Search
- Page Path
- HOME > Search
Original Articles
- Correlation of bone mineral density with ankle fractures in older adults in Korea: a retrospective cohort study
- Seung Hyun Lee, Chae Hun Lee, Seo Jin Park, Jun Young Lee
- J Musculoskelet Trauma 2025;38(4):186-192. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00150
-
 Abstract
Abstract
 PDF
PDF - Background
Bone mineral density (BMD) is well-documented in relation to fractures of the spine, hip, distal radius, and proximal humerus; however, its correlations with other fracture types are less established. This study aimed to analyze BMD and associated risk factors in older adults (≥65 years of age) with osteoporotic ankle fractures. These fractures involve low-energy trauma, resulting from falls from a standing height or lower, and occur from impacts which typically do not cause fractures in individuals with normal bone.
Methods
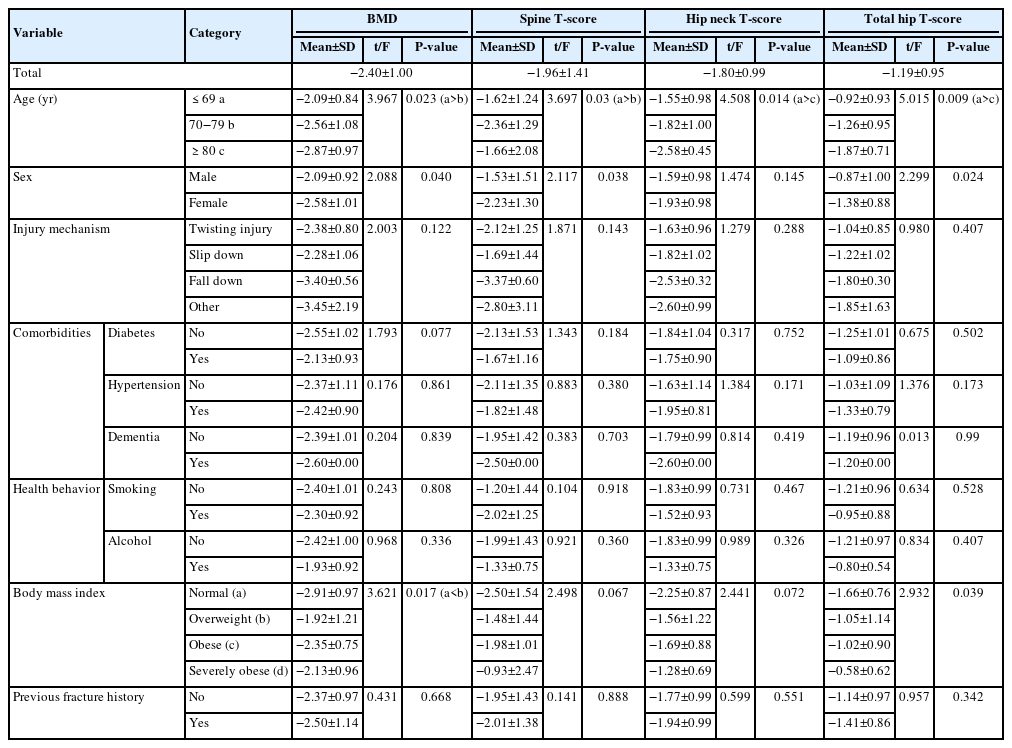
This retrospective study analyzed data from 1,411 patients diagnosed with ankle fractures admitted to Chosun University Hospital between February 2012 and April 2023. After applying inclusion criteria (age ≥65 years; low energy ankle fracture) and exclusion criteria (high energy trauma, open/multiple fractures, missing dual X-ray absorptiometry [DXA]), 73 of 1,411 patients were analyzed. Lumbar spine, femoral neck, and total hip T scores were obtained with a Horizon Wi DXA scanner, and associations with age, sex, mechanism of injury, comorbidities, smoking status, alcohol consumption, body mass index (BMI), and history of fractures were tested by ANOVA with Scheffe post hoc and Fisher exact tests.
Results
Lower BMD correlated significantly with older age, female sex, and lower BMI (P<0.05) in older adults with ankle fractures. No significant associations were observed for comorbidities (diabetes, hypertension, dementia), smoking, alcohol consumption, injury mechanism, or prior fractures.
Conclusion
These results indicate that older age, female, and lower BMI are linked to reduced BMD in ankle fracture patients over 65 years of age. Focused osteoporosis screening and management may therefore be most beneficial for older, low BMI women presenting with ankle fractures. Level of evidence: IV.
- 27 View
- 2 Download

- Correlation between Progression of Compression and Bone Densiometry Index in Osteoporotic Compression Fracture of Thoracolumbar Spine
- Jung Hoon Kim, Jeong Gook Seo, Jong Ho Ahn
- J Korean Fract Soc 2006;19(2):254-258. Published online April 30, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.2.254
-
 Abstract
Abstract
- PURPOSE
To evaluate whether progression of compression correlates with bone densiometry index in patients who were treated conservatively for osteoporotic compression fracture of thoracolumbar spine.
MATERIALS AND METHODS
Using the results of bone densiometry, 30 patients who were treated conservatively for osteoporotic compression fracture of thoracolumbar spine between March 2002 to March 2005 were categorized into 4 groups; above 80%, 70 to 80%, 60 to 70%, and below 60%. We compared the measurements of sagittal index and anterior vertebral height from the plain radiographs taken at the time of injury and following three consecutive months after the injury.
RESULTS
Patients with lower bone densiometry index had greater amount of compression at the time of injury and more rapid progression of compression. We also found that progression of compression was lowest during the first month after injury in all groups.
CONCLUSION
Patients with low bone densiometry index in osteoporotic thoracolumbar compression fracture are susceptible to more rapid progression of compression and should have early brace application and longer duration of treatment for osteoporosis. -
Citations
Citations to this article as recorded by- Comparison of Outcomes of Conservative Treatment, Early Vertebroplasty, and Delayed Vertebroplasty in Patients with Osteoporotic Vertebral Compression Fractures
Se-Hyuk Im, Young-Joon Ahn, Bo-Kyu Yang, Seung-Rim Yi, Ye-Hyun Lee, Ji-Eun Kwon, Jong-Min Kim
Journal of Korean Society of Spine Surgery.2016; 23(3): 139. CrossRef - Comparison of Outcomes of Conservative Treatment, Early Vertebroplasty, and Delayed Vertebroplasty in Patients with Osteoporotic Vertebral Compression Fractures
Se-Hyuk Im, Young-Joon Ahn, Bo-Kyu Yang, Seung-Rim Yi, Ye-Hyun Lee, Ji-Eun Kwon, Jong-Min Kim
Journal of Korean Society of Spine Surgery.2016; 23(3): 139. CrossRef - Progression of Compression and Related Factors in Conservative Management of Osteoporotic Vertebral Compression Fractures
Young Do Koh, Jeong Soo Park
Journal of the Korean Fracture Society.2015; 28(2): 132. CrossRef
- Comparison of Outcomes of Conservative Treatment, Early Vertebroplasty, and Delayed Vertebroplasty in Patients with Osteoporotic Vertebral Compression Fractures
- 357 View
- 0 Download
- 3 Crossref


 E-submission
E-submission KOTA
KOTA

 First
First Prev
Prev


