Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 29(4); 2016 > Article
-
Original Article
- The Significance of Calcaneal Posterior Tuberosity Fragment Reduction When Treated with Open Reduction in Displaced Intra-Articular Calcaneal Fractures
- Hong-Ki Park, M.D., Jong-Ryoon Baek, M.D., Jang-Seok Choi, M.D., Sang-Jin Lee, M.D., Je-Won Paik, M.D.
-
Journal of the Korean Fracture Society 2016;29(4):233-241.
DOI: https://doi.org/10.12671/jkfs.2016.29.4.233
Published online: October 20, 2016
Department of Orthopedic Surgery, Gachon University Gil Medical Center, Incheon, Korea.
- Address reprint requests to: Hong-Ki Park, M.D. Department of Orthopedic Surgery, Gachon University Gil Medical Center, 21 Namdong-daero 774beon-gil, Namdong-gu, Incheon 21565, Korea. Tel: 82-32-460-3384·Fax: 82-32-423-3384, phk@gilhospital.com
• Received: May 10, 2016 • Revised: June 8, 2016 • Accepted: July 1, 2016
Copyright © 2016 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 519 Views
- 3 Download
Abstract
-
Purpose
- We attempt to evaluate the significance of calcaneal posterior tuberosity fragment reduction when treated with surgical open reduction in displaced intra-articular calcaneal fractures.
-
Materials and Methods
- A total of 90 patients with displaced intra-articular calcaneal fracture, between January 2010 and December 2015, treated with open reduction and internal fixation were enrolled in this study. At postoperative 3 months, we evaluated the reduction state of calcaneal posterior tuberosity fragment by measuring the degree of lateral displacement of the posterior tuberosity fragment on the calcaneal axial view. Moreover, we also evaluated the difference in the calcaneal length and height with the uninjured side on the lateral view of both sides. In addition, we estimated the reduction state of the posterior facet by measuring the degree of gap and step-off on the semi-coronal view of postoperative computed tomography and estimated the restoration of calcaneal angle by measuring the difference in Böhler's and Gissane angle with the uninjured side on the lateral view of both sides.
-
Results
- The correlation coefficient with 3 components for evaluating the reduction state of posterior tuberosity fragment and gap and step-off of posterior facet was r=0.538, 0.467, r=0.505, 0.456, r=0.518, and 0.493, respectively, and restoration of Böhler's and Gissane angle was r=0.647, 0.579, r=0.684, 0.630, r=0.670, and 0.628, respectively. The relationship of each component shows a significant correlation as all p-values were <0.01.
-
Conclusion
- The precise reduction of calcaneal posterior tuberosity fragment developed by the primary fracture line was considered as an important process of anatomical reduction of calcaneal body, including the posterior facet and calcaneal angle restoration.
- 1. Benirschke SK, Mayo KA, Sangeorzan BJ, Hansen ST. Results of operative treatment of calcaneal fractures. In: Tscherne H, Schatzker J, editors. Major fractures of the pilon, the talus and the calcaneus. Berlin: Springer-Verlag; 1993. p. 215-227.Article
- 2. Carr JB, Hansen ST, Benirschke SK. Subtalar distraction bone block fusion for late complications of os calcis fractures. Foot Ankle, 1988;9:81-86.ArticlePDF
- 3. James ET, Hunter GA. The dilemma of painful old os calcis fractures. Clin Orthop Relat Res, 1983;(177):112-115.Article
- 4. Kitaoka HB, Schaap EJ, Chao EY, An KN. Displaced intra-articular fractures of the calcaneus treated non-operatively. Clinical results and analysis of motion and ground-reaction and temporal forces. J Bone Joint Surg Am, 1994;76:1531-1540.Article
- 5. Zwipp H, Tscherne H, Thermann H, Weber T. Osteosynthesis of displaced intraarticular fractures of the calcaneus. Results in 123 cases. Clin Orthop Relat Res, 1993;(290):76-86.Article
- 6. Buckley R, Tough S, McCormack R, et al. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am, 2002;84:1733-1744.Article
- 7. Giachino AA, Uhthoff HK. Intra-articular fractures of the calcaneus. J Bone Joint Surg Am, 1989;71:784-787.Article
- 8. Ibrahim T, Rowsell M, Rennie W, Brown AR, Taylor GJ, Gregg PJ. Displaced intra-articular calcaneal fractures: 15-year follow-up of a randomised controlled trial of conservative versus operative treatment. Injury, 2007;38:848-855.Article
- 9. Järvholm U, Körner L, Thorén O, Wiklund LM. Fractures of the calcaneus. A comparison of open and closed treatment. Acta Orthop Scand, 1984;55:652-656.Article
- 10. Parmar HV, Triffitt PD, Gregg PJ. Intra-articular fractures of the calcaneum treated operatively or conservatively. A prospective study. J Bone Joint Surg Br, 1993;75:932-937.ArticlePDF
- 11. Thordarson DB, Krieger LE. Operative vs. nonoperative treatment of intra-articular fractures of the calcaneus: a prospective randomized trial. Foot Ankle Int, 1996;17:2-9.Article
- 12. Randle JA, Kreder HJ, Stephen D, Williams J, Jaglal S, Hu R. Should calcaneal fractures be treated surgically? A meta-analysis. Clin Orthop Relat Res, 2000;377:217-227.Article
- 13. Myerson M, Quill GE Jr. Late complications of fractures of the calcaneus. J Bone Joint Surg Am, 1993;75:331-341.Article
- 14. Richards PJ, Bridgman S. Review of the radiology in randomised controlled trials in open reduction and internal fixation (ORIF) of displaced intraarticular calcaneal fractures. Injury, 2001;32:633-636.Article
- 15. Sanders R, Vaupel ZM, Erdogan M, Downes K. Operative treatment of displaced intraarticular calcaneal fractures: long-term (10-20 Years) results in 108 fractures using a prognostic CT classification. J Orthop Trauma, 2014;28:551-563.Article
- 16. Hammesfahr JF. Surgical treatment of calcaneal fractures. Orthop Clin North Am, 1989;20:679-689.Article
- 17. Leung KS, Yuen KM, Chan WS. Operative treatment of displaced intra-articular fractures of the calcaneum. Medium-term results. J Bone Joint Surg Br, 1993;75:196-201.ArticlePDF
- 18. Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res, 1993;(290):87-95.Article
- 19. Sanders R. Current concepts review Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am, 2000;82:225-250.Article
- 20. Miric A, Patterson BM. Pathoanatomy of intra-articular fractures of the calcaneus. J Bone Joint Surg Am, 1998;80:207-212.Article
- 21. Carr JB. Surgical treatment of the intra-articular calcaneus fracture. Orthop Clin North Am, 1994;25:665-675.Article
- 22. Ogut T, Ayhan E, Kantarci F, Unlu MC, Salih M. Medial fracture line significance in calcaneus fracture. J Foot Ankle Surg, 2001;50:517-521.Article
- 23. Rammelt S, Zwipp H. Calcaneus fractures: facts, controversies and recent developments. Injury, 2004;35:443-461.Article
- 24. Eastwood DM, Gregg PJ, Atkins RM. Intra-articular fractures of the calcaneum. Part I: pathological anatomy and classification. J Bone Joint Surg Br, 1993;75:183-188.ArticlePDF
- 25. Tennent TD, Calder PR, Salisbury RD, Allen PW, Eastwood DM. The operative management of displaced intra-articular fractures of the calcaneum: a two-centre study using a defined protocol. Injury, 2001;32:491-496.Article
- 26. Benirschke SK, Sangeorzan BJ. Extensive intraarticular fractures of the foot. Surgical management of calcaneal fractures. Clin Orthop Relat Res,, 1993;(292):128-134.Article
REFERENCES
Fig. 1
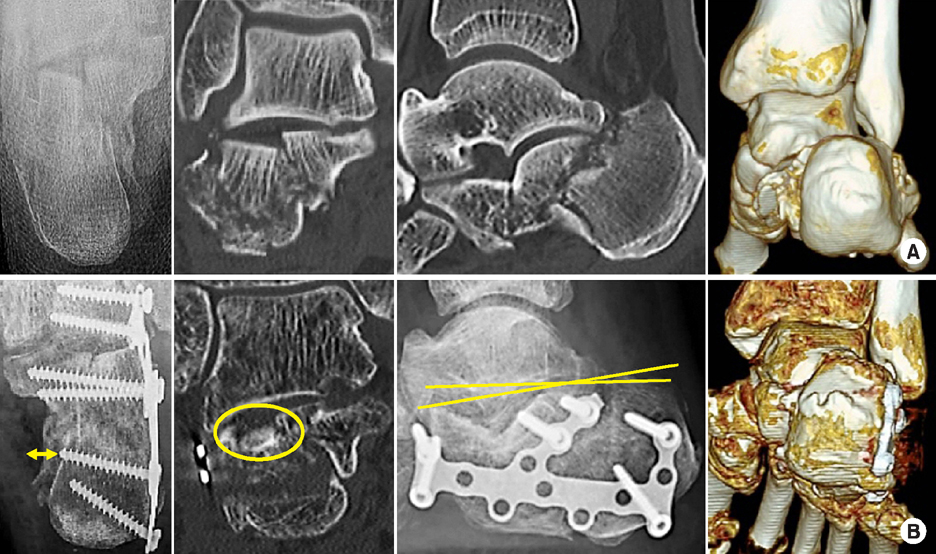
A 57-year-old male patient, with a Sanders type III intra-articular calcaneal fracture, was treated using open reduction and internal fixation with the extensile lateral approach. (A) Preoperative x-ray and computed tomography (CT) scans. (B) Postoperative x-ray and CT scans showed inaccurate reduction of posterior tuberosity fragment (yellowish arrow line), posterior facet step-off (yellowish circle), and collapsed Böhler's angle (yellowish line).
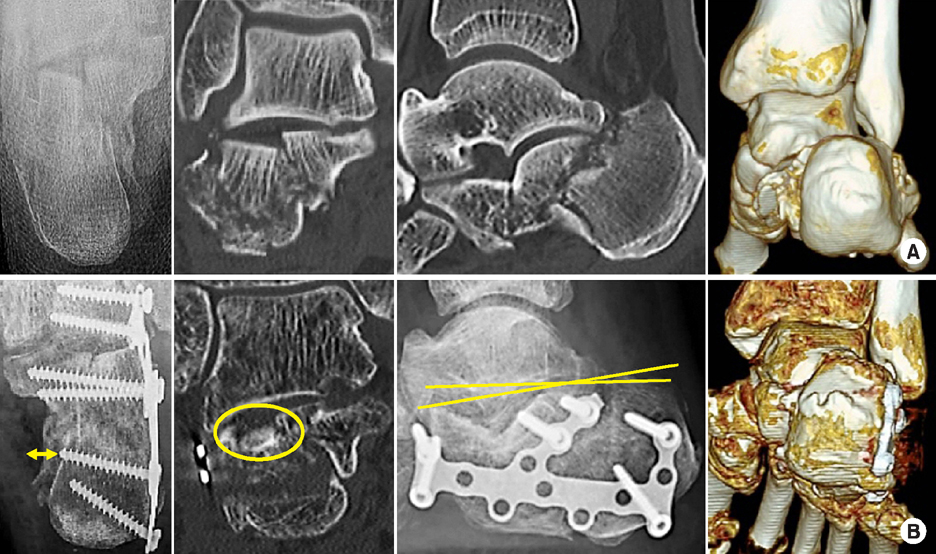
Fig. 2
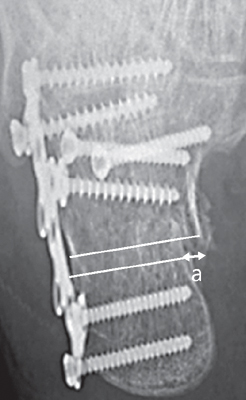
The degree of lateral displacement of the posterior tuberosity fragment (a) is measured as the gap between the superomedial fragment and posterior tuberosity fragment on the medial aspect of the calcaneal axial view.
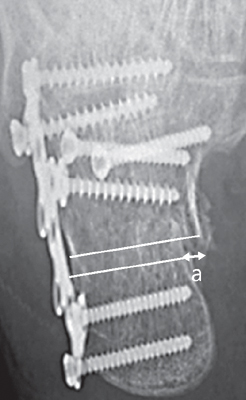
Fig. 3
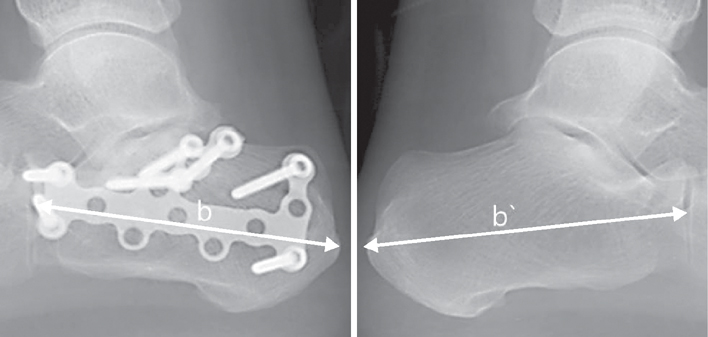
The difference in the calcaneal length with the uninjured side (b-b') is measured from the most posterior point of the tuberosity to the calcaneocuboid joint on the lateral view.
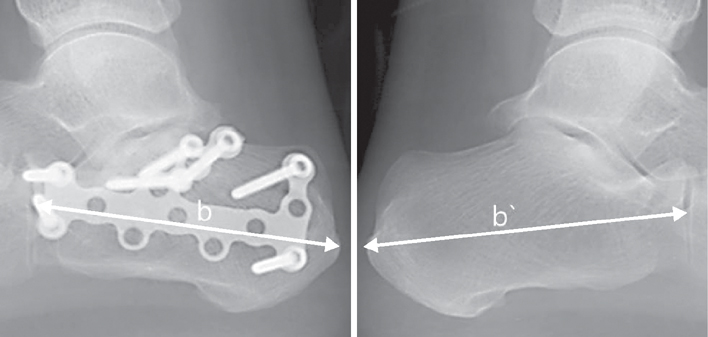
Fig. 4
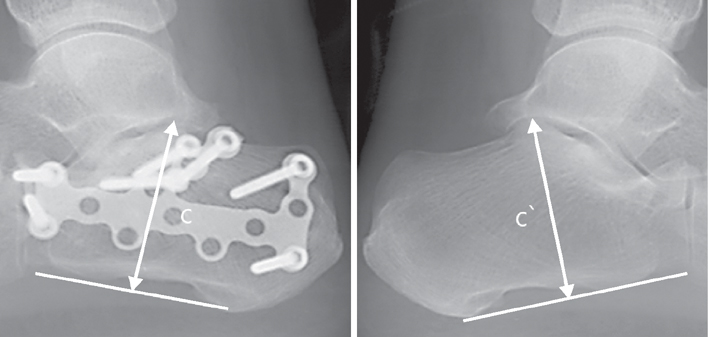
The difference in the calcaneal height with the uninjured side (c-c') is measured as a perpendicular distance from the most superior part of the posterior facet to the inferior aspect line between the calcaneocuboid joint and posterior tuberosity on the lateral view.
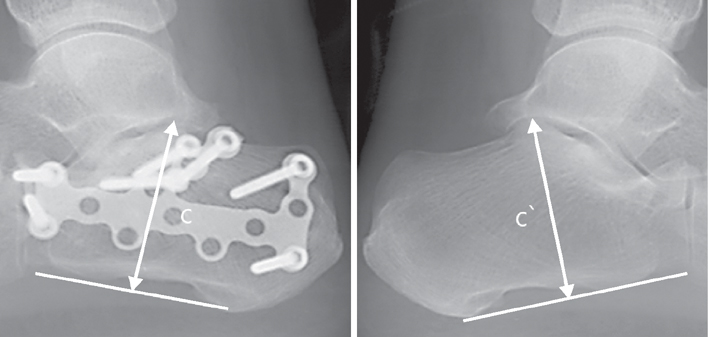
Fig. 5
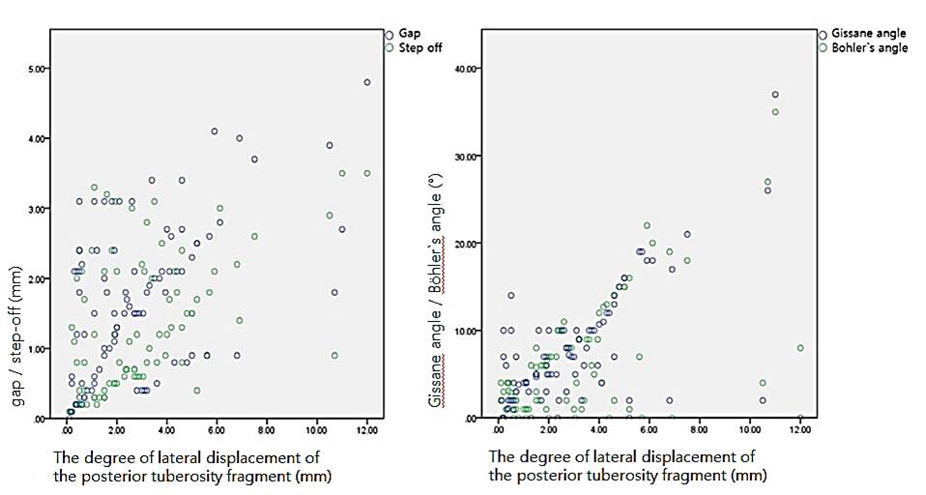
The relationship between the degree of lateral displacement of the posterior tuberosity fragment and gap/step-off of posterior facet and restoration of Gissane angle/Böhler's angle shows a significant correlation (p<0.01).
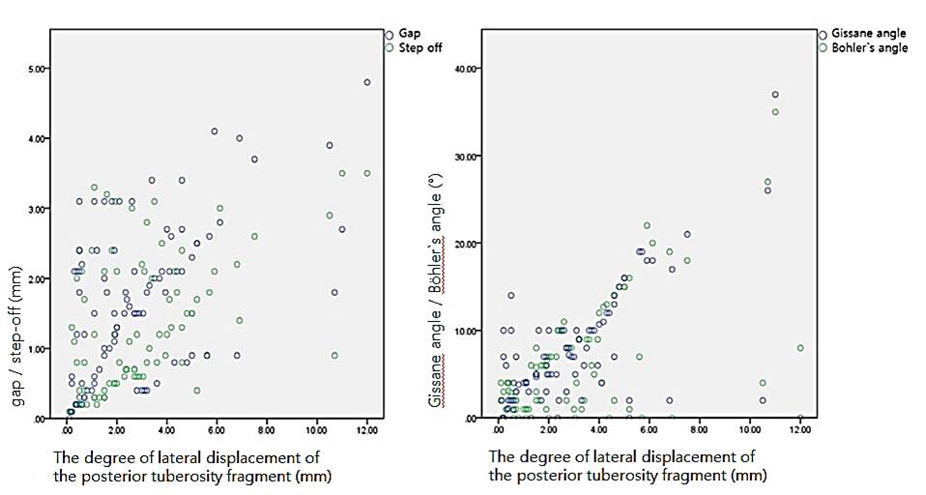
Fig. 6
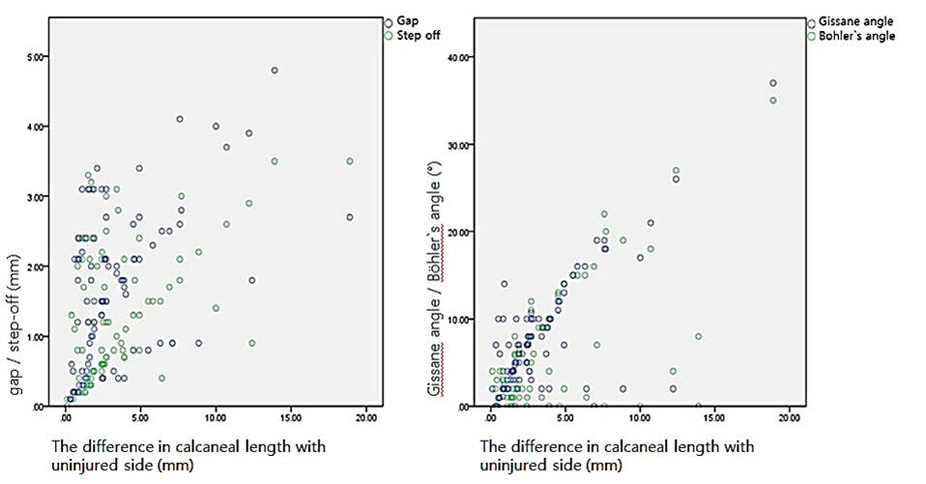
The relationship between the difference in calcaneal length with uninjured side and gap/step-off of posterior facet and restoration of Gissane angle/Böhler's angle shows a significant correlation (p<0.01).
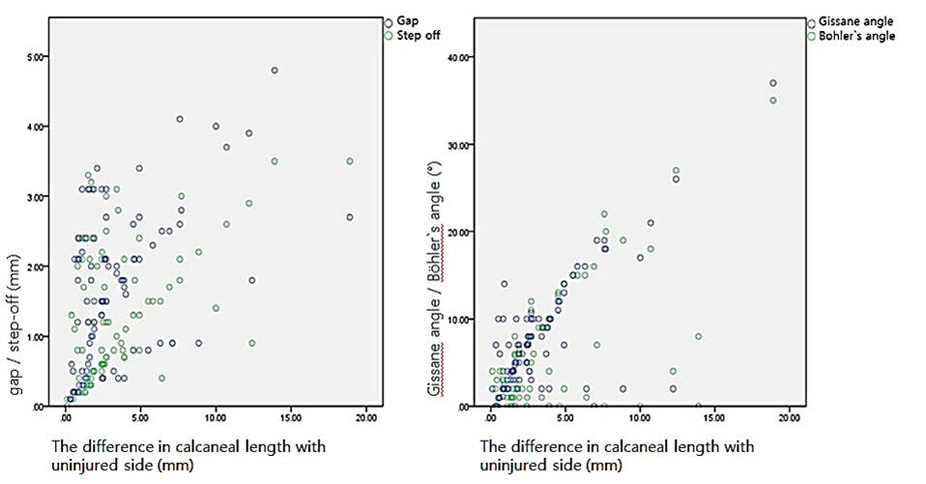
Fig. 7
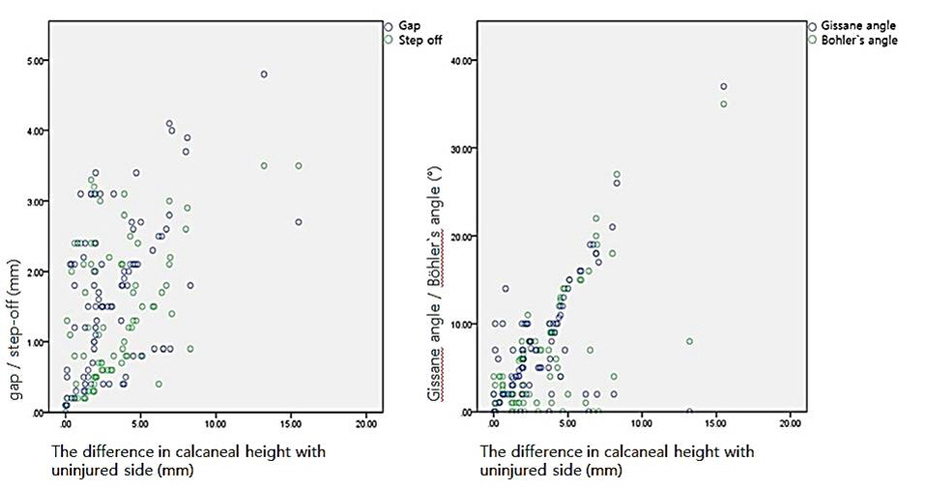
The relationship between the difference in the calcaneal height with the uninjured side and gap/step-off of posterior facet and restoration of Gissane angle/Böhler's angle shows a significant correlation (p<0.01).
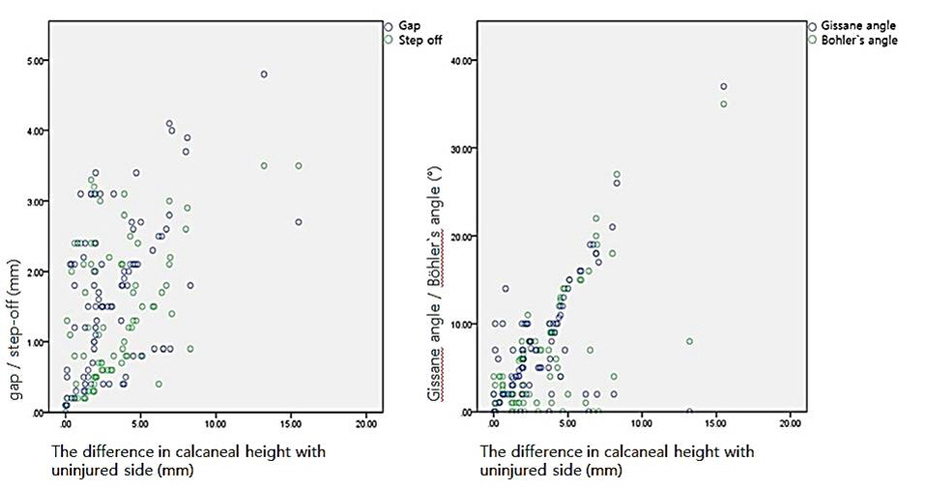
Fig. 8
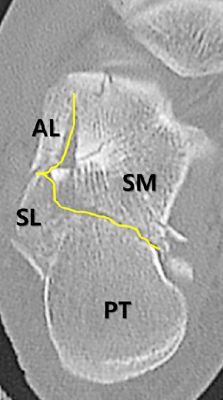
The primary fracture line (yellowish line) produced two large fragments, SM, and posterolateral fragment (SL and PT). AL: Anterolateral fragment, SL: Superolateral fragment, SM: Superomedial fragment, PT: Posterior tuberosity fragment.
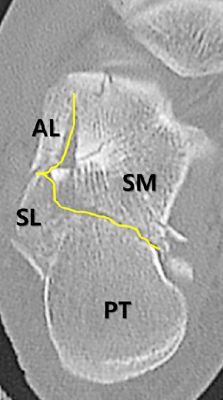
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

The Significance of Calcaneal Posterior Tuberosity Fragment Reduction When Treated with Open Reduction in Displaced Intra-Articular Calcaneal Fractures
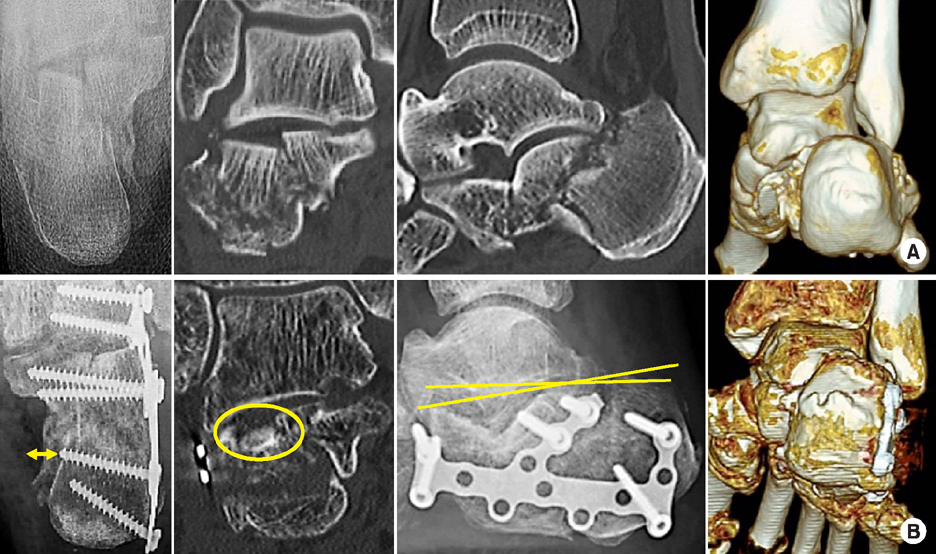
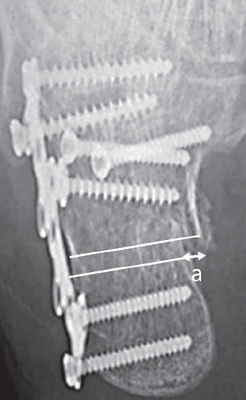
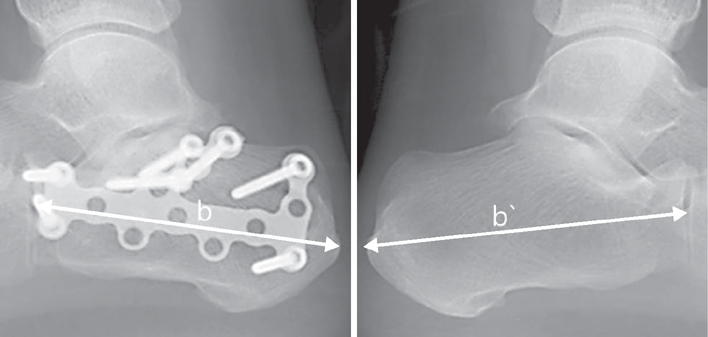
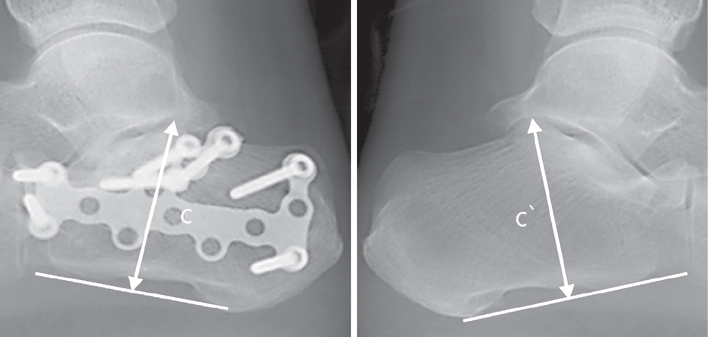
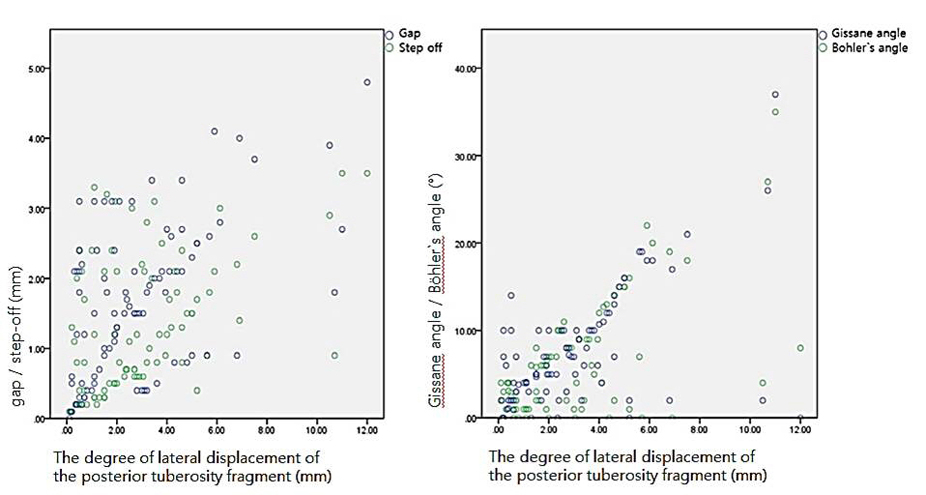
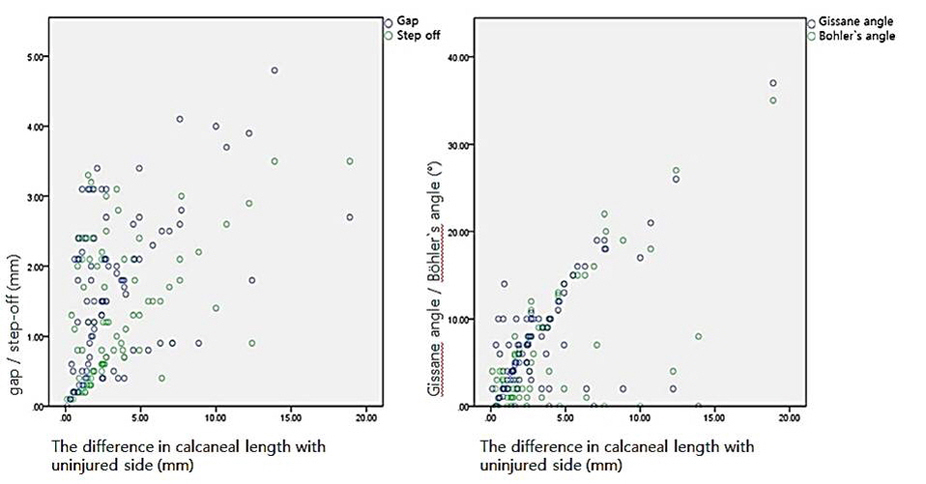
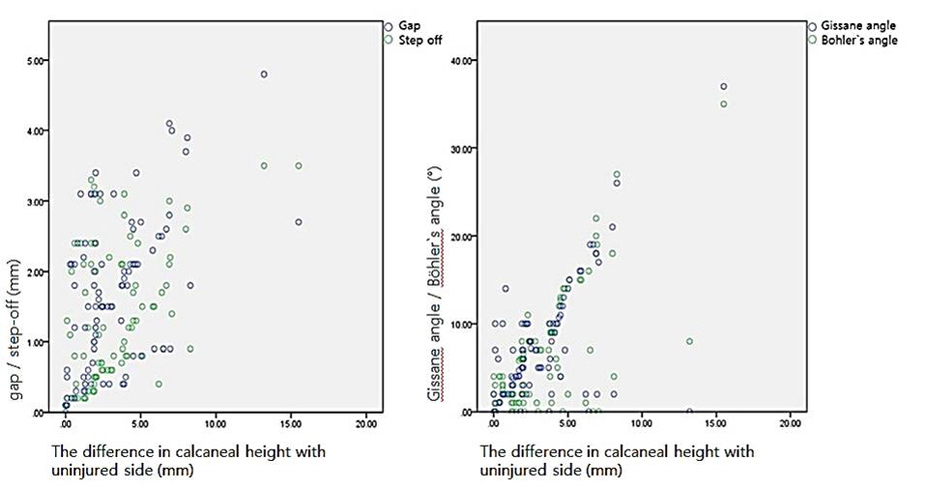
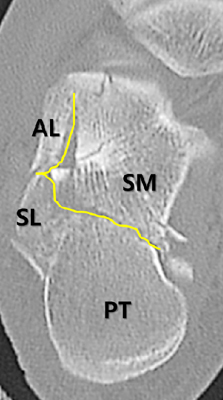
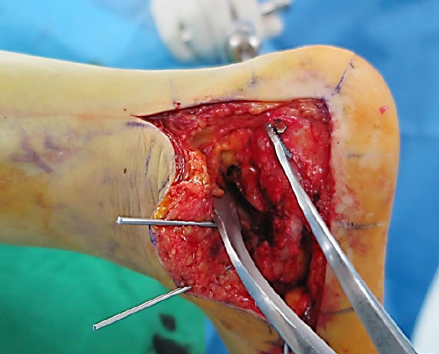
Fig. 1
A 57-year-old male patient, with a Sanders type III intra-articular calcaneal fracture, was treated using open reduction and internal fixation with the extensile lateral approach. (A) Preoperative x-ray and computed tomography (CT) scans. (B) Postoperative x-ray and CT scans showed inaccurate reduction of posterior tuberosity fragment (yellowish arrow line), posterior facet step-off (yellowish circle), and collapsed Böhler's angle (yellowish line).
Fig. 2
The degree of lateral displacement of the posterior tuberosity fragment (a) is measured as the gap between the superomedial fragment and posterior tuberosity fragment on the medial aspect of the calcaneal axial view.
Fig. 3
The difference in the calcaneal length with the uninjured side (b-b') is measured from the most posterior point of the tuberosity to the calcaneocuboid joint on the lateral view.
Fig. 4
The difference in the calcaneal height with the uninjured side (c-c') is measured as a perpendicular distance from the most superior part of the posterior facet to the inferior aspect line between the calcaneocuboid joint and posterior tuberosity on the lateral view.
Fig. 5
The relationship between the degree of lateral displacement of the posterior tuberosity fragment and gap/step-off of posterior facet and restoration of Gissane angle/Böhler's angle shows a significant correlation (p<0.01).
Fig. 6
The relationship between the difference in calcaneal length with uninjured side and gap/step-off of posterior facet and restoration of Gissane angle/Böhler's angle shows a significant correlation (p<0.01).
Fig. 7
The relationship between the difference in the calcaneal height with the uninjured side and gap/step-off of posterior facet and restoration of Gissane angle/Böhler's angle shows a significant correlation (p<0.01).
Fig. 8
The primary fracture line (yellowish line) produced two large fragments, SM, and posterolateral fragment (SL and PT). AL: Anterolateral fragment, SL: Superolateral fragment, SM: Superomedial fragment, PT: Posterior tuberosity fragment.
Fig. 9
In the semi-coronal computed tomography scan, the tuberosity tilts into the varus and acts as a wedge between SL and SM, preventing a reduction of the posterior facet. SL: Superolateral fragment, SM: Superomedial fragment, PT: Posterior tuberosity fragment.
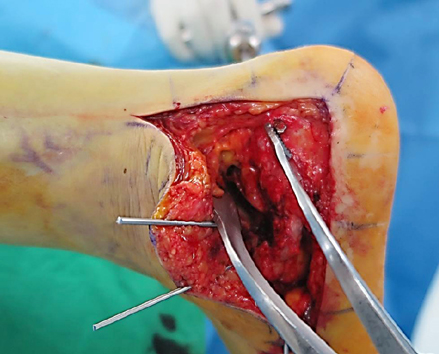
Fig. 10
We apply a distractor between the Schanz screw thread and K-wire inserted into the talar body and can achieve an effective traction of the tuberosity fragment.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
Fig. 9
Fig. 10
The Significance of Calcaneal Posterior Tuberosity Fragment Reduction When Treated with Open Reduction in Displaced Intra-Articular Calcaneal Fractures

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

