Lateral marginal fractures of the patella and patellofemoral pain
Article information
Abstract
Background
This study investigated the characteristics of lateral marginal fractures of the patella and evaluated the clinical outcomes.
Methods
We retrospectively reviewed all patients with lateral marginal fractures of the patella, defined as a vertical fracture line within 15 mm of the lateral patellar border, from 2008 to 2020. In total, 41 patients were included. Patient characteristics, radiologic findings, and clinical outcomes, including the Lysholm score at 1 year postoperation, were evaluated.
Results
The injury mechanisms were direct in 34 cases and indirect in seven. Furthermore, 85% of patients had a skyline view of the patella at the initial visit, and one medial subluxation of the patella was found. Forty of the 41 patients underwent surgery. Anatomical and nonanatomical (>1-mm displacement or excision) reductions were carried out in 36 cases (88%) and 5 cases (12%), respectively. The average Lysholm score was 89.1 (range, 67–99). The nonanatomical reduction group had a poorer functional score (79.8 vs. 90.4; P=0.010). Lateral patellar compression syndrome occurred in two patients with nonanatomical reduction.
Conclusions
Lateral marginal fractures of the patella affected patellofemoral stability. Anatomical reduction showed good functional outcomes, while nonanatomical reduction was associated with patellofemoral stability and pain. Therefore, surgeons should perform anatomical reduction with any appropriate fixation method.
Level of Evidence
IV
Introduction
Patellar fractures account for approximately 1% of all fractures and may result from direct or indirect injury mechanisms [1]. The indirect mechanism consists of direct blow to anterior knee from a fall or dashboard injury. Indirect forces with eccentric contraction of the quadriceps typically lead to transverse fractures [2]. In contrast, a direct blow more likely results in comminution, articular injury, anterior soft tissue damage, and open injury [2]. A vertical fracture pattern is not uncommon, and the fracture line is usually seen to involve the lateral facet and to lie between the middle and lateral third of the patella [3]. While Boström [1] reported that lateral avulsion was the most common mechanism in 75% of their patients, Dowd [4] reported that direct compression of the patella in a hyperflexed knee was responsible for this kind of fracture. However, there have been a few old reports about lateral marginal fractures of the patella; therefore, we attempted to investigate it based on our experience. This study aimed to define the characteristics of lateral marginal fractures of the patella and evaluate their clinical outcomes. Given the potential impact of reduction quality on patellofemoral mechanics and pain, we hypothesized that anatomical reduction would lead to better functional outcomes compared to nonanatomical reduction. This study further seeks to provide clinically relevant insights to guide optimal surgical management of these rare fractures.
Methods
Ethics Statement
The study was approved by the Institutional Review Board (IRB) of Asan Medical Center (IRB No. 2020-1075) and performed in accordance with the principles of the Declaration of Helsinki. The need for written informed consent was waived because of its retrospective design by the IRB.
We retrospectively reviewed all patients with lateral marginal fractures of the patella in two level I trauma centers from January 2008 to December 2020. A lateral marginal fracture was defined as a longitudinal lateral facet fracture with a fracture line within 15 mm of the lateral patellar border, based on consistent patterns observed in our patient cohort and anatomical considerations related to the lateral facet width. This operational definition was used to distinguish lateral marginal fractures from more central vertical or transverse fractures. The exclusion criteria were fracture with additional transverse component, periprosthetic fractures, and less than 1 year of follow-up.
During the period, a total of 1,131 patellar fractures were screened, and 145 (12.8%) were classified into AO/OTA type B1 (lateral vertical fracture) using computed tomography (CT) images. Moreover, 47 lateral marginal fractures (4.2%) were enrolled, but six patients were excluded because of less than 1 year of follow-up. Finally, 41 patients (31 male and 10 female) were included in the study with an average age of 46.6 years (range, 21–82 years). The average follow-up was 20.5 months (range, 12–52 months). The choice of surgical method was based on fragment size and comminution. Screw fixation was used for adequately sized fragments, tension band wiring (TBW) for smaller or comminuted fragments, and hook plating for selected avulsion-type fractures [5,6]. Patient characteristics and fracture pattern included injury mechanism, open fracture, comminution, distance from the lateral border to the fracture site, initial displacement, and patellar subluxation and treatment method, complication, and functional outcomes. Complications included infection, malunion, and secondary interventions due to persistent pain. The functional outcomes were evaluated with the Lysholm score at 1 year postoperatively.
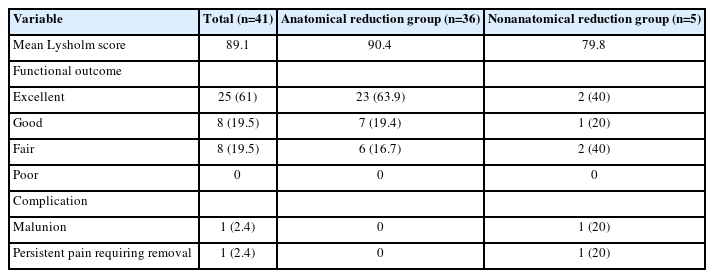
The clinical outcomes were compared between the anatomical and nonanatomical reduction groups (Table 1). The nonanatomical group was defined as having >1-mm displacement or excision of the fragment. Statistical analysis was performed using IBM SPSS ver. 21.0 (IBM Corp.). Dichotomous data were compared using Fisher exact test, while the independent t-test and Mann-Whitney test were used for the comparison of parametric and nonparametric data, respectively. Statistical significance was set at P<0.05.
Results
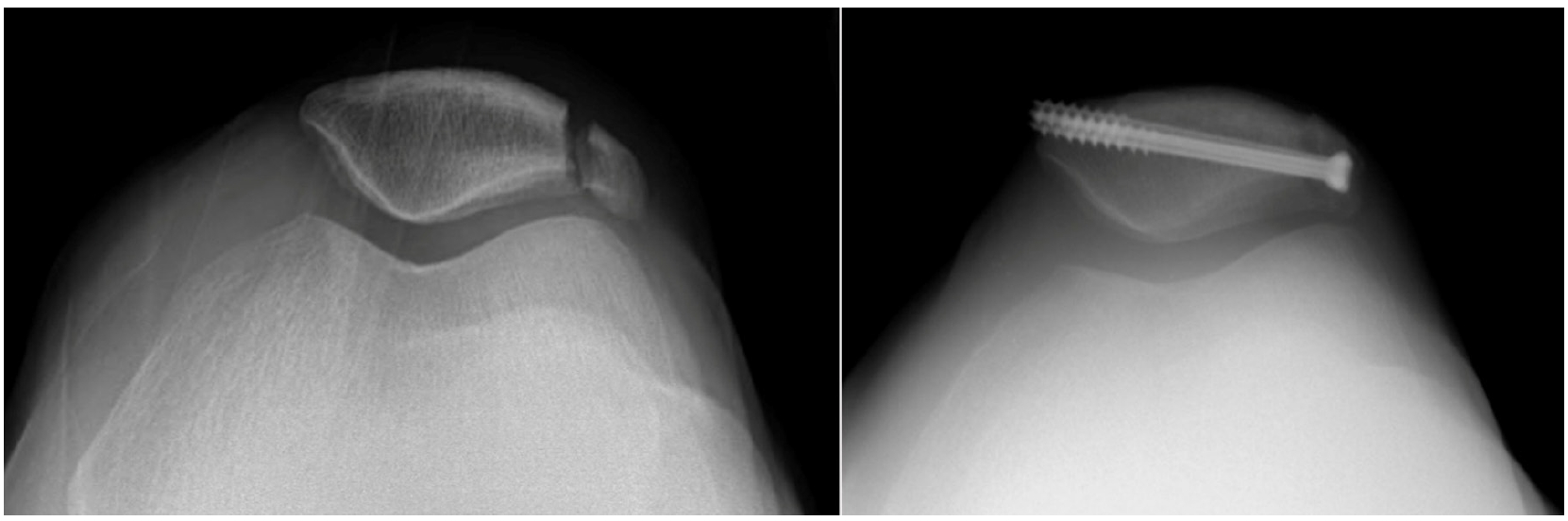
The injury mechanisms included 34 direct injuries (82.9%) and seven indirect injuries (17.1%). Three patients (7.3%) had open fractures, and 11 (26.8%) had comminuted fractures. The average distance from the lateral border of the patella to the fracture site was 9.9 mm (range, 3–15 mm), and the average displacement was 2.9 mm (range, 2–16 mm). Furthermore, 85% of the patients had the skyline view of the patella at the initial visit, and there was one case of medial patellar subluxation (Fig. 1).
Lateral marginal fracture with a small fragment. (A) Right knee anteroposterior and lateral views showing no definite fracture. (B) Skyline view revealing medial subluxation of the patella. (C) Knee computed tomography showing a small lateral fragment. (D) Hook plating. (E) Postoperative 1-year X-ray showing union, with a Lysholm score of 94.
Surgical treatment was performed in all patients, except one. The surgical methods were as follows: 24 cases, screw fixation (Fig. 2); eight, screw fixation combined with TBW; four, TBW; three, fragment removal and retinaculum repair; and one, hook plating (Fig. 1). In one patient with conservative treatment, knee X-ray did not show a fracture, and further evaluation was delayed because he was intubated and cared for in the intensive care unit for polytrauma with small bowel perforation, left clavicle shaft fracture, and mandible open fracture (Fig. 3). One month after injury, he complained of persistent right knee pain, and magnetic resonance imaging (MRI) and CT revealed a lateral marginal fracture.
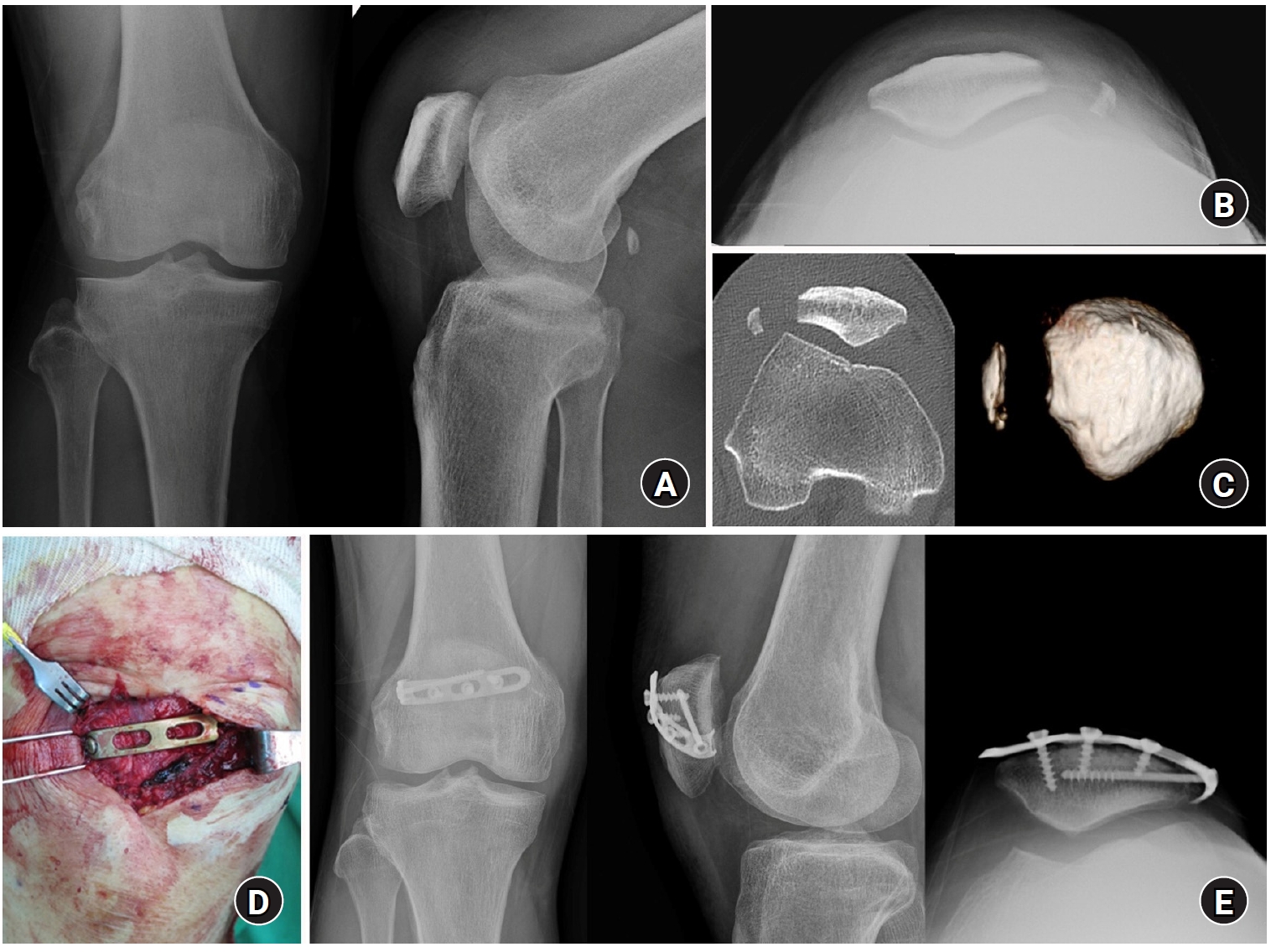
A 39-year-old male patient. (A) Initial X-ray showing no definite fracture. (B) Computed tomography performed 1 month after injury revealed a tiny fragment at the lateral border of the patella. (C) Postoperative 1-year anteroposterior and lateral views. (D) Skyline view showing the remaining fragment at the lateral border and 12° tilt of the patella, with a Lysholm score of 67.
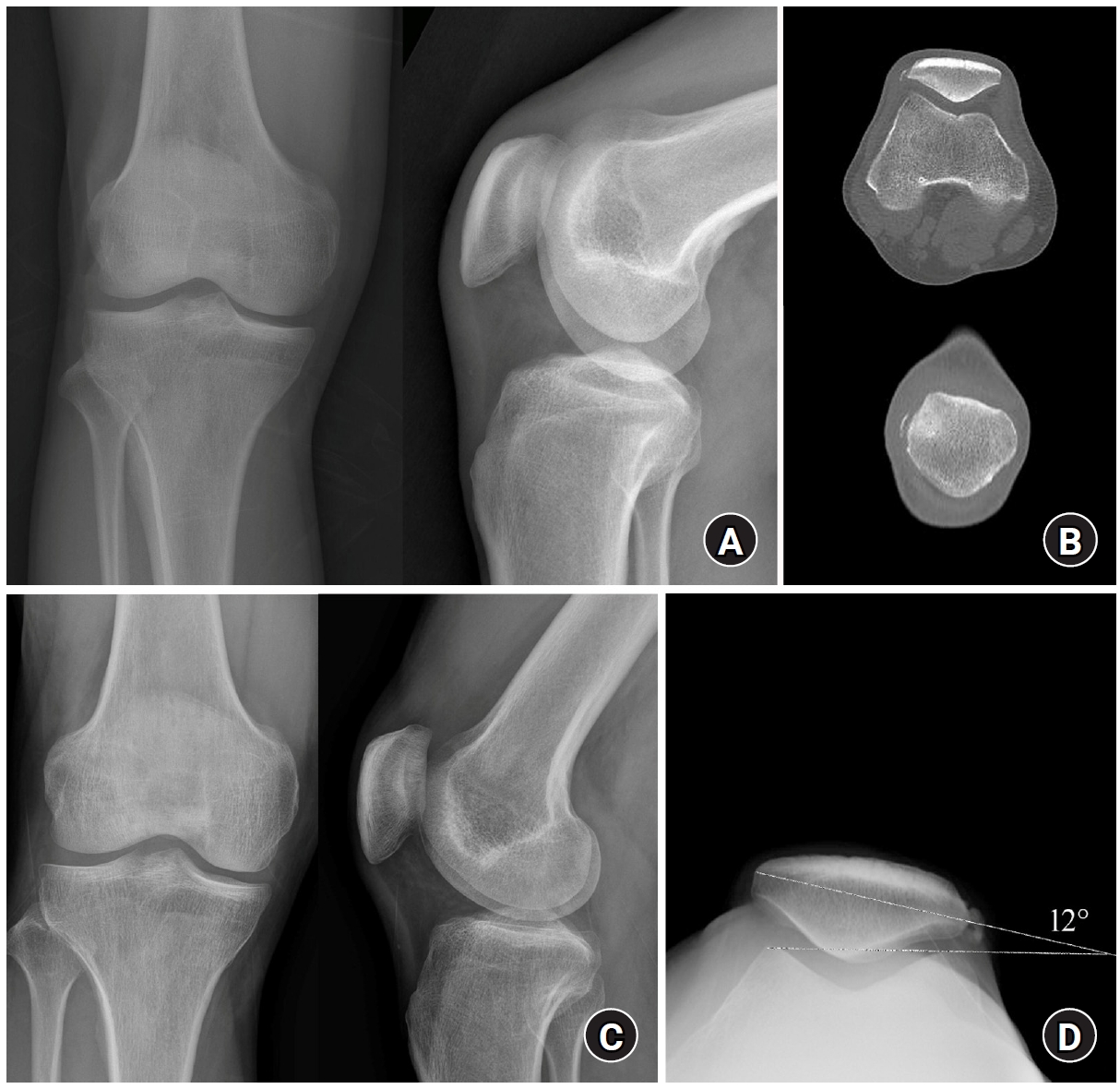
Anatomical reduction was acquired in 36 cases (88%), but there were five cases (12%) involving nonanatomical reduction (>1-mm displacement and excision of fragment). All cases with internal fixation acquired bone union without complications, including infection. The average Lysholm score was 89.1 (range, 67–99): 25 cases (61%), excellent (>90); eight cases (19.5%), good (84–90); eight cases (19.5%), fair (65–83); and 0 case, poor (<65). The nonanatomical reduction group had a poorer functional score (79.8 vs. 90.4; P=0.010). There were five patients in this group: one patient received conservative treatment, another underwent screw fixation, and the others underwent excision. Two cases (40%) of complications were noted, involving malunion and persistent pain that required implant removal. The patient treated by screw fixation had malunion with a laterally displaced fragment and complained of persistent anterior knee pain (Fig. 4). Reoperation for removal was performed, but the pain was persistent. Follow-up knee X-ray after removal showed a 21° lateral tilt of the patella with a “comma sign,” and bone single-photon emission CT findings evidenced the patellofemoral pain. The patient who was managed conservatively also had persistent anterior knee pain with tenderness along the lateral patellar border with a 12° lateral tilt of the patella (Fig. 3). The cause of pain in these two patients was considered as “lateral patellar compression syndrome.”
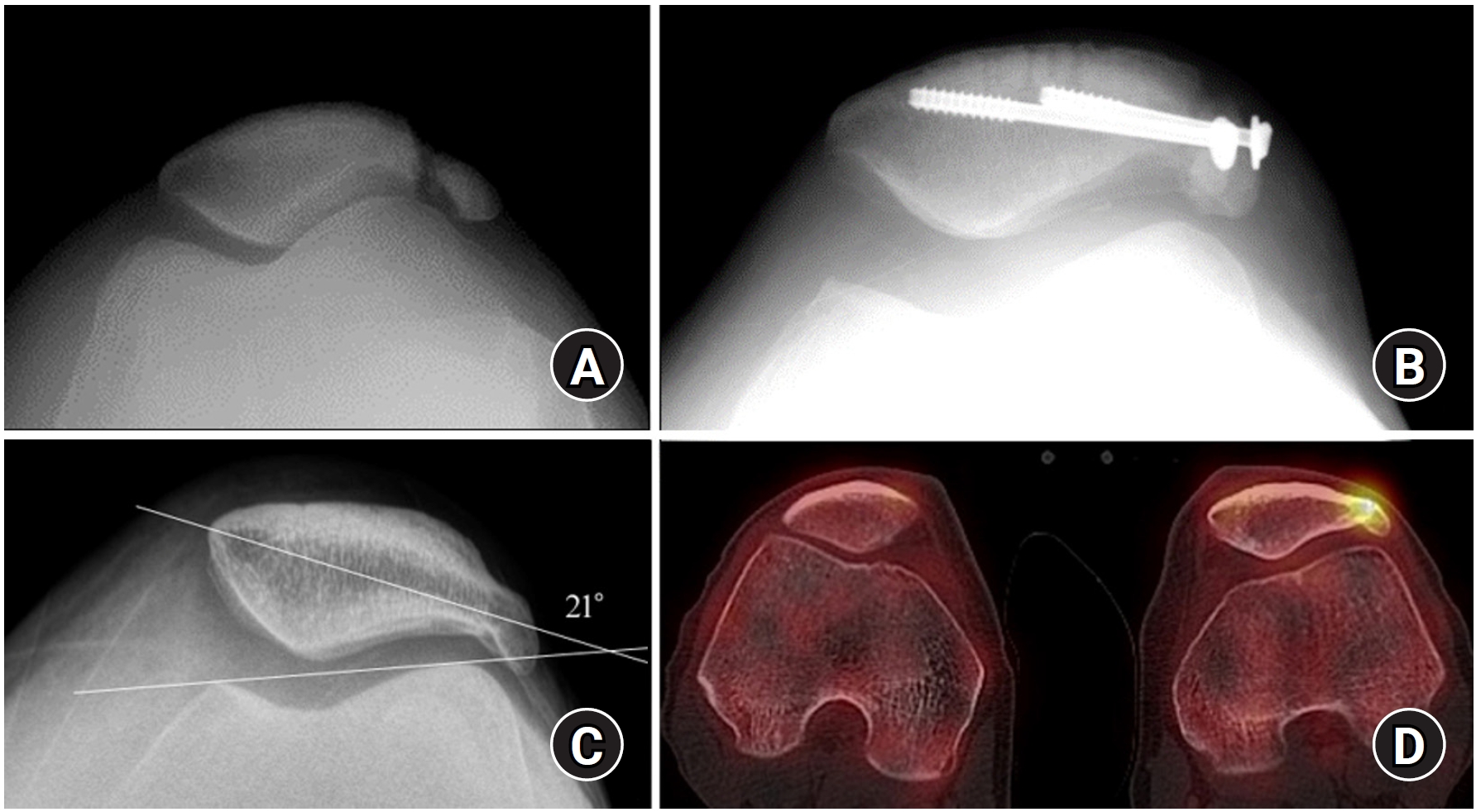
A 41-year-old male patient. (A) Lateral marginal fracture of the left patella. (B) Displaced fragment after screw fixation. (C) Skyline view showing malunion of the lateral patella and 21° lateral tilt. (D) Bone single-photon emission computed tomography revealing hot uptake at the lateral fragment.
Discussion
The current study revealed that lateral marginal fractures of the patella were uncommon (4.2%) and most of them (82.9%) were caused by a direct injury. A direct injury to the patella increased the compression force and resulted in a vertical fracture. As the direct force is significantly increasing, the patella would indent the lateral femoral condyle. The history of injury in the current study would support this injury mechanism. An indirect injury on the patella also led to lateral marginal fractures caused by sudden excessive muscle pull compressing the patella onto the lateral femoral condyle, which acted as a fulcrum while the knee was flexed [7]. Another rare pattern is stress fracture (not observed in the current study) caused by middle-distance running or weightlifting, in which strong and repetitive the quadriceps contractions during flexion angles between 20° and 90° could induce compression of the lateral articular facet against the lateral femoral condyle [8,9].
The patellar marginal fractures are uncommon injuries compared with other types [10,11]. The marginal fractures are potentially more common than supposed because it often remain undiagnosed as acute injuries [4]. This fracture often leads to less acute disability than a stellate or transverse fracture, and plain radiographs are often unhelpful. In the present study, most of the patients were diagnosed at initial visit, but the diagnosis of one case (2.4%) was delayed 1 month after injury, which was a special case because of unavailability of conversation with the patient and no definite fracture in initial X-ray. However, CT or MRI has been currently performed for patients with knee trauma, and would be helpful to detect marginal fractures [12,13].
In the radiographic review, we found two significant findings: medial patellar subluxation (Fig. 1) and lateral tilt with bone fragment/ossifying tissue along the lateral border of the patella (Figs. 3 and 4). The abnormalities of dynamic muscle strength (vastus medialis obliquus) and static soft tissue restraint (lateral retinaculum) have profound effects on patellofemoral kinematics and may lead to clinical dysfunction [14]. Medial subluxation is uncommon and usually seen after a lateral release surgical procedure [15]. However, as shown in Fig. 1, displaced or inappropriately reduced lateral marginal fracture would lead to medial subluxation. Medial subluxation or dislocation causes patellofemoral pain syndrome [16], and appropriate reduction should be achieved to restore soft tissue tension. Another problem is the “lateral tilt of the patella with ossifying tissue.” The newly developed tissue results in aberrant anatomy and ultimately biomechanical abnormalities [14]. The lateral retinaculum also plays an important role in patellofemoral pain syndrome [16]. Injury to the lateral retinaculum, particularly when accompanied by lateral ossifying tissue or a displaced fragment, may result in fibrotic changes and nerve entrapment within the retinaculum. This neuropathic alteration resembles the histopathological features of a Morton neuroma, characterized by perineural fibrosis and nerve irritation [17]. A tilt angle between 0° and 5° is normal, that between 5° and 10° is borderline, and an angle greater than 10° is considered abnormal. In addition, an abnormal tilt was detected in 85% of patients experiencing malalignment pain [18]. It seemed to be a kind of “lateral patellar compression syndrome,” which is associated with overload and increased pressure on the lateral facet due to pathologic lateral soft tissue restraints [19]. As shown in Figs. 3 and 4, failure to diagnose or restore marginal fracture of the patella may result in the disability of the knee and potential degenerative changes in the patellofemoral joint.
The current study demonstrated that the postoperative reduction state was related to the functional outcomes. Generally, surgical indications were articular step-off ≥ 1–2 mm and the displacement of articular fragment ≥2–3 mm with the loss of active knee extension [20]. The goals of treatment were as follows: (1) restoration of the extensor mechanism and (2) maintenance of a congruous articular surface [21]. Lateral marginal fractures mainly involve a vertical component and a well-preserved extensor mechanism but are commonly related to articular step-off or displacement. When the reduction was anatomical, the functional outcome was good, while patellofemoral pain, sometimes associated with lateral patellar compression syndrome in the case of failure of reduction, was observed to worsen function. Therefore, such fractures should be managed focusing on anatomical reduction.
The main surgical method was screw fixation, which was useful to secure the fragment firmly but had limitation to small fragment (Fig. 4). For the small fragments, TBW was used in combination or isolation. It is challenging to fix comminuted small fragments, in which excision was one option, and hook plating has been introduced recently for the avulsion fragment [6]. There were several studies about the clinical outcomes of patellar fractures but few results about marginal fracture except inferior pole fractures [6,22,23]. Therefore, further studies about the fixation method and its outcomes are needed.
The limitations of this study include its retrospective nature and the small number of cases. However, the participants were enrolled from a large cohort of 1,131 patellar fractures. Considering the rarity of these fractures, the study findings could be meaningful, even with the small number of cases. In addition, a potential bias may be present because the surgeries were performed at different centers. To overcome this kind of bias, a standard surgical procedure based on basic fracture principles was performed. Despite these limitations, this is a unique study about lateral marginal fractures of the patella and related clinical characteristics.
Conclusions
Lateral marginal fractures of the patella are uncommon injuries, most often caused by direct trauma. These fractures can affect patellofemoral stability and lead to anterior knee pain. In this study, anatomical reduction was associated with better functional outcomes, while nonanatomical reduction was linked to persistent pain. Therefore, we recommend that surgeons should perform anatomical reduction with any fixation method.
Notes
Author contribution
Conceptualization: JAS, CHK, JWK. Data curation: JAS, CHK, JWK. Formal analysis: JAS, CHK, JWK. Investigation: JAS, JWK. Methodology: JAS, JWK. Project administration: CHK, JWK. Resources: CHK, JWK. Software: CHK. Supervision: CHK, JWK. Validation: CHK, JWK. Visualization: CHK. Writing-original draft: JAS. Writing-review & editing: CHK, JWK. All authors read and approved the final manuscript.
Conflict of interests
Ji Wan Kim is a deputy editor of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Funding
None.
Data availability
Contact the corresponding author for data availability.