal-union.
(B) After his third operation with preoperative evaluation of lung mass, biopsy of fracture site was confirmed as pathologic fracture originated from lung cancer (White arrow is a lung mass).
(C) At 5 months after closed reduction and IM nailing with bone graft, we found persistent non-union of humeral shaft. He died at 26 weeks after operation.
Fig. 1
Fig. 2
Surgical Treatment of Pathologic Humeral Fracture
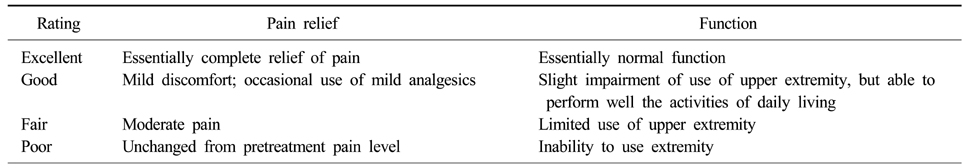
Modification of the rating system of Perez et al.
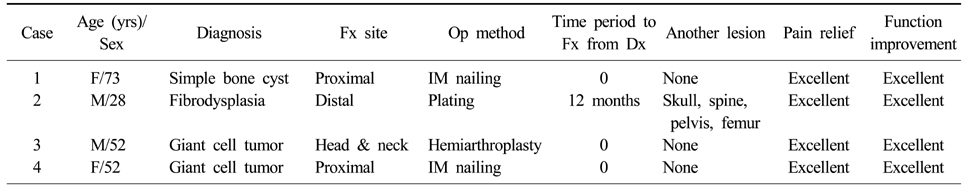
Data of 4 cases with benign humeral lesion
Fx: Fracture, Dx: Diagnosis, IM: Intramedullary, Op: Operation.
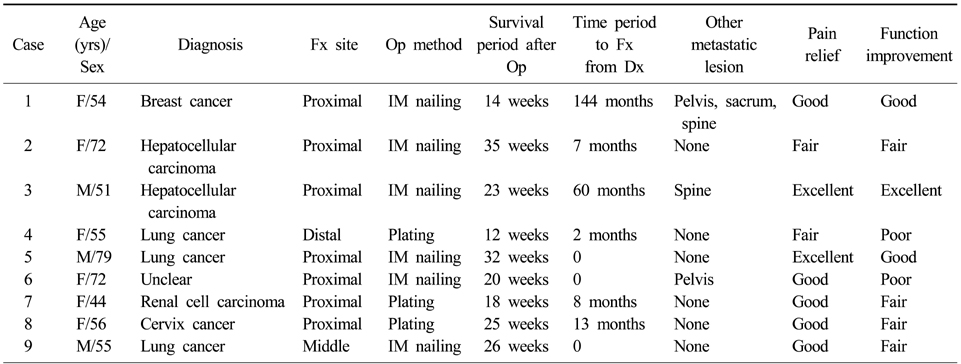
Data of 9 cases with metastatic humeral lesion
Fx: Fracture, Dx: Diagnosis, IM: Intramedullary, Op: Operation.
Table 1
Modification of the rating system of Perez et al.
Table 2
Data of 4 cases with benign humeral lesion
Fx: Fracture, Dx: Diagnosis, IM: Intramedullary, Op: Operation.
Table 3
Data of 9 cases with metastatic humeral lesion
Fx: Fracture, Dx: Diagnosis, IM: Intramedullary, Op: Operation.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

