Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 27(2); 2014 > Article
-
Original Article
- Intramedullary Nailing of Distal Tibial Fractures with Percutaneous Reduction by Pointed Reduction Forceps
- Jae-Kwang Hwang, M.D., Chung-Hwan Kim, M.D., Young-Joon Choi, M.D., Gi-Won Lee, M.D., Hyun-Il Lee, M.D., Tae-Kyung Kim, M.D.
-
Journal of the Korean Fracture Society 2014;27(2):144-150.
DOI: https://doi.org/10.12671/jkfs.2014.27.2.144
Published online: April 18, 2014
Department of Orthopaedic Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- Address reprint requests to: Chung-Hwan Kim, M.D. Department of Orthopaedic Surgery, Gangneung Asan Hospital, 38 Bangdong-gil, Sacheon-myeon, Gangneung 210-711, Korea. Tel: 82-33-610-3249, Fax: 82-33-641-8050, chkim@gnah.co.kr
Copyright © 2014 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 533 Views
- 1 Download
Abstract
-
Purpose
- The purpose of this study is to analyze the radiographic and clinical results of intramedullary nailing after percutaneous reduction using pointed reduction forceps for spiral or oblique fractures of the distal tibia. The benefit of percutaneous reduction using pointed reduction forceps in anatomical reduction and maintenance was assessed.
-
Materials and Methods
- From January 2005 to December 2009, 47 cases of distal one-third tibial fracture were managed by intramedullary nailing using pointed reduction forceps. Thirty-eight cases were spiral fracture and nine cases were oblique fracture. In all cases, the percutaneous reduction was achieved using pointed reduction forceps under fluoroscopy control. While maintaining the reduction with the pointed reduction forceps, the intramedullary nail was inserted. The pointed reduction forceps were removed after insertion of proximal and distal inter-locking screws. Alignment was evaluated with anterior-posterior and lateral radiographs taken immediately post-operation and at the time of union.
-
Results
- At immediate post-operation, the mean displacement of valgus and anterior angulation was 0.57° and 0.24°, respectively. That of valgus and anterior angulation at bone union was 0.37° and 0.16°, respectively. The average duration of bone union was 16.1 weeks.
-
Conclusion
- Intramedullary nailing with percutaneous reduction using pointed reduction forceps for distal tibial fractures was an easy and effective method for achievement of accurate alignment intra-operatively. Accurate alignment was successfully maintained until bone union.
- 1. Janssen KW, Biert J, van Kampen A. Treatment of distal tibial fractures: plate versus nail: a retrospective outcome analysis of matched pairs of patients. Int Orthop, 2007;31:709-714.
- 2. Kim YS, Chung PH, Hwang CS, Kang S, Kim JP, Lee HM. Interlocking intramedullary nailing in distal tibial metaphyseal fractures. J Korean Fract Soc, 2005;18:269-274.
- 3. Seyhan M, Unay K, Sener N. Intramedullary nailing versus percutaneous locked plating of distal extra-articular tibial fractures: a retrospective study. Eur J Orthop Surg Traumatol, 2013;23:595-601.PDF
- 4. Yang SW, Tzeng HM, Chou YJ, Teng HP, Liu HH, Wong CY. Treatment of distal tibial metaphyseal fractures: Plating versus shortened intramedullary nailing. Injury, 2006;37:531-535.
- 5. Beazley JC, Hull P. Temporary intra-operative reduction techniques for tibial fracture fixation: a review of the literature. Injury, 2010;41:1228-1233.
- 6. Forman JM, Urruela AM, Egol KA. The percutaneous use of a pointed reduction clamp during intramedullary nailing of distal third tibial shaft fractures. Acta Orthop Belg, 2011;77:802-808.
- 7. Kim KC, Lee JK, Hwang DS, Yang JY, Kim YM. Provisional unicortical plating with reamed intramedullary nailing in segmental tibial fractures involving the high proximal metaphysis. Orthopedics, 2007;30:189-192.
- 8. Krettek C, Stephan C, Schandelmaier P, Richter M, Pape HC, Miclau T. The use of Poller screws as blocking screws in stabilising tibial fractures treated with small diameter intramedullary nails. J Bone Joint Surg Br, 1999;81:963-968.
- 9. Nork SE, Schwartz AK, Agel J, Holt SK, Schrick JL, Winquist RA. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Joint Surg Am, 2005;87:1213-1221.
- 10. Sharan AD, Jeshuran W, Mulligan M, McGuire K, Uhl R. Intramedullary nailing in a tibial shaft fracture with distal articular extension. Orthopedics, 2005;28:571-572.
- 11. Wysocki RW, Kapotas JS, Virkus WW. Intramedullary nailing of proximal and distal one-third tibial shaft fractures with intraoperative two-pin external fixation. J Trauma, 2009;66:1135-1139.
- 12. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int, 1994;15:349-353.PDF
- 13. Mohammed A, Saravanan R, Zammit J, King R. Intramedullary tibial nailing in distal third tibial fractures: distal locking screws and fracture non-union. Int Orthop, 2008;32:547-549.PDF
- 14. Konrath G, Moed BR, Watson JT, Kaneshiro S, Karges DE, Cramer KE. Intramedullary nailing of unstable diaphyseal fractures of the tibia with distal intraarticular involvement. J Orthop Trauma, 1997;11:200-205.
- 15. Egol KA, Weisz R, Hiebert R, Tejwani NC, Koval KJ, Sanders RW. Does fibular plating improve alignment after intramedullary nailing of distal metaphyseal tibia fractures? J Orthop Trauma, 2006;20:94-103.
- 16. Isik M, Subasi M, Karsli B, Saricicek V, Karsli G. Intramedullary nailing and angulation prevention in distal metaphyseal tibial fractures. Orthopedics, 2012;35:e1765-e1768.
- 17. Lee KB, Song SY, Kwon DJ, Lee YB, Rhee NK, Choi JH. A comparison between minimally invasive plate osteosynthesis & interlocking intramedullary nailing in distal tibia fractures. J Korean Fract Soc, 2008;21:286-291.
- 18. Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma, 2011;25:736-741.
- 19. Vallier HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): plating versus intramedullary nailing. J Orthop Trauma, 2008;22:307-311.
REFERENCES
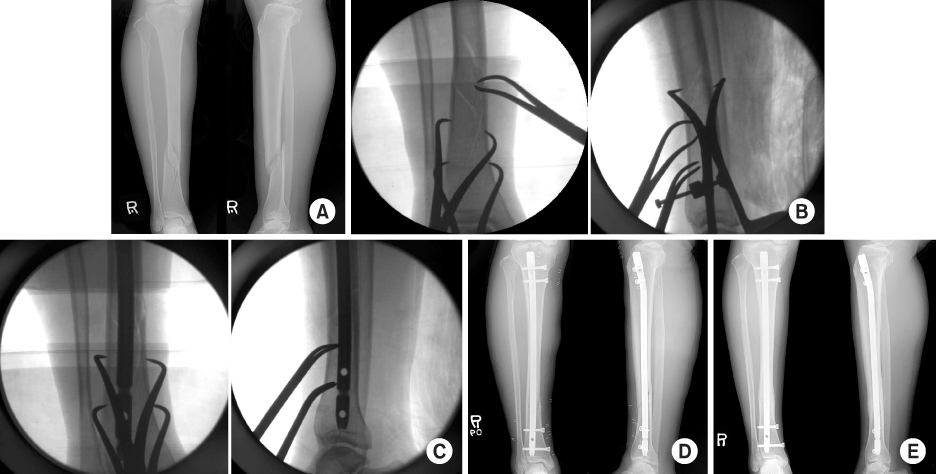
Figure & Data
REFERENCES
Citations

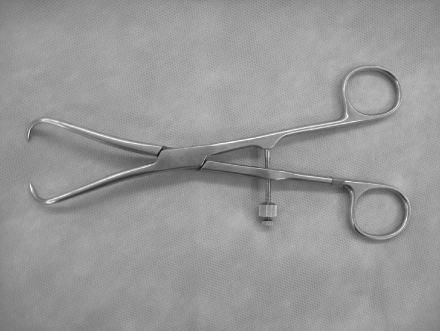
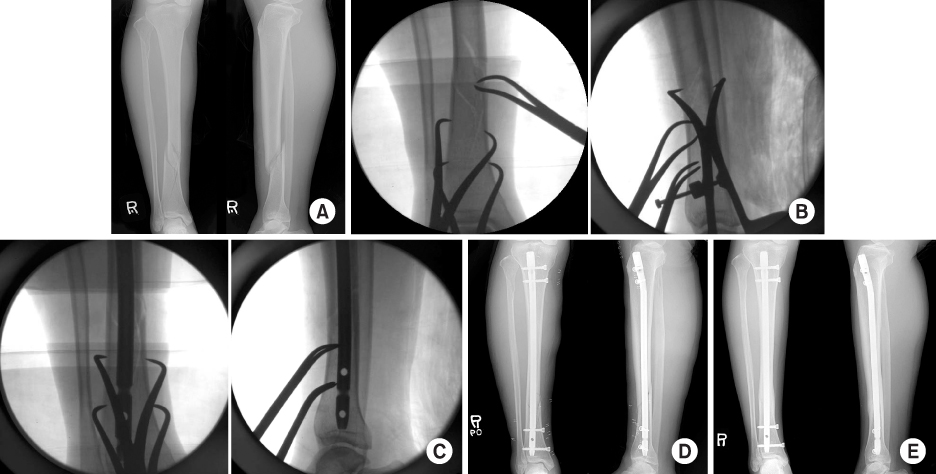
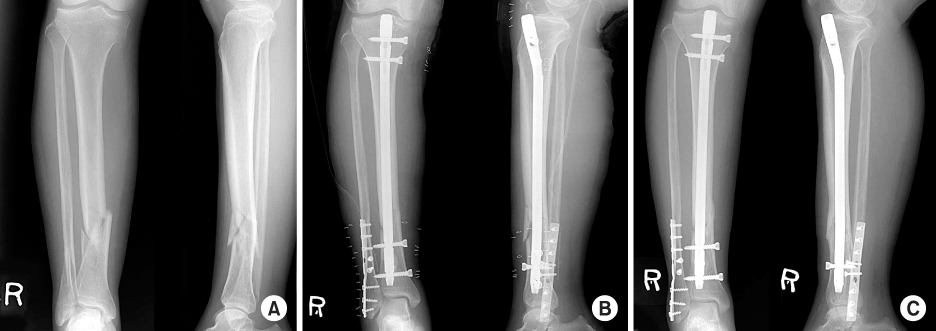
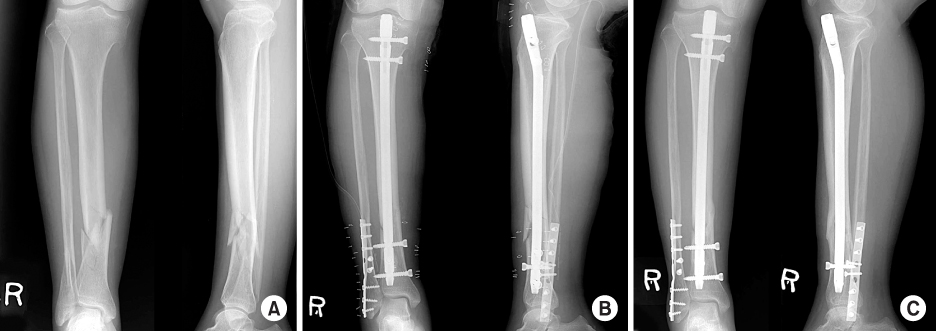
Fig. 1
Fig. 2
Fig. 3
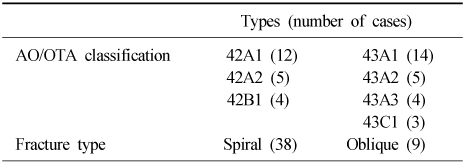
Fracture Type (AO/OTA Classification)
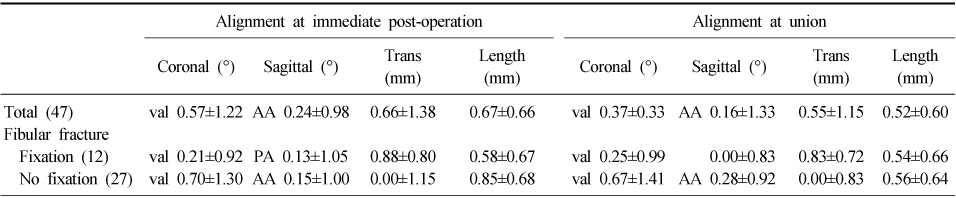
Summary of Results
Trans: Translation, Length: Lengthening, val: Valgus, AA: Anterior apical angulation, PA: Posterior apical angulation.
Trans: Translation, Length: Lengthening, val: Valgus, AA: Anterior apical angulation, PA: Posterior apical angulation.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

