Principles for Management of Periprosthetic Acetabular Fractures after Hip Arthroplasty
Article information
Abstract
Abstract
Periprosthetic acetabular fracture (PAF) is an uncommon complication following hip arthroplasty. However, as the number of people needing hip prostheses continues to rise, the absolute number of PAF is expected to increase as well. These fractures may occur either intraoperatively or postoperatively. Postoperative fractures can be caused by traumatic events or by pathologic conditions related to periacetabular osteolysis. The management of PAF usually depends on the degree of displacement and the stability of the acetabular component. While most of non-displaced fractures can be managed non-operatively by protected weight bearing, displaced fractures with unstable implants require surgical intervention, which is often technically challenging. This review summarized the latest findings on the epidemiology, the diagnosis, the classification, and the treatment of PAF.

(A) A 55-year-old female underwent total hip arthroplasty due to rheumatoid arthritis on her left hip. (B) Fractures on the superior and inferior ramus were found after the patient suffered a minor trauma at 8 months postoperatively. Arrows indicate pubic rami fractures. (C) The fractures were healed after 6 months with conservative management. The acetabular component was stable without pain.

(A) Postoperative radiograph of a 52-year-old female with developmental dysplasia of the hip. (B) Non-displaced fracture of the posterior column was observed in the Lowenstein lateral radiograph at 2 months postoperatively. An arrow indicates posterior column fracture. (C) The fracture was healed with callus formation after 4 months of protected weight-bearing.

(A) A 55-year-old female with secondary osteoarthritis due to tuberculosis sequelae underwent total hip arthroplasty. (B) Eighteen-year postoperative radiograph showed severe osteolytic lesions around the acetabular cup and proximal stem. A minor traumatic event caused periprosthetic acetabular and greater trochanteric fractures. (C-E) The corresponding computed tomography scan indicated pelvic discontinuity caused by a transverse acetabular fracture. Arrows indicate fracture lines causing pelvic discontinuity. (F, G) Massive impaction bone grafting was performed, followed by acetabular revision using a 64-mm jumbo cup with multiple screw holes.
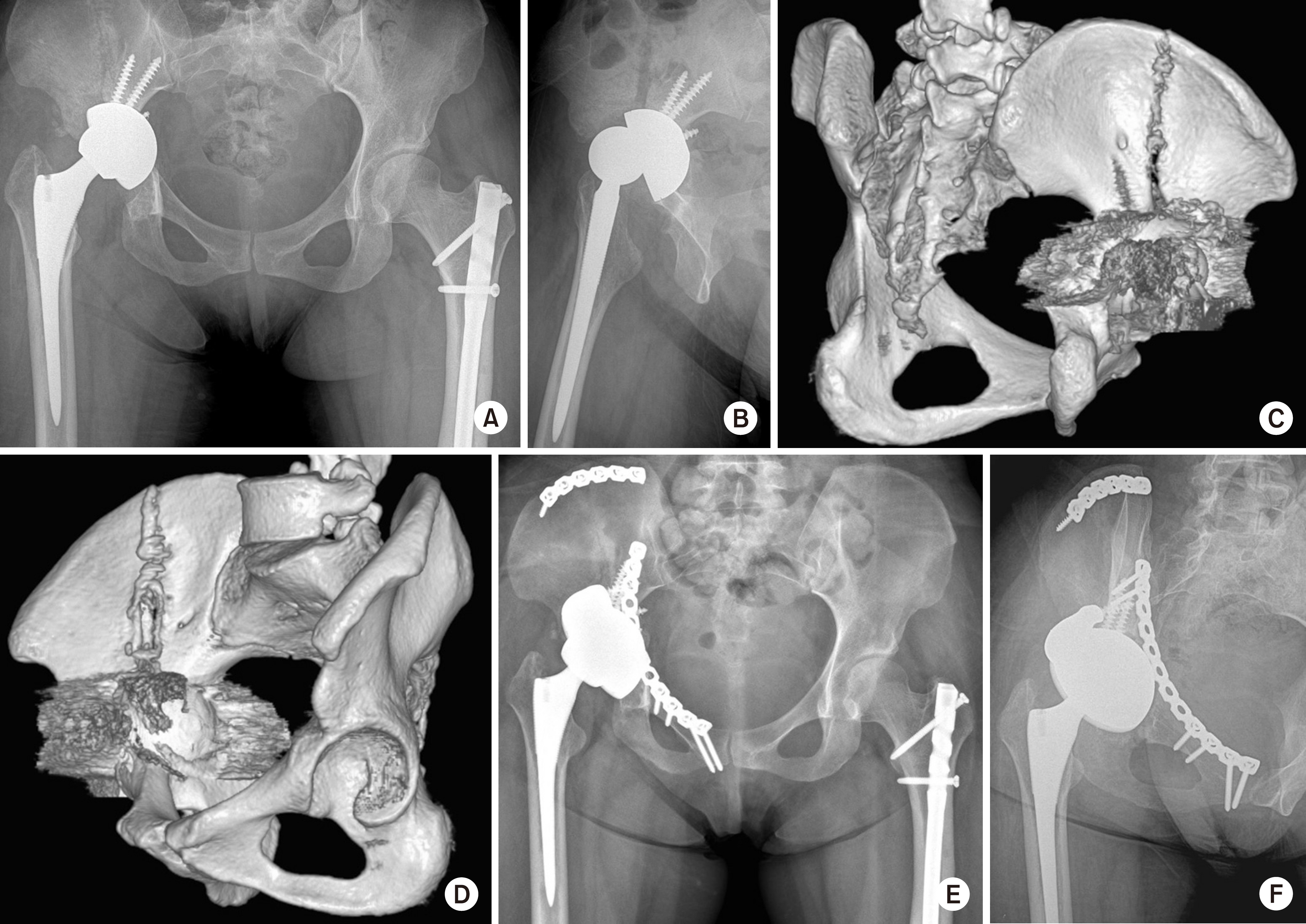
(A, B) The acetabular prosthesis became unstable due to a traumatic periprosthetic acetabular fracture. (C, D) The three-dimensional reconstruction images showed a displaced acetabular fracture involving both columns and the iliac wing. (E, F) After removing the previous prosthesis, the fracture was treated by open reduction and internal fixation with two reconstruction plates. The acetabular component was revised with the help of tantalum metal block and additional screws. Three-month postoperative radiographs showed stable implant fixations.

(A, B) Preoperative radiographs showing a displaced acetabular fracture with the protrusion of the bipolar cup into the pelvic cavity. (C, D) Computed tomography images showed comminuted fracture of the medial wall of the acetabulum. (E) The displaced quadrilateral surface was visualized through the modified Stoppa approach. (F-H) After open reduction of depressed articular surface of the acetabulum, buttress plating was performed using reconstruction plates and screws. (I, J) Five-month postoperative radiographs showed the stable bipolar component in the congruent hip joint.

