Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 36(4); 2023 > Article
- Original Article The Efficiency of Radiation Shielding Sheet to Reduce Radiation Exposure during C-arm Fluoroscopy
- Hosang Jeon, Won Chul Shin, Hee Yun Seol, Yongkan Ki, Kyeong Baek Kim, Ki Seok Choo, Sang Don Lee, Suk-Woong Kang
-
Journal of Musculoskeletal Trauma 2023;36(4):111-117.
DOI: https://doi.org/10.12671/jkfs.2023.36.4.111
Published online: October 31, 2023
2Departments of Orthopedics, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
3Departments of Internal Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
4Departments of Radiology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
5Departments of Urology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- 2,849 Views
- 52 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
This study evaluates the radiation shielding performance of a new lead-free tungsten-based sheet to reduce the radiation exposure of operators and patients under C-arm fluoroscopy.
Materials and Methods
A non-lead radiation shielding sheet (ROO201128; Pentas, Korea) was fabri-cated using tungsten and bismuth. The dose measurements were conducted using a C-arm fluoroscopy machine at 64 kVp and 1.5 mA, assuming two possible scenarios according to the position of the sheet. In each scenario, measurements were conducted at three distances (30, 60, and 90 cm) away from the beam center and in three directions (cephal, caudal, and operator’s direction).
Results
In the area within a radius of 60 cm from the beam center, the measured doses were reduced by 66.3% on mean, and the doses measured at distances more than 60 cm were less than 0.1 mSv/h in both scenarios. The most beneficial utilization of the lead-free shielding sheet was verified during C-arm fluoroscopy by placing the sheet on the X-ray tube. The operator’s radiation exposure was reduced by 56.6% when the sheet was placed under the phantom, and by 81.0% when the sheet was placed on the X-ray tube.
Conclusion
The use of lead-free radiation shielding sheets under C-arm fluoroscopy was effective in reducing radiation exposure, and the most beneficial scenario in which the sheet can be utilized was verified when the sheet was placed on the X-ray tube.
Published online Oct 25, 2023.
https://doi.org/10.12671/jkfs.2023.36.4.111
 , Ph.D.,
Won Chul Shin
, Ph.D.,
Won Chul Shin , M.D., Ph.D.,*
Hee Yun Seol
, M.D., Ph.D.,*
Hee Yun Seol , M.D.,†
Yongkan Ki
, M.D.,†
Yongkan Ki , M.D.,
Kyeong Baek Kim
, M.D.,
Kyeong Baek Kim , M.D.,*
Ki Seok Choo
, M.D.,*
Ki Seok Choo , M.D., Ph.D.,‡
Sang Don Lee
, M.D., Ph.D.,‡
Sang Don Lee , M.D., Ph.D.,§
and Suk-Woong Kang
, M.D., Ph.D.,§
and Suk-Woong Kang , M.D.*
, M.D.*
Abstract
Purpose
This study evaluates the radiation shielding performance of a new lead-free tungsten-based sheet to reduce the radiation exposure of operators and patients under C-arm fluoroscopy.
Materials and Methods
A non-lead radiation shielding sheet (ROO201128; Pentas, Korea) was fabricated using tungsten and bismuth. The dose measurements were conducted using a C-arm fluoroscopy machine at 64 kVp and 1.5 mA, assuming two possible scenarios according to the position of the sheet. In each scenario, measurements were conducted at three distances (30, 60, and 90 cm) away from the beam center and in three directions (cephal, caudal, and operator’s direction).
Results
In the area within a radius of 60 cm from the beam center, the measured doses were reduced by 66.3% on mean, and the doses measured at distances more than 60 cm were less than 0.1 mSv/h in both scenarios. The most beneficial utilization of the lead-free shielding sheet was verified during C-arm fluoroscopy by placing the sheet on the X-ray tube. The operator’s radiation exposure was reduced by 56.6% when the sheet was placed under the phantom, and by 81.0% when the sheet was placed on the X-ray tube.
Conclusion
The use of lead-free radiation shielding sheets under C-arm fluoroscopy was effective in reducing radiation exposure, and the most beneficial scenario in which the sheet can be utilized was verified when the sheet was placed on the X-ray tube.
초록
목적
본 연구의 목적은 C-arm 투시술 중 술자와 환자의 방사선 피폭을 줄이기 위한 새로운 무연, 텅스텐 기반 시트의 성능을 평가하고자 하였다.
대상 및 방법
비납형 방사선 차폐 시트(ROO201128; Pentas, Korea)는 텅스텐과 비스무트를 사용하여 제작되었다. 선량 측정은 시트의 위치에 따라 두 가지 가능한 시나리오를 가정하여 64 kVp 및 1.5 mA에서 C-arm 투시 기계를 사용하여 수행하였다. 각 시나리오에서 빔 중심에서 3개의 거리(30, 60, 90 cm)와 3개의 방향(머리쪽, 꼬리쪽, 술자 방향)에서 측정하였다.
결과
빔 센터에서 반경 60 cm 이내의 영역에서 측정된 선량은 평균 66.3% 감소했으며, 60 cm 이상의 거리에서 측정된 선량은 두 시나리오 모두에서 0.1 mSv/h 미만이었다. X선 튜브에 시트를 올려 C-arm 투시를 함으로써 무연 차폐 시트를 가장 유용하게 사용할 수 있었다. X선 튜브에 시트를 올려놓을 때와 phantom 모델 아래에 위치시켰을 때 술자의 방사선 노출은 각각 56.6%, 81.0% 감소했다.
결론
C-arm 형광 투시 시 무연 차폐 시트를 사용하는 것은 방사선 피폭을 줄이는 데 효과적이었으며, 시트를 X선 튜브 위에 올려놓았을 때 가장 효과적이었다.
Introduction
In the last century, radiation-based devices for diagnosis and surgery were developed not only in the field of orthopedics but also in various medical fields. In particular, the development of fluoroscopy had a great impact on the advancement of intraoperative orthopedic surgery or orthopedic practice and resulted in reduced patient morbidity and length of a patient’s hospital stay.1)
However, the development of these radiation-based devices causes a large amount of radiation exposure to medical workers and patients. According to a 2006 report by the National Commission on Radiation Protection and Measurement, the per capita radiation dose in the United States increased from 3.6 mSv in the early 1980s to 6.2 mSv in 2006 due to the increased use of CT.2) The use of fluoroscopy has also increased with the development of minimal invasive procedures, resulting in excessive radiation exposure.3,4) Chou et al.5) investigated cancer prevalence among female orthopedic, urological, and plastic surgeons in the United States. In the study, female orthopedic surgeons had a higher-than-expected prevalence of cancers that may or may not be due to occupational exposure to ionizing radiation. Specifically, it reported that breast cancer was 2.5 times more common among female orthopedic surgeons using fluoroscopy.5)
In medical radiation exposure, orthopedic surgeons do not experience serious organ damage from radiation exceeding its thresholds. However, ionizing radiation is accumulated for a long period of time and has the effect of causing genetic mutations or various cancers.6,7) Although these stochastic effects are not related to radiation dose, but to higher dose accumulation increasing the probability of these effects occurring. That is why the as low as reasonably achievable (ALARA) principle has been emphasized.8) One study reported a higher incidence of cancer among orthopedic surgeons.9) In particular, there is a high risk of damage to radiosensitive organs such as the thyroid gland, eye, and gonad.9,10) Nevertheless, awareness of the risks of long-term radiation exposure is not high, and education to prevent it is not systematically conducted.11,12) In particular, in a survey on the awareness orthopedic surgeons have of complications related to radiation, only 87 of 1,024 surgeons (8.5%) had read an article related to fluoroscopy risk at least once. Moreover, almost all participants (99.2%) were unaware of the amount of radiation the patient was exposed to during fluoroscopy.13)
The International Commission on Radiological Protection emphasized the importance of shielding to minimize radiation exposure.14) Therefore, personal protectors for radiation shielding, such as aprons, protective glasses, thyroid shields, and gloves, have been introduced. These personal shields were mostly made using lead material because of its high radiation attenuation coefficient and low cost and moreover, it has various problems due to human health and environmental problems. Therefore, research on reducing the lead content of products or developing shielding sheets using other alternative materials is ongoing.
In this study, the shielding effect of a non-lead radiation shielding sheet, which was designed for minimizing the exposure of medical staff and patients, was evaluated using an anthropomorphic phantom. We evaluated the radiation protection performance of the sheet using two possible scenarios in which the sheet was located on the X-ray tube or under the phantom during C-arm fluoroscopy.
Materials and Methods
1. Radiation shielding sheet
We adopted a non-lead radiation shielding sheet (ROO201128; Pentas, Busan, Korea) with high flexibility and low weight. It mainly consisted of tungsten and bismuth which have high atomic numbers; thus, a high radiation attenuation rate was expected in the range of up to 100 kVp. The size and inner thickness of the sheet were 45 cm×35 cm and 0.45 mm, respectively.
2. Experimental setup
A C-arm fluoroscopic unit (Arcadis Varic; Siemens, München, Germany) was used to irradiate an anthropomorphic chest phantom (N1 Lungman; Kagaku, Kyoto, Japan) with fixed conditions of 64 kVp and 1.5 mA. The phantom was located such that the center of the sternum coincided with the center of the X-ray beam. The equivalent dose values were measured using a gamma survey meter (PM1401K-3P; Polimaster, Minsk, Belarus) in millisievert per hour (mSv/h).
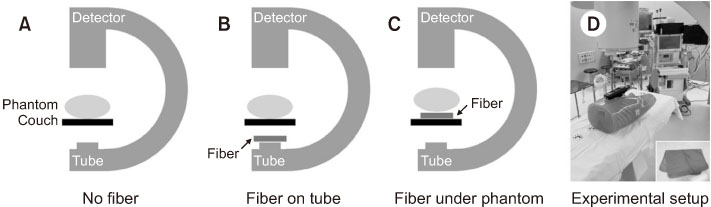
We designed three scenarios: without the fiber (Sno), the fiber on the X-ray tube (Stube), and the fiber under the phantom (Sphantom). In each scenario, we measured the central dose in front of the phantom and then measured three dose values according to the distances from the beam center (30, 60, and 90 cm) in each of the three directions (cephal, caudal, and operator’s direction). The operator’s direction was set to the opposite side of the fluoroscopy, and the measuring instrument measured at the same height as the phantom center in all directions. The total number of data points was 3 (scenarios)×10 (measurements per scenario)=30. A brief description of our experimental setup is presented in Fig. 1.
Fig. 1
Description of the different scenarios (A-D) using the radiation shielding fiber and experimental setup.
3. Measurements and analysis
We performed measurements 4 times for each data point. The mean and standard deviation of each data point were calculated after excluding the measured value with the largest difference from the mean. The dose values located between the measured data points were interpolated using a surface-fitting method. The dose values between different scenarios and directions were compared and analyzed. In addition, X-ray images with sizes of 1,024×1,024 were also acquired. The contrast-to-noise ratios (CNR) between the tissue and bone in the images that were acquired using different experimental conditions were compared to assess the effect of each condition on image quality.
Results
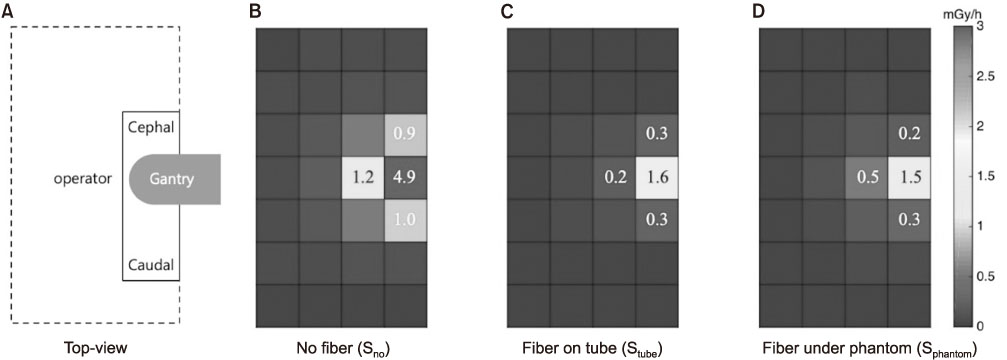
The measured dose distributions were compared between the different scenarios, as shown in Fig. 2.
Fig. 2
Measured dose distributions of the three different scenarios. (A-D) All numbers presented in the figure are in mSv/h, and the pixel dimension is 30 cm×30 cm.
In all scenarios, the dose value drastically decreased as the distance from the beam center increased. In the area within a 30 cm radius from the beam center, the measured doses were reduced by 72.9% and 67.4% on mean in Stube and Sphantom, respectively. In the case of a longer 60 cm radius from the beam center, the measured doses were reduced by 70.6% and 61.9% on mean in Stube and Sphantom, respectively.
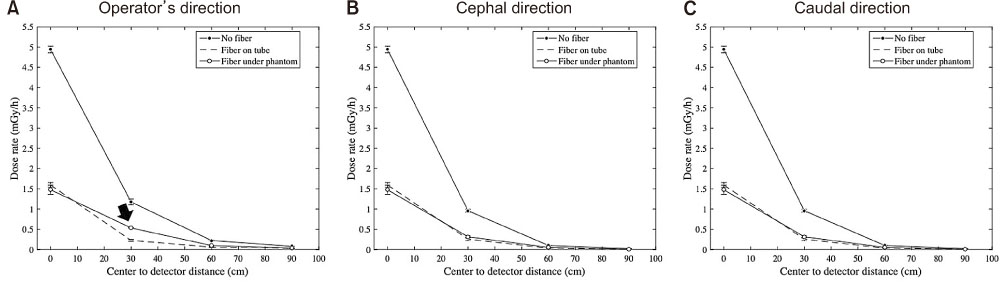
The behaviors of dose reduction curves among Sno, Stube, and Sphantom were compared in each direction (Fig. 3).
Fig. 3
Comparison of measured dose curves between different scenarios in three directions (A-C). The black arrow shows a noticeably high dose value toward the operator.
No significant difference was noted between the dose curves in the cephal and caudal directions, as shown in Fig. 3B, C, respectively. However, in the operator’s direction, a noticeably high dose value (0.53 mSv/h), as indicated by the black arrow in Fig. 3A was observed at the center-todetector distance of 30 cm in Sphantom. In Stube and Sphantom, all dose values measured at positions more than 60 cm away from the beam center were less than 0.1 mSv/h.
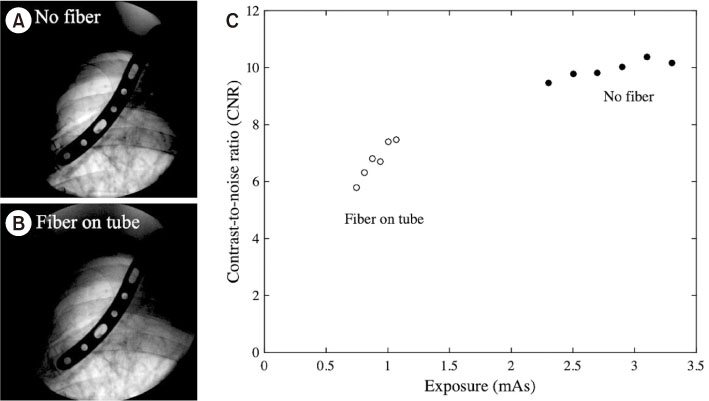
The CNR between the tissue and bone in the images were used to evaluate the effect of exposure on image quality (Fig. 4). The brightness of the image appeared to be lower in Stube, and the image contrast also seemed to be lower in Stube (Fig. 4B) compared to that in Sno (Fig. 4A). The CNR values of images acquired in Sno were in a different group from those acquired in Stube, as shown in Fig. 4C. When the radiation shielding fiber was placed on the X-ray tube, the radiation exposure was reduced by 72.9% on mean. However, the mean CNR of the acquired images only decreased by 26.5%.
Fig. 4
Examples of images acquired using (A) no fiber and (B) fiber on the X-ray tube, and (C) comparison of image quality between the two different conditions with respect to the amount of exposure.
Discussion
Kaplan et al.8) found that only 69% of trainees were aware of the “ALARA” principle. Additionally, in one study, only 18% of trainees had read any literature on radiation safety and only 24% had a thyroid shield.12) A personal apron or glasses for radiation shielding is very important. However, in the study by Cremen and McNulty,15) 3 of 14 hospitals did not have enough aprons, and only 1 had individual aprons. Additionally, 72% of hospitals only had medium- and large-size aprons, which did not provide adequate shielding due to poorly fitting over clothing.15) Moreover, although protective equipment for radiation shielding was introduced to medical staff in many studies, the authors developed the shielding sheet used in this study because patients were also exposed to radiation. A study by Cha et al.16) also reported a radiation shielding rate of 55.3%-93.6% using a phantom model for patients using a shielding sheet. In our study, the overall radiation exposure reduction rate by the sheet was 66.2% on mean within a radius of 60 cm from the beam center. This means that the radiation exposure of both medical staff and patients could be effectively reduced using the sheet only. Furthermore, while the radiation exposure was greatly reduced by using the fiber, the image quality was only slightly reduced.
The Stube scenario is superior to the Sphantom scenario regarding radiation protection. In Stube, the measured dose at the beam center was slightly increased while the dose in the operator’s direction significantly decreased by 56.6%, compared to Sphantom. Since the sheet under the phantom attenuates only the portion of the primary beam that goes toward the phantom, there is no significant reduction in the scatter radiation between the X-ray tube and the operator in Sphantom. In contrast, the sheet on the X-ray tube attenuates the entire primary beam so that the dose reduction to both the operator and patients can be expected in Stube. Therefore, it would be most beneficial to place the radiation shielding sheet on the X-ray tube during C-arm fluoroscopy. The result of our study is valid only under the condition that the operator stands by the image identifier as shown in Fig. 1. The operators are expected to be exposed to much more scattered X-rays if they stand by the X-ray tube.17) Hayda et al.17) mentioned several method to minimize radiation exposure of orthopedic surgeons in a review paper. In order to minimize radiation exposure, the use of radiation shielding and leaded glasses was recommended, and the location of the C-arm and the position of the operator were explained. During surgery, a surgeon standing on the emitter side of the C-arm in a horizontal position sustains 4-8 times more scattered radiation exposure than a surgeon standing on the intensifier side of the C-arm.18,19)
Lead is widely used as a radiation shielding agent due to its low cost and high processability. However, its harmful effects on the human body are already well known.20) Furthermore, due to lead being heavy, 25% of users reported problems with their hips, knees, and ankles due to wearing lead aprons, with 50% of users reporting spine problems. Classified as a toxic heavy metal, lead can have serious long-term effects on human health and the environment. Therefore, efforts to find a non-toxic, lightweight, flexible, and inexpensive radiation shielding material to replace lead are especially needed. In order to compensate for the various disadvantages of lead, aprons and shields using leadfree materials were introduced.21,22) Among these materials, a shield using a tungsten-based material was introduced, and many studies mentioned that it is a material that can replace lead.23,24,25) The sheet used in this study was also fabricated based on tungsten. In an experiment with the same radiation dose generated by the C-arm currently used in orthopedic surgery, the authors confirmed a meaningful shielding rate of tungsten-based material. Besides tungsten, bismuth and barium sulfate are the main substitutes for lead. A shielding sheet using these materials undergoes a rather complex mixing process because it must have high flexibility in order to be worn or stored on the body and must be stable even in a disinfection process using alcohol. There is still a debate about materials and blend manufacturing methods optimized in terms of the economics and functionality of shielding sheets.
Moreover, due to lead’s heaviness and toxicity to the human body, it has recently been replaced with an ecofriendly shielding material. Shielding materials that can replace lead include barium, boron, tin, bismuth, and tungsten, of which tungsten is the most used recently.26,27) According to the study by Chou et al.,5) when analyzing the absorbed radiation dose according to the type of shielding material, it was confirmed that barium sulfate had the lowest shielding rate, followed by bismuth, lead, and tungsten. This is thought to be because bismuth, lead, and tungsten have a higher atomic number than barium.28) Lead has a higher atomic number than tungsten. However, since the density of tungsten is higher than that of lead, it has a higher electron density than lead when it is the same size; thus, it has an approximately 1.5 times higher shielding efficiency than lead.29) However, tungsten is a representative rare metal and may be less efficient in terms of economy than lead. In order to compensate for these disadvantages, research on manufacturing methods or mixed manufacturing with other materials is continuously required.
Radiation shielding is important for clinicians and patients; however, the purpose of using fluoroscopy is to be able to see the target point clearly during surgery or the procedure. To our knowledge, no study has assessed the image quality during C-arm fluoroscopy and radiation shielding. Although our study used a phantom model, it confirmed that the image quality was reduced by 26.5%. It is difficult to determine exactly how much this reduction will affect the operation or procedure when actual shielding sheets are used. Hence, future studies are necessary to evaluate the effect of reduced image quality during actual operation.
This study has several limitations. First, the authors adopted an anthropomorphic phantom instead of a clinical trial. However, the authors tried to recreate the conditions that would occur in real surgery. The same radiation dose was generated using the C-arm as that used during surgery in the operating room. Second, although the degradation in image quality caused by fiber introduction has been confirmed to be limited, its effect on clinical performances should be objectively evaluated. For the quantitative evaluation of image quality with shielding sheets, the future research is required.
Conclusion
The performance of a lead-free radiation shielding sheet was evaluated during C-arm fluoroscopy, and the most beneficial scenario in which the sheet can be utilized was verified when the sheet was placed on the X-ray tube. This study provides useful information and insights to the operator who designs the overall surgical plan using C-arm fluoroscopy.
Financial support:None.
Conflict of interests:None.
References
-
Seo SY, Han MS, Kim CG, Jeon MC, Kim YK, Kim GJ. A study on the usefulness of a fusion model designed cloak shield to reduce the radiation exposure of the assistant during CT of severely injured patient. J Korea Converg Soc 2017;8:211–216.
-
-
Jo HJ, Park ET, Kim JH. Reduced effect of kV-CBCT dose by use of shielding materials in radiation therapy. J Korean Soc Radiol 2018;12:467–474.
-
-
Jang DG, Kim GH, Park CW. Analysis of shielding effect of lead and tungsten by use of medical radiation. J Korean Soc Radiol 2018;12:173–178.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

