Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 22(4); 2009 > Article
-
Review Article
- Distal Tibia Fracture: Plate Osteosynthesis
- Keun Bae Lee, M.D., Ph.D.
-
Journal of the Korean Fracture Society 2009;22(4):306-313.
DOI: https://doi.org/10.12671/jkfs.2009.22.4.306
Published online: October 30, 2009
Department of Orthopedic Surgery, Chonnam National University Medical School and Hospital, Gwangju, Korea.
- Address reprint requests to: Keun Bae Lee, M.D., Ph.D. Department of Orthopedic Surgery, Chonnam National University Medical School and Hospital, 8, Hak-dong, Dong-gu, Gwangju 501-757, Korea. Tel: 82-62-220-6336, Fax: 82-62-225-7794, kbleeos@chonnam.ac.kr
Copyright © 2009 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 745 Views
- 3 Download
- 4 Crossref
- 1. Arens S, Kraft C, Schleqel U, Printzen G, Perren SM, Hansis M. Susceptibility to local infection in biological internal fixation. Experimental study of open vs minimally plate osteosynthesis in rabbits. Arch Orthop Trauma Surg, 1999;119:82-85.
- 2. Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg, 2006;14:406-416.
- 3. Borg T, Larsson S, Lindsjö U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury, 2004;35:608-614.
- 4. Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res, 2000;375:69-77.
- 5. Foux A, Yeadon AJ, Uhthoff HK. Improved fracture healing with less rigid plates. A biomechanical study in dogs. Clin Orthop Relat Res, 1997;339:232-245.
- 6. Francois J, Vandeputte G, Verheyden F, Nelen G. Percutaneous plate fixation of fractures of the distal tibia. Acta Orthop Belg, 2004;70:148-154.
- 7. Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury, 2007;38:365-370.
- 8. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia-results in 20 patients. Injury, 2006;37:877-887.
- 9. Helfet DL, Shonnard PY, Levine D, Borrelli J Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury, 1997;28:A42-A47.
- 10. Helfet DL, Suk M. Minimally invasive percutaneous plate osteosynthesis of fractures of the distal tibia. Instr Course Lect, 2004;53:471-475.
- 11. Krackhardt T, Dilger J, Flesch I, Höntzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg, 2005;125:87-94.PDF
- 12. Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop, 2008;32:697-703.PDF
- 13. Maffulli N, Toms AD, McMurtie A, Olive F. Percutaneous plating of distal tibial fractures. Int Orthop, 2004;28:159-162.PDF
- 14. Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res, 2003;408:286-291.
- 15. Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury, 2004;35:615-620.
REFERENCES
Fig. 1
(A) A man was sustained distal tibia fracture with severe soft tissue swelling and blister.
(B) A temporary external fixator was applied to reduce the fracture and to maintain the length and alignment of the limb.
(C) A skeletal traction with calcaneal Steinmann pin was applied temporarily.
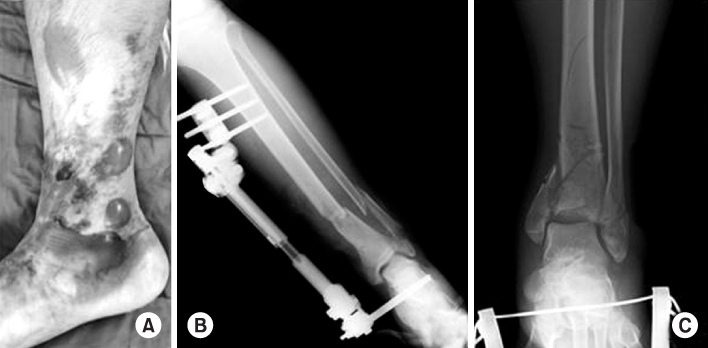
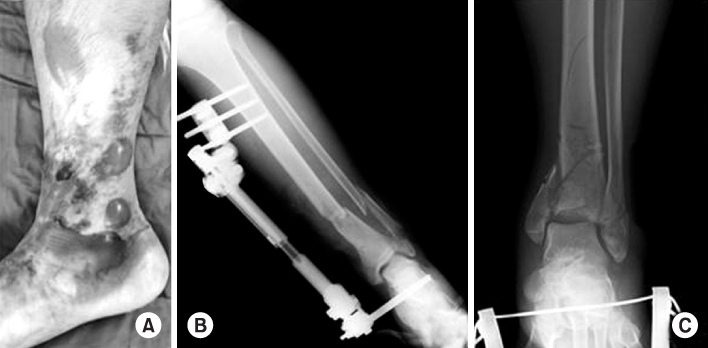
Fig. 2
(A) Medial and (B) anterolateral distal tibia locking plate (Synthes®, Zimmer®). (C) Application of periarticular distal tibia locking plate system (from Synthes®).
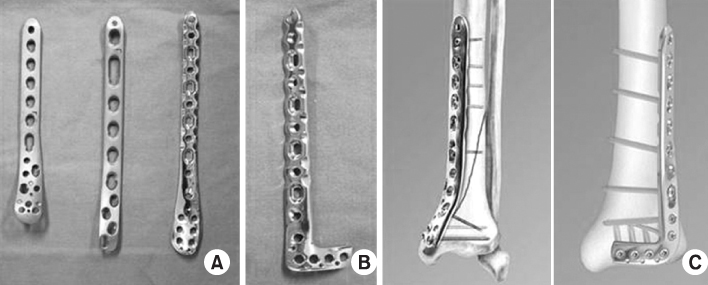
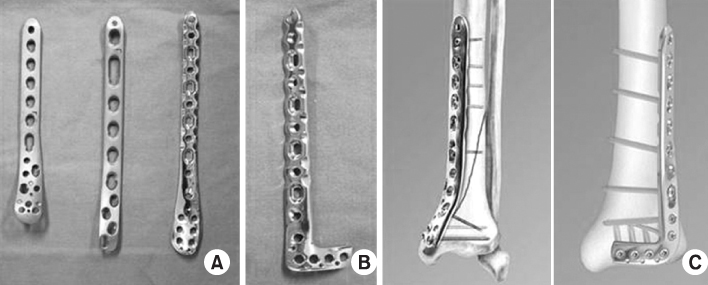
Fig. 3
(A) Apply femoral distractor to correct axial malalignment and to maintain the length. (B) First, fix the fibula taking care to restore length, alignment and rotation. Also, the fibula is fixed to increase the stability of the ankle fracture. (C) Directly reduce the fragment using pointed forcep. (D) Holding the fragment by pointed forcep, insert interfragmenary lag screw before plating. (E) An additional T-plate was applied through limited approaches to buttress a large metaphyseal defect.
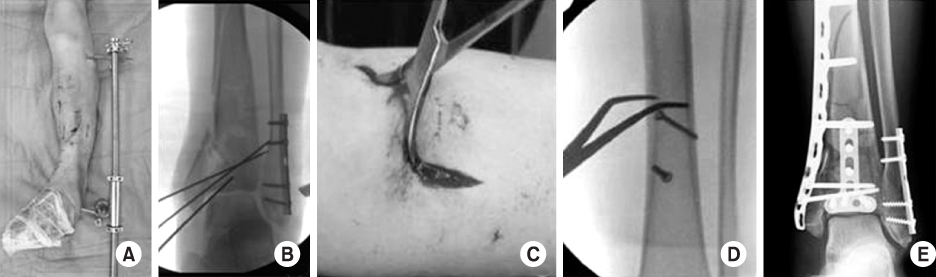
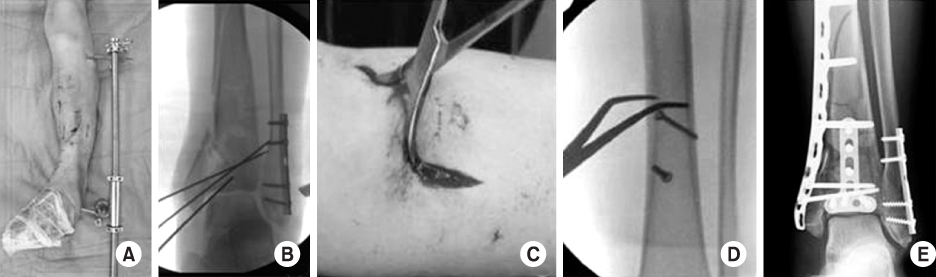
Fig. 4
(A, B) A 47 year-old man had distal tibia fracture. (C) Minimal skin incisions were shown proximally and distally on the medial side of tibia. (from AO surgery reference) (D, E) Minimally invasive percutaneous insertion of the LCP using drill sleeve on distal tibia. The location and size of plate, and the reduced fracture site was verified by fluoroscopy. (F) The compression screw can be used through the conventional hole for plate adjustment. (G) Interfragmentory lag screw was inserted under fluoroscopic guidance. (H) Skin incisions were determined minimally under fluoroscopic guidance for screw fixation. (I, J) 4 months after operation, the distal tibia fracture was achieved adequate reduction and bony union.
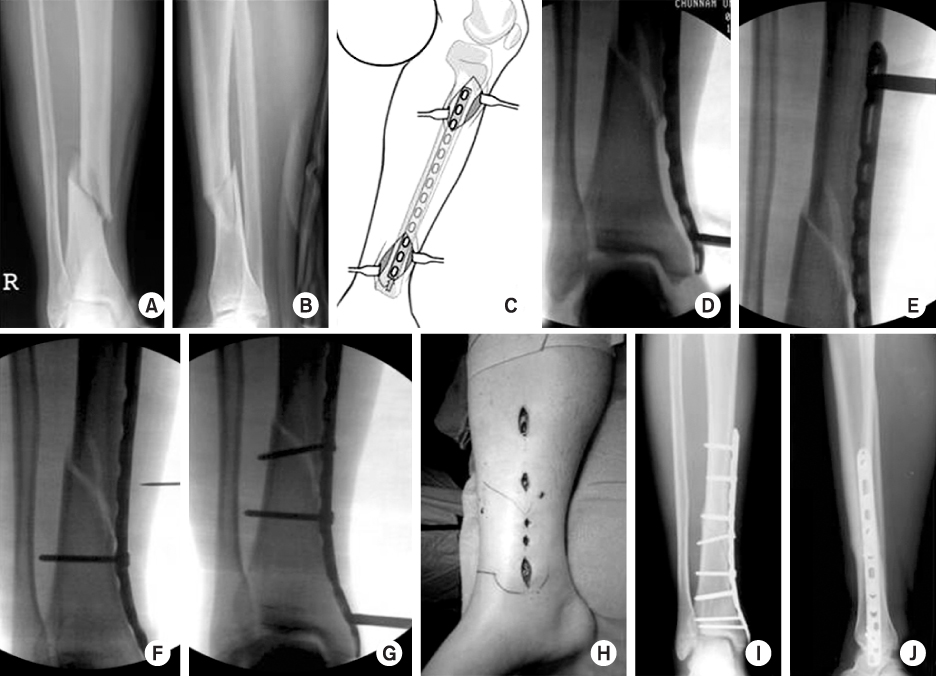
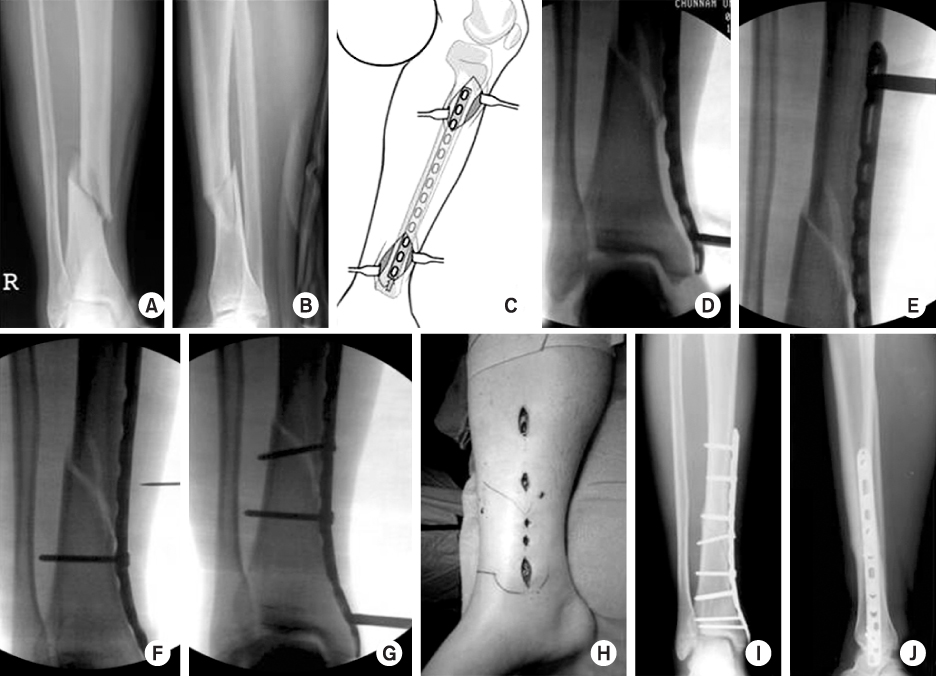
Fig. 6
(A, B) A 26 year-old man was stained distal tibia and fibular open fractures.
(C, D) A temporary external fixator was applied immediately to maintain the alignment due to severe soft tissue injury.
(E) The Vacuum Assisted Closure (VAC) device was used to facilitate wound healing by converting an open wound to a closed wound. 4 weeks after applying Wound VAC, granulation tissue was formed and wound was closed.
(F) Immediate postoperative x-ray, the distal tibia and fibular fracture achieved adequate reduction.
(G, H, I, J) The patient had a good bony union and clinical outcomes.


Fig. 7
(A, B) A 40 year-old man was sustained distal tibia comminuted fracture combined with distal tibiofibular joint comminution caused by falling down.
(C, D) Immediate operation was impossible due to medical comorbidity, so calcaneal traction was applied temporarily.
(E, F) The fracture was treated with percutaneous plating using LCP-MP on medial side at 2 weeks after injury.
(G) Clinical photo showed multiple minimal incisions intraoperatively.
(H, I, J) A successful union was achieved with a good functional outcome.


Fig. 8
(A) A 53 year-old man was sustained proximal and distal tibia open comminuted fractures by traffic accident.
(B, C) Spanning external fixator was applied immediately to maintain the alignment.
(D) The fractures were treated with MIPO using LCP-DTP on medial side at 3 weeks after injury.
(E) Delayed infection was developed at primary open site and plate was exposed at 2 months postoperatively.
(F) Patient underwent curettage and antibiotic bead insertion without plate removal.
(G, H, I) A successful union was achieved at 9 months postoperatively, with a good functional outcome.


Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Anterolateral Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures Using an Anterolateral Locking Plate
Dongwhan Suh, Hwan Hee Lee, Young Hoon Han, Jae Jung Jeong
Journal of Korean Foot and Ankle Society.2020; 24(1): 19. CrossRef - The Result of Using an Additional Mini-Locking Plate for Tibial Pilon Fractures
Suenghwan Jo, Jun Young Lee, Boseon Kim, Kang Hyeon Ryu
Journal of the Korean Fracture Society.2017; 30(2): 75. CrossRef - Minimally Invasive Plate Osteosynthesis for Fractures of Distal Tibia
Tae Hun Kim, So Hak Chung
Kosin Medical Journal.2014; 29(1): 23. CrossRef - Minimally Invasive Osteosynthesis with Locking Compression Plate for Distal Tibia Fractures
Sung-Kyu Kim, Keun-Bae Lee, Keun-Young Lim, Eun-Sun Moon
Journal of the Korean Fracture Society.2011; 24(1): 33. CrossRef
Distal Tibia Fracture: Plate Osteosynthesis

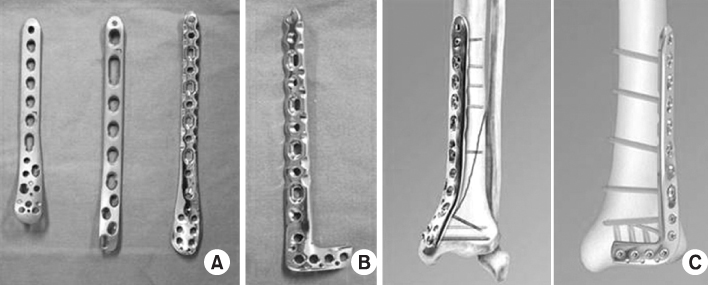
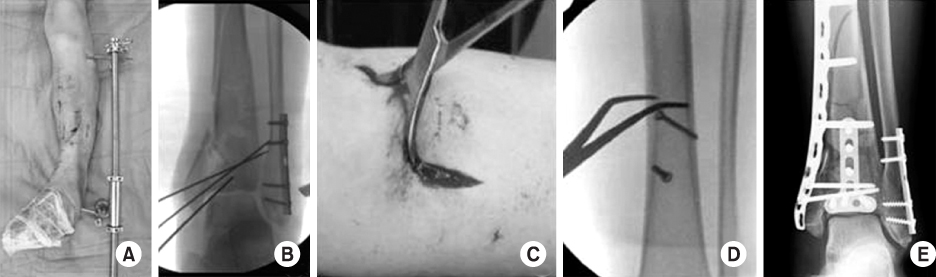
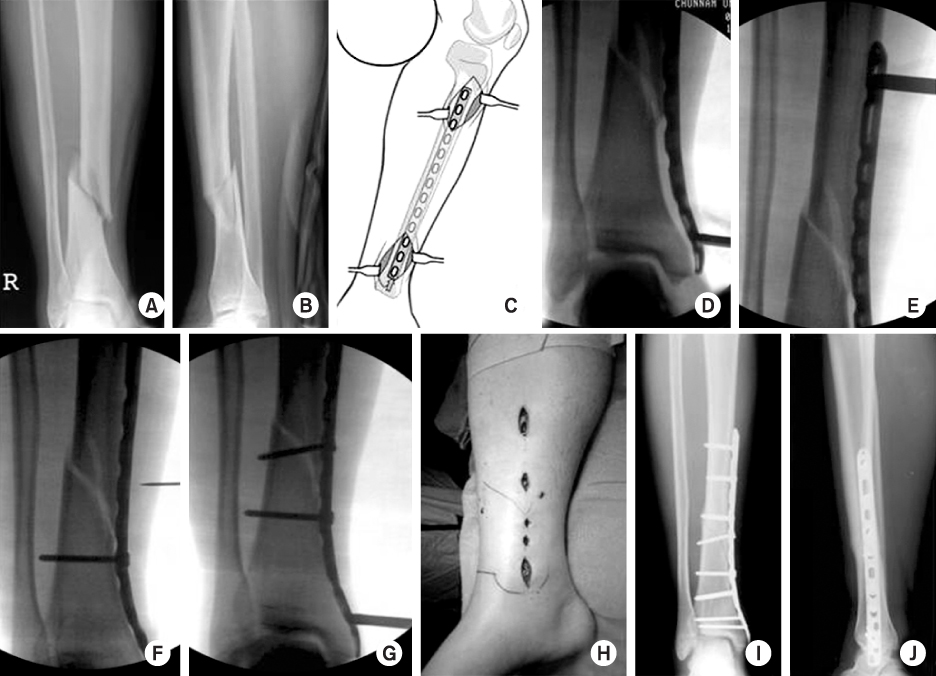




Fig. 1
(A) A man was sustained distal tibia fracture with severe soft tissue swelling and blister.
(B) A temporary external fixator was applied to reduce the fracture and to maintain the length and alignment of the limb.
(C) A skeletal traction with calcaneal Steinmann pin was applied temporarily.
Fig. 2
(A) Medial and (B) anterolateral distal tibia locking plate (Synthes®, Zimmer®). (C) Application of periarticular distal tibia locking plate system (from Synthes®).
Fig. 3
(A) Apply femoral distractor to correct axial malalignment and to maintain the length. (B) First, fix the fibula taking care to restore length, alignment and rotation. Also, the fibula is fixed to increase the stability of the ankle fracture. (C) Directly reduce the fragment using pointed forcep. (D) Holding the fragment by pointed forcep, insert interfragmenary lag screw before plating. (E) An additional T-plate was applied through limited approaches to buttress a large metaphyseal defect.
Fig. 4
(A, B) A 47 year-old man had distal tibia fracture. (C) Minimal skin incisions were shown proximally and distally on the medial side of tibia. (from AO surgery reference) (D, E) Minimally invasive percutaneous insertion of the LCP using drill sleeve on distal tibia. The location and size of plate, and the reduced fracture site was verified by fluoroscopy. (F) The compression screw can be used through the conventional hole for plate adjustment. (G) Interfragmentory lag screw was inserted under fluoroscopic guidance. (H) Skin incisions were determined minimally under fluoroscopic guidance for screw fixation. (I, J) 4 months after operation, the distal tibia fracture was achieved adequate reduction and bony union.
Fig. 5
Partial weight-bearing was permitted by applying Ankle-Foot-Orthosis.
Fig. 6
(A, B) A 26 year-old man was stained distal tibia and fibular open fractures.
(C, D) A temporary external fixator was applied immediately to maintain the alignment due to severe soft tissue injury.
(E) The Vacuum Assisted Closure (VAC) device was used to facilitate wound healing by converting an open wound to a closed wound. 4 weeks after applying Wound VAC, granulation tissue was formed and wound was closed.
(F) Immediate postoperative x-ray, the distal tibia and fibular fracture achieved adequate reduction.
(G, H, I, J) The patient had a good bony union and clinical outcomes.
Fig. 7
(A, B) A 40 year-old man was sustained distal tibia comminuted fracture combined with distal tibiofibular joint comminution caused by falling down.
(C, D) Immediate operation was impossible due to medical comorbidity, so calcaneal traction was applied temporarily.
(E, F) The fracture was treated with percutaneous plating using LCP-MP on medial side at 2 weeks after injury.
(G) Clinical photo showed multiple minimal incisions intraoperatively.
(H, I, J) A successful union was achieved with a good functional outcome.
Fig. 8
(A) A 53 year-old man was sustained proximal and distal tibia open comminuted fractures by traffic accident.
(B, C) Spanning external fixator was applied immediately to maintain the alignment.
(D) The fractures were treated with MIPO using LCP-DTP on medial side at 3 weeks after injury.
(E) Delayed infection was developed at primary open site and plate was exposed at 2 months postoperatively.
(F) Patient underwent curettage and antibiotic bead insertion without plate removal.
(G, H, I) A successful union was achieved at 9 months postoperatively, with a good functional outcome.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
Distal Tibia Fracture: Plate Osteosynthesis
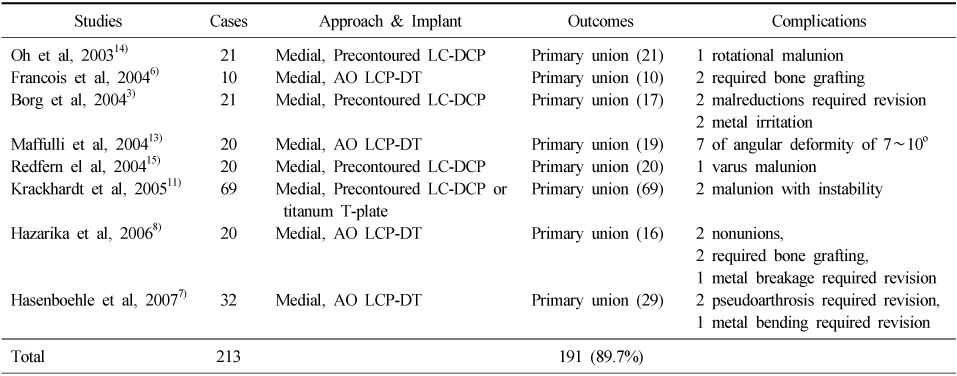
Literature reviews on outcomes and complications of MIPO for distal tibia fractures
Table 1
Literature reviews on outcomes and complications of MIPO for distal tibia fractures

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

