Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 34(1); 2021 > Article
- Original Article Clinical Outcomes of Customized Staple Fixation Using K-wire in Metacarpal Base or Neck Fractures
- Hong-ki Jin, Hyoung Min Kim, Yong Seung Oh, Jihoon Kim
-
Journal of Musculoskeletal Trauma 2021;34(1):23-29.
DOI: https://doi.org/10.12671/jkfs.2021.34.1.23
Published online: January 31, 2021

- 728 Views
- 4 Download
- 1 Crossref
- 0 Scopus
Abstract
Purpose
This study was designed to evaluate the radiological and clinical outcomes of a new surgical technique—customized staple fixation using K-wire—in displaced metacarpal neck or base fractures.
Materials and Methods: From November 2016 to May 2017, 13 unstable metacarpal neck and base fractures (10 patients) were treated with II-shaped customized K-wire staples fixation, after performing open reductions through minimal dorsal incisions. The radiological and clinical outcomes were retrospectively evaluated.
Results: A mean of 2.6 staples were used for each fracture fixation. Preoperative angulation of 36.3°was reduced to 3.1° postoperatively. A week after surgery, the volar short arm splint was replaced with a dorsal splint to initiate active range of motion exercise, and the splint was subsequently removed after 3 weeks. The radiologic union was achieved at a mean of 5.1 weeks, and total active motion was recovered at a mean of 7.4 weeks. On a mean, K-wire staples were removed at 16.5 weeks after the surgery, and the mean treatment took 18.6 weeks. At the final follow-up (at mean 27.3 weeks), no significant difference was observed for total active motion of the digits and grip strength, when compared to the contralateral hand. Complete union was achieved in all fractures without deformity, or complications such as infection or nerve injury. All patients were satisfied with the cosmetic and functional outcomes.
Conclusion: K-wire stapling is an effective alternative modality in treating unstable displaced metacarpal neck or base fractures. It requires minimal incision to enable open reduction. In addition, early mobilization is ensured through the rigid fixations. Moreover, it prevents postoperative joint stiffness and reduces the time needed for treatment.
Published online Jan 25, 2021.
https://doi.org/10.12671/jkfs.2021.34.1.23
Clinical Outcomes of Customized Staple Fixation Using K-wire in Metacarpal Base or Neck Fractures
Abstract
Purpose
This study was designed to evaluate the radiological and clinical outcomes of a new surgical technique—customized staple fixation using K-wire—in displaced metacarpal neck or base fractures.
Materials and Methods
From November 2016 to May 2017, 13 unstable metacarpal neck and base fractures (10 patients) were treated with II-shaped customized K-wire staples fixation, after performing open reductions through minimal dorsal incisions. The radiological and clinical outcomes were retrospectively evaluated.
Results
A mean of 2.6 staples were used for each fracture fixation. Preoperative angulation of 36.3° was reduced to 3.1° postoperatively. A week after surgery, the volar short arm splint was replaced with a dorsal splint to initiate active range of motion exercise, and the splint was subsequently removed after 3 weeks. The radiologic union was achieved at a mean of 5.1 weeks, and total active motion was recovered at a mean of 7.4 weeks. On a mean, K-wire staples were removed at 16.5 weeks after the surgery, and the mean treatment took 18.6 weeks. At the final follow-up (at mean 27.3 weeks), no significant difference was observed for total active motion of the digits and grip strength, when compared to the contralateral hand. Complete union was achieved in all fractures without deformity, or complications such as infection or nerve injury. All patients were satisfied with the cosmetic and functional outcomes.
Conclusion
K-wire stapling is an effective alternative modality in treating unstable displaced metacarpal neck or base fractures. It requires minimal incision to enable open reduction. In addition, early mobilization is ensured through the rigid fixations. Moreover, it prevents postoperative joint stiffness and reduces the time needed for treatment.
Fig. 1
A 2-cm longitudinal incision was made at the fracture site. After open reduction, the fracture site was temporarily fixed using the K-wire.
Fig. 2
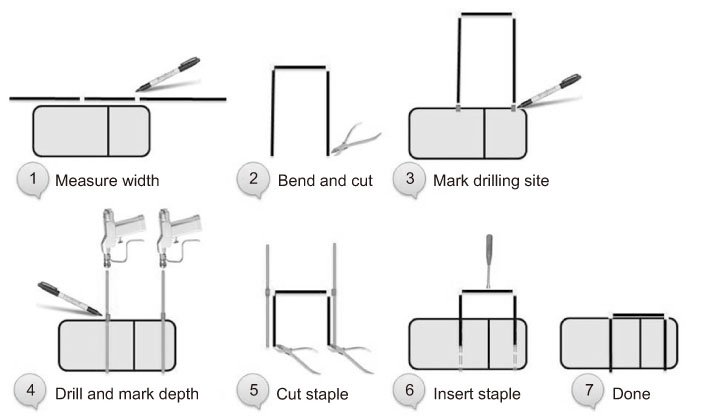
Procedure of customized K-wire stapling technique.
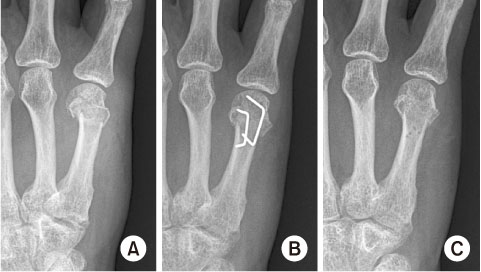
Fig. 3
(A) 5th metacarpal neck fracture with 31° dorsal angulation after trauma. (B) Postoperative x-ray shows reduction and secure fixation of the fracture site using 2 staple fixation. (C) Staples were removed 3 months after trauma.
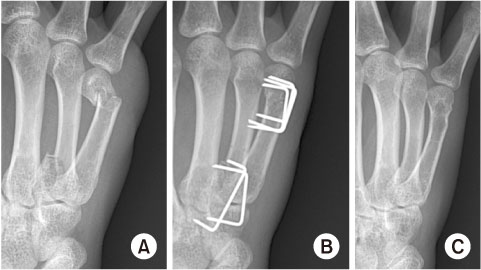
Fig. 4
(A) Fracture and lateral subluxation of the 4th metacarpal base, and 68° dorsal angulation after a punch injury with closed fist. (B) Postoperative x-ray shows reduction and secure fixation of the fracture site. (C) Staples were removed 1 year after trauma.
Fig. 5
At 1-year follow-up, normal total active motion of digits was restored without deformity or angulation.
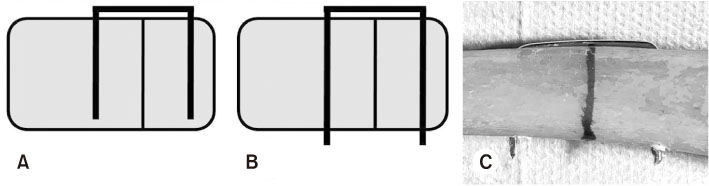
Fig. 6
(A) Conventional unicortical staple fixation method, ordinary staple. (B, C) Bicortical fixation of the K-wire staple.
Financial support:None.
Conflict of interests:None.
References
-
Nakashian MN, Pointer L, Owens BD, Wolf JM. Incidence of metacarpal fractures in the US population. Hand. N Y 2012;7:426–430.
-
-
Jahss SA. Fractures of the metacarpals: a new method of reduction and immobilization. J Bone Joint Surg 1938;20:178–186.
-
-
Harris AR, Beckenbaugh RD, Nettrour JF, Rizzo M. Metacarpal neck fractures: results of treatment with traction reduction and cast immobilization. Hand. N Y 2009;4:161–164.
-
-
Choi SJ, Chang SK. Treatment method of the metacarpal bone fractures with retrograde percutaneous intramedullary K-wire fixation to decrease the injury of extensor tendon. J Korean Soc Surg Hand 2004;9:117–122.
-
-
Kwon GD, Yeo YB, Rho JH, et al. Biomechanical study of fixation methods for comminuted phalangeal fractures. J Korean Soc Surg Hand 2006;11:221–226.
-
- Related articles

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS




 Cite
Cite

